Abstract
Children with autism spectrum disorder (ASD) often exhibit challenging behaviors. Existing behavioral parent trainings (BPT) address ASD symptomology, but are lengthy and associated with significant attrition. In the current pilot study, a longitudinal randomized controlled trial was used to evaluate a novel brief BPT targeting caregivers of children with ASD ages 5–9. The 6-session BPT, delivered in a group format, focused on high-frequency challenging behaviors (e.g., problem behaviors, feeding and sleep issues). Caregivers who received BPT (n = 29), relative to an active control (psychoeducation/supportive therapy; n = 9), reported higher treatment satisfaction and acceptability. Challenging behaviors were reduced in the BPT and active control groups. The novel BPT was a feasible and acceptable intervention to target challenging behaviors in youth with ASD.
Similar content being viewed by others
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by social communication deficits, restricted interests, and repetitive patterns of behavior (American Psychiatric Association, 2013). Autistic individuals are at risk for emotional and behavioral problems in early childhood that often persist across time (Simonoff et al., 2008). Challenging behaviors such as aggression, disruption, and self-injurious behavior are common, and have been estimated to occur in over half of children with ASD (Maskey et al., 2013; Matson et al., 2008). Additionally, children with ASD often present with challenging behaviors related to feeding and sleeping. Gastrointestinal disorders commonly co-occur (Yang et al., 2018) and food selectivity, food refusal, and rapid-eating were found in over 75% of a sample of 136 children with ASD. An estimated 50–80% of children with ASD display sleep disturbances such as insomnia, problematic bedtime routines, short sleep cycles, early waking, nightmares, and associated daytime sleepiness (Reynolds & Malow, 2011; Richdale & Schreck, 2009). None of these challenging behaviors are diagnostic features of ASD, yet are all prevalent and associated with poor psychosocial and educational outcomes, and increased risk of institutionalization in the ASD population (Fitzpatrick et al., 2016).
Relatedly, caregivers of children with ASD experience higher levels of stress, anxiety, and depression than both caregivers of typically developing children and caregivers of individuals with other developmental disabilities (Hayes & Watson, 2013). Moreover, caregiver stress and mental-health symptoms are exacerbated when a child with ASD also engages in challenging behavior (Argumedes et al., 2018; Lecavalier et al., 2006; McStay et al., 2014). This relationship between caregiver stress and challenging behavior in children with ASD is bidirectional (Neece et al., 2012), with reductions in caregiver stress associated with behavioral improvements in the child (Estes et al., 2019; Singh et al., 2014). Similarly, challenging behavior is often learned and maintained by socially mediated consequences delivered by the caregivers (Beavers et al., 2013). Thus, modifying child challenging behavior often necessitates caregivers adjusting their own behaviors (Karst & Van Hecke, 2012).
Behavioral parent training (BPT) programs are a type of intervention that teaches caregivers effective skills to help manage their child’s needs. BPT can engender change in caregiver behavior, significantly increase caregiver feelings of self-efficacy, and reduce caregiver stress (Bearss et al., 2015; Miyajima et al., 2017; Schrott et al., 2019; Sharp et al., 2014; Tellegen & Sanders, 2014). A widely implemented evidence-based BPT group intervention, Incredible Years (IY), offers the Incredible Years Autism Spectrum and Language Delays Parent Program (IY-ASLD; Dababnah & Parish, 2016). The IY-ASLD consists of 14–16 group sessions and utilizes a series of video vignettes and structured activities to cover a variety of topics, such as using praise and rewards, setting limits, and promoting academic, emotional, and social skills (Dababnah & Parish, 2016; Williams et al., 2020). Pilot studies and a randomized control trial (RCT) of the IY-ASLD revealed high caregiver satisfaction with the program and a significant increase in pro-social skills in their children with ASD (Dababnah & Parish, 2016; Williams et al., 2020). However, IY-ASLD does not directly target several of the more frequent challenging behaviors displayed by individuals’ with ASD (e.g., agression, feeding issues, sleep disturbance).
In addition to IY-ASLD, Bearss et al. (2013) conducted an initial pilot study of a BPT specifically targeting challenging behavior in children with ASD. The Research Units on Pediatric Psychopharmacology Autism Network Parent Training (RUPP PT) program consisted of 11 core sessions, 7 optional sessions, 2 home visits, and 3 booster sessions over the course of 16 weeks. Behavior management techniques, such as reinforcement strategies and planned ignoring, were taught in the core sessions, and specific challenging behaviors (e.g., toileting, sleeping, feeding) were covered in the optional sessions. The 2013 pilot study indicated feasibility of the RUPP PT, with 87% of the families completing treatment and caregiver rated decreases in child disruptive behavior. Bearss et al. (2015) conducted a follow-up RCT comparing the efficacy of a 24-week Research Units in Behavioral Intervention (RUBI) parent training intervention to psychoeducation for reducing a wide range of challenging behaviors (e.g., tantrums, noncompliance). Compared to psychoeducation, the RUBI intervention was more efficacious in reducing disruptive behaviors in children with ASD. Although there were supplemental sessions targeting other high-frequency challenging behaviors (e.g., feeding and sleeping issues), analyses and outcomes mainly focused on the effect on disruptive behaviors. Thus, it is unclear to what extent the intervention meaningfully impacted participants feeding and sleeping challenging behaviors.
BPTs that target only feeding challenges exist, and the efficacy evaluations of these interventions suggest that they are superior to general parent trainings in improving feeding challenges (Johnson et al., 2019; Miyajima et al., 2017; Sharp et al., 2014, 2019). Regarding sleep disturbances in ASD, no extant studies have evaluated a BPT specifically designed for sleep; although, there is preliminary evidence that the incorporation of parent training in sleep interventions may improve sleep quality for children with ASD (Kirkpatrick et al., 2019).
The risk for emotional and behavioral problems and associated psychosocial and educational impairments, coupled with the increasing number of children diagnosed with ASD (e.g., 1 in 44 children; Maenner, 2021), have resulted in an increased need for efficacious interventions. Because there are often long waitlists to access individual treatment services, BPTs administered in a group setting may maximize treatment availability, access, and ultimately engagement (Gordon-Lipkin et al., 2016). For example, waitlists may be reduced by delivering services to multiple caregivers simultaneously reducing the need for individual services. Moreover, group settings may be especially efficacious for caregivers of youth with ASD because they provide a forum to learn from other caregivers and receive validation from those experiencing similar challenges (Todd et al., 2010). While efficacious, many existing parent trainings for ASD are lengthy (e.g., 12 + weeks in length; Bearss et al., 2015; Dababnah & Parish, 2016; Johnson et al., 2019; Sharp et al., 2019) and pose challenges with retention (Postorino et al., 2017). For all the above reasons, there exists a need to develop a brief and efficacious BPT group intervention targeting challenging behaviors in ASD.
To fill this existing void, we developed a brief group-based BPT intervention for caregivers of children with ASD to focus more centrally on the types of high frequency challenging behavior reported in the ASD population (e.g., externalizing behavior problems, feeding issues, sleep disturbances). To do so, we conducted two focus groups with caregivers of youth with ASD to obtain feedback about the content and structure of the proposed BPT intervention. Subsequently, we conducted an initial pilot efficacy and acceptability test of our novel brief BPT intervention using a longitudinal RCT design with an active control condition. We hypothesized that our novel brief intervention would be associated with reduced child challenging behaviors (operationalized as a broad range of externalizing behavior problems, feeding issues, and sleep disturbances), reduced caregiver stress, and improved caregiver mental health functioning.
Methods
Participants
A total of 38 caregivers with a child aged 5–9 (M = 6.9 years, SD = ± 1.2 years) who was diagnosed with ASD participated. The BPT condition consisted of 29, randomly assigned, caregivers (M = 35.4 years, SD = ± 4.4 years). Nine caregivers (M = 35.1 years, SD = ± 4.0 years) were assigned randomly to the active control intervention (psychoeducation and supportive therapy; PST). As outlined in Table 1, no differences emerged between the two groups with respect to child or caregiver demographic variables including medication status. Nearly all of the youth who were prescribed medication, were prescribed medication for externalizing behaviors.
In addition, no group differences emerged on ASD severity. The mean ADOS-2 scores for both groups were in the “high” level of autism-spectrum related symptoms. As shown in Table 2, the only Time 1 difference between groups was on the Parenting Stress Index Parent Total Composite, F (1,36) = 5.24, p = .028, η2 = 0.13. Importantly, no other dependent variables differed between the two groups at baseline (p’s > 0.20).
Inclusion Measures
Autism Diagnostic Interview-Revised (ADI-R)
The ADI-R is a structured interview used to diagnose ASD and discriminate it from other developmental disorders (Lord et al., 1994). The interview is conducted with the caregiver of a child referred for an evaluation. A licensed psychologist who met research reliability requirements and who was not affiliated with the research study administered the ADI-R.
Autism Diagnostic Observation Schedule, Second Edition (ADOS-2)
The ADOS-2 is a standardized assessment comprised of structured and semi-structured tasks that is used to diagnose ASD. The tasks in the ADOS-2 allow the clinician to observe communication skills, social interaction, and imaginative use of materials in individuals who are being evaluated (Lord et al., 2012). A licensed psychologist who met clinical reliability requirements and who was not affiliated with the research study administered the ADOS-2.
Only children meeting diagnostic criteria for ASD based on both ADI-R and ADOS-2 scoring met inclusion criteria for this study. Two children who were referred for potential study participation failed to meet ASD diagnostic criteria on both ADI-R and ADOS-2 and thus were not included in the trial.
Child Dependent Variables
Unless otherwise noted, all measures were completed by caregivers at baseline (Week 0), outcome assessment (Week 6), and 6-month follow-up (Week 30).
Externalizing Behavior
The Aberrant Behavior Checklist (ABC) is a scale used to measure problem behaviors in individuals with intellectual or developmental disabilities (Aman & Singh, 1986). The checklist measures behaviors in five domains: irritability, agitation, and crying; lethargy/social withdrawal; stereotypic behavior; hyperactivity/noncompliance; and inappropriate speech (Aman & Singh, 1986). Cronbach’s alpha for the ABC in the current study was 0.96, indicating excellent internal consistency reliability.
Positive Behavior
The Nisonger Child Behavior Rating Form (NCBRF) is a 76-item instrument used to measure behaviors in children with ASD (Aman et al., 1996). Each item asks about the occurrence of a behavior and is rated on a 4-point Likert scale (Aman et al., 1996). The NCBRF contains two positive/social behavior subscales and six problem behavior subscales (Aman et al., 1996). The parent version of the NCBRF was administered to our participants to gain information about changes in positive behaviors (e.g., prosocial behavior). Therefore, only the Positive Behavior composite was used. Cronbach’s alpha for the NCBRF positive/social behavior subscales in the current study was 0.95, indicating excellent internal consistency reliability.
Feeding
The Brief Autism Mealtime Behavior Inventory (BAMBI) is an 18-item instrument used to assess mealtime and feeding behavior problems in children with ASD (Lukens & Linscheid, 2008). The BAMBI was specifically developed to be sensitive to mealtime and feeding problems in the ASD population and measured three main factors: limited variety in diet, food refusal, and features of autism (Lukens & Linscheid, 2008). Cronbach’s alpha for the BAMBI in the current study was 0.77, indicating acceptable internal consistency reliability.
Sleep
The Albany Sleep Problems Scale (ASPS) is a 46-item measure that identifies sleep problems in children (Durand, 2008). Items assess difficulties falling asleep, difficulties staying asleep, problems during sleep (e.g. snoring, grinding teeth, bed wetting), and behavioral and emotional problems surrounding bedtime (Durand, 2008). Cronbach’s alpha for the ASPS in the current study was 0.75, indicating acceptable internal consistency reliability.
Caregiver Dependent Variables
Depression
The Beck Depression Inventory, Second Edition (BDI-II) is a 21-item self-report inventory of depression symptoms and severity (Beck et al., 1996). Cronbach’s alpha for the BDI-II in the current study was 0.93, indicating excellent internal consistency reliability.
Stress
The Parenting Stress Index − 4th edition (PSI-4) is an inventory designed to assess the magnitude of stress in caregivers of children aged 1 month − 12 years (Abidin, 2012). The PSI consists of 120 items and yields a total stress score, a score of caregiver characteristics contributing to family stress, and a score of child characteristics contributing to family stress (Abidin, 2012). Cronbach’s alpha for the PSI in the current study was 0.95, indicating excellent internal consistency reliability.
Perceived Acceptability Measure
To assess caregiver perceptions of their assigned treatment, a 2-item, 7-point Likert scale querying treamtent satisfaction (“How satisfied are you with this treatment?”) and acceptability (“How aceptable did you find this treatment for your child’s problem behaviors?”) was completed by caregivers at week 6 (end of the active treatment phase). Higher scores indicate more global satisfaction with the received intervention.
Principal Outcome Measure
Clinical Global Impression-Improvement (CGI-I)
The CGI-I is a clinician-rated scale used to track changes in global functioning and response to treatment (Guy, 1976). An independent evaluator (IE), who was an experienced ASD clinician familiar with all outcomes measures yet unaware of the study hypotheses or treatment assignment (“blinded rater”), completed the CGI-I for changes in caregiver and child behavioral and emotional functioning. To help inform ratings, the IE was provided with all study data except for the perceived acceptability data obtained at the end of the active treatment phase. After reviewing all data at the conclusion of the 6-month follow-up, the IE assigned an omnibus CGI-I for each participating caregiver/child dyad to provide an evaluation of global improvement. The CGI-I score reflects the IE’s assessment of overall caregiver/child dyad change from baseline to 6-month follow-up rated on a scale from very much improved (score of 1) through no change (score of 4) to very much worse (score of 7). By convention, ratings of very much improved (1) or much improved (2) were used to operationalize a positive response (Busner & Targum, 2007). All other scores were classified as a negative treatment response.
Procedures
Participants were recruited from one developmental pediatrics clinic housed in an academic medical center in Syracuse, NY. Families that responded to recruitment were contacted by project staff and administered a qualifying interview (e.g., age of child, ASD diagnosis, ability to travel to group trainings). In addition to meeting age and ASD inclusion criteria, children with ASD were required to have at least one caregiver report challenging behavior. Caregivers of children on stable psychotropic medication (defined as being on the same dose for 3 consecutive months) were allowed to participate. To increase the external validity of these data, no ASD comorbidity or developmental level was excluded. Exclusion criteria included non-English speaking caregivers or caregivers who were not able to commit to attend the 6-treatment sessions. Written informed consent was received from all participants. This study was approved by the IRB at SUNY Upstate Medical University.
After ascertainment and ADI-R/ADOS-2 administration, caregivers were block randomized based upon ASD severity in a 3:1 ratio to one of two conditions: BPT intervention or the active control intervention (PST). While both treatment conditions in our study were active (see below for descriptions), our decision to assign more caregivers to the BPT intervention condition was guided by our hypothesis that the PST intervention would be less efficacious. The 3:1 randomization ratio was selected to balance the need for a control group while allowing greater access to the intervention hypothesized to be more efficacious.
There were four clinical-assessment visits designed to assess study inclusion and dependent variables: screening (Week − 1), baseline (Week 0), outcome assessment (Week 6), and 6-month follow-up (Week 30). The ADOS-2 and ADI-R were administered at screening. Dependent variable assessments were administered at baseline to characterize participants, ensure eligibility, and establish baseline for the outcome measures. Clinical outcome assessments were repeated at treatment endpoint and at a 6-month follow-up visit to assess maintenance.
All measures were completed remotely via a Qualtrics survey. Results were not shared with group providers, participating caregivers, or the blinded IE until after the final 6-month follow-up data collection was complete.
Interventions
BPT development
The novel, brief BPT intervention was originally developed by a consensus conference group of nine clinicians, researchers, and doctoral students with cumulative 100 + years of expertise in research and clinical care of ASD and behavior analysis. Following the initial development of the BPT content, two focus groups were held to refine the intervention. Focus group participants were recruited from the same developmental pediatrics clinic as RCT participants and were selected based upon the same study inclusion/exclusion criteria. The focus groups were led by an experienced clinician with ASD expertise, and participants provided qualitative input about all aspects of the proposed intervention. The intervention and materials were finalized based on refinements from the two focus groups.
BPT intervention
Once finalized, each BPT session was 120 min, delivered in-person on one of the university campuses associated with this study, in a group-based format, and spanned 6 weekly sessions. Similar to other established parent training group interventions (e.g., RUBI, IY), groups were structured around (a) providing education to caregivers about the use of behavior-analytic techniques (e.g., functional assessment, behavior-specific praise, planned ignoring, antecedent- and consequent-based strategies, differential reinforcement, time-out) to address challenging behaviors and (b) facilitating group discussion of these topics through a series of video vignettes. Caregivers were also asked to complete weekly homework assignments related to that week’s instruction. These assignments included collecting antecedent-behavior-consequence data on a target behavior, planned ignoring, differential reinforcement, sleep tracking, and logging food consumption. At the beginning of each session, homework assignments were reviewed and each caregiver was asked to share their experiences within the context of a structured discussion.
The novel, brief BPT intervention consisted of the 6 following weekly topics: (1) Parental attention, social and emotional persistence coaching; (2) Effective praise, increasing child motivation, planned ignoring; (3) Managing externalizing challenging behavior in ASD; (4) Strategies to address sleep disturbances in ASD; (5) Treatments for feeding issues in ASD; (6) Review and conclusions. See Online Resource 1 for full group content. In order to reduce attrition, groups were conducted at times that accommodated families’ schedules, including evening times. There was no attrition in the 6-session BPT group, and there was 100% attendance to all 6 sessions.
PST intervention
Like the novel, brief BPT intervention, each PST session was 120 min, delivered in-person on one of the the university campuses associated with this study, in a group-based format, and the intervention spanned 6 weekly sessions. The PST was designed to be an active control condition to permit higher confidence that changes in dependent variables were due to the BPT intervention as opposed to nonspecific factors, such as time spent with the therapist or support from group members. That is, learning about and discussing ASD diagnosis, treatment, and educational services with an experienced therapist has been shown to be helpful to caregivers of youth with ASD (Estes et al., 2019). Although these discussions can be helpful, PST is far less specific than an ASD-specific group BPT intervention and does not include instruction on the use of evidence-based strategies, which was the key component of the ASD-specific group BPT intervention.
In the current study, the PST curriculum consisted of the same topics as the BPT yet did not include the hypothesized active BPT ingredient (providing training to caregivers about the use of behavior-analytic techniques). PST sessions consisted of psychoeducation pertaining to the topic and the use of supportive, motivational interviewing techniques (e.g., asking open-ended questions, using reflections to communicate empathy, etc.), but did not include a skills-teaching component. See Online Resource 2 for full group content. Similar to the BPT, PST caregivers completed weekly homework assignments related to that week’s instruction, and assignments were reviewed and incorporated into discussion the following week. In order to reduce attrition, we scheduled groups at times that accommodated families’ schedules, including evening times. Similar to the BPT, there was no attrition in the 6-session PST group, and there was 100% attendance to all 6 sessions.
Treatment Fidelity
All BPT and PST group treatment sessions were videorecorded. For both the BPT and PST groups, each session had a scripted outline for the treatment providers (two separate advanced doctoral students for each group) to follow. The session outlines served as a standardized training structure and also provided a fidelity check for treatment implementation. Each topic area to be covered was defined, and observers who had been previously trained in direct observation used these outlines to check for adherence by reviewing all videorecorded sessions. Undergraduate research assistants completed a 3-hour training on the treatment protocol and needed to attain 90% inter-rater reliability with an experienced clinician prior to coding research video recordings. Following attainment of research reliability, the treatment fidelity checklist (see Online Resource 3) was completed for all sessions. For the BPT and PST groups, all 6 sessions were delivered with high fidelity (BPT M = 94.84%; range, 90–100%; PST M = 94.02%; range, 88–100%).
Planned Analyses
Based upon a hypothesized medium effect size, two groups, three measurement periods, and presumed r = .5 correlations between measurements, a sample of 28 caregiver/child dyads were required to attain 80% statistical power. Given our sample of 38 dyads, our repeated measures analyses of variance (ANOVA) were adequately powered to detect statistically significant medium effects.
Results
Principal Outcome Measure
When treating blinded IE CGI-I ratings as a continuous variable, differences emerged between the two groups, t (36) = − 2.49, p = .018. That is, BPT caregiver/child dyads were rated as more improved than PST dyads. Blinded IE CGI-I scale ratings also differed between the two groups when considering the CGI-I dichotomously, X2 (1) = 5.21, p = .022. In the PST group, 2 of the 9 child/caregiver dyads (22%) were judged to be significantly improved on the 6-month follow-up CGI-I scale. In the BPT group, 19 of the 29 child/caregiver dyads (66%) were judged to be significantly improved on the blinded IE CGI-I ratings. In sum, IE ratings on the CGI-I indicated greater improvement among participants who received the BPT.
Secondary Outcome Measures - Child Outcomes
Externalizing Behaviors
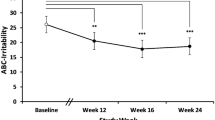
A repeated measures ANOVA comparing ABC composite group X time interactions failed to reach significance, F (1.938, 85.336) = 0.339, p = .707, η2 = 0.01. A main effect of time emerged, F (1.938, 85.336) = 5.721, p = .005, η2 = 0.14. On the ABC, caregivers in both groups reported reductions in child problematic behaviors at 6-month follow-up relative to baseline. No parents reported any medication or medication dosage changes at 6-month follow-up relative to baseline. See Fig. 1 for all child outcomes.
Positive Behaviors
A repeated measures ANOVA comparing NCBRF Positive Behavior composite group X time interactions failed to reach significance, F (1.611, 22.551) = 0.972, p = .376, η2 = 0.07. A main effect of time emerged, F (1.611, 22.551) = 7.094, p = .003, η2 = 0.34. On the NCBRF, caregivers in both groups reported more positive child behaviors at follow-up relative to baseline.
Feeding Problems
A repeated measures ANOVA comparing BAMBI group X time interactions failed to reach significance, F (1.724, 60.332) = 0.764, p = .352, η2 = 0.02. A main effect of time emerged, F (1.724, 60.332) = 3.638, p = .031, η2 = 0.09. Caregivers in both groups reported reductions in feeding problems at follow-up relative to baseline.
Sleep Problems
A repeated measures ANOVA comparing ASPS group X time interactions failed to reach significance, F (1.724, 60.941) = 0.567, p = .547, η2 = 0.02. The main effect of time was also non-significant, F (1.724, 60.941) = 1.822, p = .175, η2 = 0.05.
Child Variables. Dependent child variables, externalizing behavior, positive behavior, feeding, and sleep, measured at Time 1, Time 2, and Time 3 in the Behavioral Parent Training and active control Psychoeducation and Supportive Therapy groups. Scales have different start points for each graph due to differences in the means and total scoring for different measures. ABC = Aberrant Behavior Checklist; ASPS = Albany Sleep Problems Scale; BAMBI = Brief Autism Mealtime Behavior Inventory; NCBRF = Nisonger Child Behavior Rating Form
Secondary Outcome Measures - Caregiver Outcomes
Depression
A repeated measures ANOVA comparing BDI group X time interactions failed to reach significance, F (1.628, 58.598) = 0.348, p = .664, η2 = 0.01. A main effect of time emerged, F (1.628, 58.598) = 4.918, p = .010, η2 = 0.12. Caregivers in both groups reported reductions in depressive symptoms at follow-up relative to baseline. Please see Fig. 2 for all caregiver outcomes.
Caregiver Variables. Dependent caregiver variables, parent stress and depression, measured at Time 1, Time 2, and Time 3 in the Behavioral Parent Training and active control Psychoeducation and Supportive Therapy groups. Scales have different start points for each graph due to differences in the means and total scoring for different measures. BDI-2 = Beck Depression Inventory, Second Edition; PSI = Parenting Stress Index
Caregiver Stress
A repeated measures ANOVA comparing group X time Parenting Stress Composite interactions failed to reach significance, F (1.956, 68.454) = 1.356, p = .264, η2 = 0.04. Similarly, the repeated measures ANOVA comparing group X time Child Stress Composite interactions failed to reach significance, F (1.970, 68.963) = 0.967, p = .384, η2 = 0.03. No main effects of time emerged on either composite.
Perceived Treatment Acceptability
Caregivers in both groups reported globally high satisfaction and treatment acceptability. However, caregivers in the BPT reported more favorable opinions, t (36) = 3.54, p = .001.
Discussion
ASD is defined by the presence of social communication deficits, restricted interests, and repetitive behaviors. In addition to these core symptoms, challenging behaviors (e.g., externalizing behavior problems, feeding issues, and sleep disturbances) are also common (Maskey et al., 2013; Matson et al., 2008). One approach that is effective at increasing prosocial behaviors and reducing challenging behaviors in children with ASD is BPT (Bearss et al., 2015; Prata et al., 2018). Although effective, BPT geared for caregivers of children with ASD takes a considerable amount of time (e.g., > 12 weeks), and may not always address common behavior problems that caregivers find challenging (e.g., feeding issues and sleep disturbances).
To address these concerns, we developed a novel, brief 6-week BPT intervention targeting high-frequency challenging behaviors in ASD. A longitudinal RCT design was employed. One group of caregivers with children diagnosed with ASD received BPT, which consisted of teaching caregivers behavior-analytic principles and treatment strategies designed to target high-frequency challenging behaviors. Outcomes on various measures of child and caregiver functioning (e.g., CGI-I) were compared with an active control group of caregivers that received PST, which entailed psychoeducation about ASD and the use of motivational interviewing techniques.
We predicted the novel BPT intervention would generally be associated improvements as measured by the CGI-I scale, reduced levels of child challenging behaviors as reported by caregivers (e.g., ABC), as well as reduced caregiver stress (PSI) and improved mental health (BDI), compared to the control group. As predicted, there were statistically significant differences for the improvement ratings on the CGI-I completed by a blinded IE (based on all outcome measures) between the caregiver/child dyads in the BPT group versus those in the PST group. Treatment acceptability and satisfaction ratings were also higher in the BPT group. These findings provide preliminary evidence that supports the acceptability and use of our novel brief BPT approach to improve caregiver and child functioning, relative to an active control condition.
Following the BPT, there were significant decreases in caregiver-reported child externalizing behavior, child sleep and feeding challenges, caregiver stress and depression, and increases in positive child behaviors. These findings indicate that the novel, brief BPT may be an efficacious intervention for improving challenging behavior in children with ASD in only 6 weeks. Nonetheless, significant group X time interactions were not found for many of the caregiver-reported child and caregiver dependent variables. As noted in the figures, improvements from Time 1 to Time 2 for externalizing behavior, positive behavior, sleeping, and caregiver depression occurred in both groups; whereas, caregiver stress and feeding only improved in the BPT group. From Time 2 to Time 3 (follow-up), maintenance or improvements across both groups were observed for child positive behaviors, sleeping, and feeding. Caregiver depressive symptom reductions were maintained in the BPT group, but not in the PST group. Child externalizing behaviors and caregiver stress regressed for both groups during follow-up. This may have occurred simply because of a regression to the mean, or because those externalizing behaviors continued to produce reinforcement in other environments (e.g., school; MacDonald et al., 2013). Given the limited maintenance of the externalizing behavior improvements in the absence of treatment, it is not surprising that parenting stress also regressed given the bidirectional relation between child externalizing behavior and caregiver stress (Estes et al., 2019; Neece et al., 2012; Singh et al., 2014).
One possible reason for the lack of interaction effects are the improvements observed with the PST group. As described earlier, the PST was an active treatment group and consisted of education about autism and relied heavily on the use of motivational interviewing techniques. Other, ASD and non-ASD behavioral parent treatment research has indicated that the use of motivational interviewing techniques enhances caregiver engagement and ultimately outcomes (Nock & Kazdin, 2005; Rogers et al., 2019). It is also possible that variables such as simple access to treatment with a provider with ASD knowledge and understanding, having parental voices heard and recognized, feeling listened to and validated, and hearing about the experiences of other caregivers of autistic youth are helpful (Boshoff et al., 2021). Thus, improvements were noted in both groups, possibly due to the PST being an efficacious intervention on its own. Future studies should test the efficacy of the PST against both active and waitlist controls to explore this possibility.
A distinct advantage of the novel BPT evaluated in the current study, relative to past, lengthier BPTs, is the brief nature of the intervention. Previously studied BPT groups range from a minimum 12 weeks (Dababnah & Parish, 2016; Johnson et al., 2019; Sharp et al., 2019) up to 24 weeks or longer (Bearss et al., 2015), and appreciable participant attrition has been reported (e.g., Bearss et al., 2015). In the current study, there was no participant attrition in either group and there was 100% attendance to all 6 sessions, both of which may be attributable to the shorter duration of the treatment which caregivers rated as acceptable. Therefore, the brevity of this BPT may increase access to these important behavioral services for caregivers who are experiencing long-wait lists for services (Monz et al., 2019). It will be important for future research to evaluate dosage effects to determine the optimal amount of time needed to maximize treatment outcomes while maintaining caregiver satisfaction and retention across BPTs.
There were also several limitations worth noting. ASD severity was the primary variable of interest in our randomization process, however, developmental level (e.g., IQ) was not accounted. Future research should consider the extent to which developmental level impacts BPT outcomes. The current study also relied heavily on caregiver report of child behavior, with no direct measurement of the challenging behaviors of interest. Collecting direct-observation baseline and post-treatment data in the natural environment, in addition to caregiver reports of behavior, may allow for greater understanding of how BPTs affect child and caregiver outcomes – especially because there are often discrepancies between caregiver report and direct observation of child behaviors (Moens et al., 2018). It should also be noted that the BAMBI and ASPS had acceptable but low internal consistencies. In addition to these measurement considerations, it may be of interest for future researchers to consider the interventions’ potential for decreasing the use of medications targeting disruptive behaviors.
We also did not collect data on adherence with homework assignments in either group. Although we reviewed homework each week through a structured 15-minute discussion, there was no formal data collected to assess the caregivers’ fidelity and follow through with these tasks. Because homework was verbally reviewed in session, it is likely that adherence was higher than if no homework review was incorporated at all. However, in future studies, homework adherence will be important to evaluate to ensure skill-based practice is being completed as prescribed, and to determine if varying levels of adherence impact outcomes (Chacko et al., 2016).
While video vignettes were used to illustrate concepts, this novel BPT did not include any role-play activities within the sessions. Role-play may have helped the instructors evaluate understanding and skill level across participants prior to caregivers implementing procedures at home without supervision. In most behavioral-skills training sequences, there is a model and role-play component to ensure accurate implementation of these procedures (Van Camp et al., 2008). Future studies could evaluate the efficacy of BPT with and without a role-play component.
Finally, this BPT was conducted in-person for all sessions, yet there has been a recent trend, clearly accelerated by COVID-19, towards developing virtual versions of BPT programs. These virtual BPT programs have demonstrated efficacy in improving parenting skills and child symptoms (Baumel & Faber, 2018; DuPaul et al., 2018), yet caregivers have reported lower acceptability of virtual compared to in-person BPTs (DuPaul et al., 2018). Future research should continue to evaluate the efficacy of virtual BPTs and consider the use of supplementing in-person core BPT programs with additional follow-up virtual trainings.
In conclusion, the present BPT intervention was associated with global improvement and was more acceptable to caregivers relative to caregivers in an active control group. This brief BPT was efficacious in helping caregivers of children with ASD who engage in challenging behaviors learn how to implement evidence-based procedures and best practices to promote prosocial behavior and suppress challenging behaviors in their child. Moreover, the BPT placed an emphasis on promoting positive interactions between caregiver and child to improve the well-being of both the child and caregiver. Overall, the brevity of this BPT offers a promising approach that may alleviate wait-list laden service providers (Buescher et al., 2014; Gordon-Lipkin et al., 2016).
References
Abidin, R. (2012). Parenting Stress Index–Fourth Edition (PSI-4). Lutz, FL: Psychological Assessment Resources. Psychological Assessment Resources
Aman, M. G., & Singh, N. N. (1986). Aberrant Behavior Checklist manual. Slosson Educational Publications
Aman, M. G., Tassé, M. J., Rojahn, J., & Hammer, D. (1996). The Nisonger CBRF: A child behavior rating form for children with developmental disabilities. Research in Developmental Disabilities, 17(1), 41–57. https://doi.org/10.1016/0891-4222(95)00039-9
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition). American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596
Argumedes, M., Lanovaz, M. J., & Larivée, S. (2018). Brief Report: Impact of Challenging Behavior on Parenting Stress in Mothers and Fathers of Children with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 48(7), 2585–2589. https://doi.org/10.1007/s10803-018-3513-1
Baumel, A., & Faber, K. (2018). Evaluating Triple P Online: A Digital Parent Training Program for Child Behavior Problems. Cognitive and Behavioral Practice, 25(4), 538–543. https://doi.org/10.1016/j.cbpra.2017.10.001
Bearss, K., Johnson, C., Smith, T., Lecavalier, L., Swiezy, N., Aman, M. … Scahill, L. (2015). Effect of parent training vs parent education on behavioral problems in children with autism spectrum disorder: A randomized clinical trial. JAMA, 313(15), 1524–1533. https://doi.org/10.1001/jama.2015.3150
Beavers, G. A., Iwata, B. A., & Lerman, D. C. (2013). Thirty Years of Research on the Functional Analysis of Problem Behavior. Journal of Applied Behavior Analysis, 46(1), 1–21. https://doi.org/10.1002/jaba.30
Beck, A., Steer, R., & Brown, G. (1996). Beck Depression Inventory—2nd edition (BDI-II). Pearson Publishing
Boshoff, K., Bowen-Salter, H., Gibbs, D., Phillips, R. L., Porter, L., & Wiles, L. (2021). A meta-synthesis of how parents of children with autism describe their experience of accessing and using routine healthcare services for their children. Health & Social Care in the Community. https://doi.org/10.1111/hsc.13369
Buescher, A. V. S., Cidav, Z., Knapp, M., & Mandell, D. S. (2014). Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics, 168(8), 721–728. https://doi.org/10.1001/jamapediatrics.2014.210
Busner, J., & Targum, S. D. (2007). The Clinical Global Impressions Scale. Psychiatry (Edgmont), 4(7), 28–37
Chacko, A., Jensen, S. A., Lowry, L. S., Cornwell, M., Chimklis, A., Chan, E. … Pulgarin, B. (2016). Engagement in Behavioral Parent Training: Review of the Literature and Implications for Practice. Clinical Child and Family Psychology Review, 19(3), 204–215. https://doi.org/10.1007/s10567-016-0205-2
Dababnah, S., & Parish, S. L. (2016). Incredible Years Program Tailored to Parents of Preschoolers With Autism: Pilot Results. Research on Social Work Practice, 26(4), 372–385. https://doi.org/10.1177/1049731514558004
DuPaul, G. J., Kern, L., Belk, G., Custer, B., Daffner, M., Hatfield, A., & Peek, D. (2018). Face-to-Face Versus Online Behavioral Parent Training for Young Children at Risk for ADHD: Treatment Engagement and Outcomes. Journal of Clinical Child & Adolescent Psychology, 47(sup1), S369–S383. https://doi.org/10.1080/15374416.2017.1342544
Durand, M. (2008). When Children Don’t Sleep Well: Parent Workbook: Interventions for pediatric sleep disorders. Oxford University Press
Estes, A., Swain, D. M., & MacDuffie, K. E. (2019). The effects of early autism intervention on parents and family adaptive functioning. Pediatric Medicine (Hong Kong, China), 2. https://doi.org/10.21037/pm.2019.05.05
Fitzpatrick, S. E., Srivorakiat, L., Wink, L. K., Pedapati, E. V., & Erickson, C. A. (2016). Aggression in autism spectrum disorder: Presentation and treatment options. Neuropsychiatric Disease and Treatment, 12, 1525–1538. https://doi.org/10.2147/NDT.S84585
Gordon-Lipkin, E., Foster, J., & Peacock, G. (2016). Whittling Down the Wait Time. Pediatric Clinics of North America, 63(5), 851–859. https://doi.org/10.1016/j.pcl.2016.06.007
Guy, W. (1976). ECDEU Assessment Manual for Psychopharmacology. U.S. Department of Health, Education, and Welfare
Hayes, S. A., & Watson, S. L. (2013). The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(3), 629–642. https://doi.org/10.1007/s10803-012-1604-y
Johnson, C. R., Brown, K., Hyman, S. L., Brooks, M. M., Aponte, C., Levato, L. … Smith, T. (2019). Parent Training for Feeding Problems in Children With Autism Spectrum Disorder: Initial Randomized Trial. Journal of Pediatric Psychology, 44(2), 164–175. https://doi.org/10.1093/jpepsy/jsy063
Karst, J. S., & Van Hecke, A. V. (2012). Parent and family impact of autism spectrum disorders: A review and proposed model for intervention evaluation. Clinical Child and Family Psychology Review, 15(3), 247–277. https://doi.org/10.1007/s10567-012-0119-6
Kirkpatrick, B., Louw, J. S., & Leader, G. (2019). Efficacy of parent training incorporated in behavioral sleep interventions for children with autism spectrum disorder and/or intellectual disabilities: A systematic review. Sleep Medicine, 53, 141–152. https://doi.org/10.1016/j.sleep.2018.08.034
Lecavalier, L., Leone, S., & Wiltz, J. (2006). The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research: JIDR, 50(Pt 3), 172–183. https://doi.org/10.1111/j.1365-2788.2005.00732.x
Lord, C., Rutter, M., DiLavore, P., Risi, S., Gotham, K., Bishop, S. … Guthrie, W. (2012). Autism Diagnostic Observation Schedule (2nd ed.). Western Psychological Services
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. https://doi.org/10.1007/BF02172145
Lukens, C. T., & Linscheid, T. R. (2008). Development and validation of an inventory to assess mealtime behavior problems in children with autism. Journal of Autism and Developmental Disorders, 38(2), 342–352. https://doi.org/10.1007/s10803-007-0401-5
MacDonald, J. M., Ahearn, W. H., Parry-Cruwys, D., Bancroft, S., & Dube, W. V. (2013). Persistence during Extinction: Examining the Effects of Continuous and Intermittent Reinforcement on Problem Behavior. Journal of Applied Behavior Analysis, 46(1), 333–338. https://doi.org/10.1002/jaba.3
Maenner, M. J. (2021). Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2018. MMWR. Surveillance Summaries, 70. https://doi.org/10.15585/mmwr.ss7011a1
Maskey, M., Warnell, F., Parr, J. R., Couteur, A. L., & McConachie, H. (2013). Emotional and behavioural problems in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(4), 851–860. https://doi.org/10.1007/s10803-012-1622-9
Matson, J. L., Wilkins, J., & Macken, J. (2008). The Relationship of Challenging Behaviors to Severity and Symptoms of Autism Spectrum Disorders. Journal of Mental Health Research in Intellectual Disabilities, 2(1), 29–44. https://doi.org/10.1080/19315860802611415
McStay, R. L., Dissanayake, C., Scheeren, A., Koot, H. M., & Begeer, S. (2014). Parenting stress and autism: The role of age, autism severity, quality of life and problem behaviour of children and adolescents with autism. Autism, 18(5), 502–510. https://doi.org/10.1177/1362361313485163
Miyajima, A., Tateyama, K., Fuji, S., Nakaoka, K., Hirao, K., & Higaki, K. (2017). Development of an Intervention Programme for Selective Eating in Children with Autism Spectrum Disorder. Hong Kong Journal of Occupational Therapy: HKJOT, 30(1), 22–32. https://doi.org/10.1016/j.hkjot.2017.10.001
Moens, M. A., Weeland, J., Van der Giessen, D., Chhangur, R. R., & Overbeek, G. (2018). In the Eye of the Beholder? Parent-Observer Discrepancies in Parenting and Child Disruptive Behavior Assessments. Journal of Abnormal Child Psychology, 46(6), 1147–1159. https://doi.org/10.1007/s10802-017-0381-7
Monz, B. U., Houghton, R., Law, K., & Loss, G. (2019). Treatment patterns in children with autism in the United States. Autism Research: Official Journal of the International Society for Autism Research, 12(3), 517–526. https://doi.org/10.1002/aur.2070
Neece, C. L., Green, S. A., & Baker, B. L. (2012). Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities, 117(1), 48–66. https://doi.org/10.1352/1944-7558-117.1.48
Nock, M. K., & Kazdin, A. E. (2005). Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology, 73(5), 872–879. https://doi.org/10.1037/0022-006X.73.5.872
Postorino, V., Sharp, W. G., McCracken, C. E., Bearss, K., Burrell, T. L., Evans, A. N., & Scahill, L. (2017). A Systematic Review and Meta-analysis of Parent Training for Disruptive Behavior in Children with Autism Spectrum Disorder. Clinical Child and Family Psychology Review, 20(4), 391–402. https://doi.org/10.1007/s10567-017-0237-2
Prata, J., Lawson, W., & Coelho, R. (2018). Parent training for parents of children on the autism spectrum: A review. International Journal of Clinical Neurosciences and Mental Health. https://doi.org/10.21035/ijcnmh.2018.5.3. 3
Reynolds, A. M., & Malow, B. A. (2011). Sleep and Autism Spectrum Disorders. Pediatric Clinics of North America, 58(3), 685–698. https://doi.org/10.1016/j.pcl.2011.03.009
Richdale, A. L., & Schreck, K. A. (2009). Sleep problems in autism spectrum disorders: Prevalence, nature, & possible biopsychosocial aetiologies. Sleep Medicine Reviews, 13(6), 403–411. https://doi.org/10.1016/j.smrv.2009.02.003
Rogers, S. J., Estes, A., Vismara, L., Munson, J., Zierhut, C., Greenson, J. … Talbott, M. (2019). Enhancing Low-Intensity Coaching in Parent Implemented Early Start Denver Model Intervention for Early Autism: A Randomized Comparison Treatment Trial. Journal of Autism and Developmental Disorders, 49(2), 632–646. https://doi.org/10.1007/s10803-018-3740-5
Schrott, B., Kasperzack, D., Weber, L., Becker, K., Burghardt, R., & Kamp-Becker, I. (2019). Effectiveness of the Stepping Stones Triple P Group Parenting Program as an Additional Intervention in the Treatment of Autism Spectrum Disorders: Effects on Parenting Variables. Journal of Autism and Developmental Disorders, 49(3), 913–923. https://doi.org/10.1007/s10803-018-3764-x
Sharp, W. G., Burrell, T. L., Berry, R. C., Stubbs, K. H., McCracken, C. E., Gillespie, S. E., & Scahill, L. (2019). The Autism Managing Eating Aversions and Limited Variety Plan vs Parent Education: A Randomized Clinical Trial. The Journal of Pediatrics, 211, 185–192e1. https://doi.org/10.1016/j.jpeds.2019.03.046
Sharp, W. G., Burrell, T. L., & Jaquess, D. L. (2014). The Autism MEAL Plan: A parent-training curriculum to manage eating aversions and low intake among children with autism. Autism: The International Journal of Research and Practice, 18(6), 712–722. https://doi.org/10.1177/1362361313489190
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929. https://doi.org/10.1097/CHI.0b013e318179964f
Singh, N. N., Lancioni, G. E., Winton, A. S. W., Karazsia, B. T., Myers, R. E., Latham, L. L., & Singh, J. (2014). Mindfulness-Based Positive Behavior Support (MBPBS) for Mothers of Adolescents with Autism Spectrum Disorder: Effects on Adolescents’ Behavior and Parental Stress. Mindfulness, 5(6), 646–657. https://doi.org/10.1007/s12671-014-0321-3
Tellegen, C. L., & Sanders, M. R. (2014). A randomized controlled trial evaluating a brief parenting program with children with autism spectrum disorders. Journal of Consulting and Clinical Psychology, 82(6), 1193–1200. https://doi.org/10.1037/a0037246
Todd, S., Bromley, J., Ioannou, K., Harrison, J., Mellor, C., Taylor, E., & Crabtree, E. (2010). Using Group-Based Parent Training Interventions with Parents of Children with Disabilities: A Description of Process, Content and Outcomes in Clinical Practice. Child and Adolescent Mental Health, 15(3), 171–175. https://doi.org/10.1111/j.1475-3588.2009.00553.x
Van Camp, C. M., Montgomery, J. L., Vollmer, T. R., Kosarek, J. A., Happe, S., Burgos, V., & Manzolillo, A. (2008). Behavioral Parent Training in Child Welfare: Maintenance and Booster Training. Research on Social Work Practice, 18(5), 392–400. https://doi.org/10.1177/1049731508318658
Williams, M. E., Hastings, R. P., & Hutchings, J. (2020). The Incredible Years Autism Spectrum and Language Delays Parent Program: A Pragmatic, Feasibility Randomized Controlled Trial. Autism Research: Official Journal of the International Society for Autism Research, 13(6), 1011–1022. https://doi.org/10.1002/aur.2265
Yang, X. L., Liang, S., Zou, M. Y., Sun, C. H., Han, P. P., Jiang, X. T. … Wu, L. J. (2018). Are gastrointestinal and sleep problems associated with behavioral symptoms of autism spectrum disorder? Psychiatry Research, 259, 229–235. https://doi.org/10.1016/j.psychres.2017.10.040
Acknowledgments
We would like to thank Avery Albert, Nicole M. DeRose, Ellie Kaplan, Brian K. Martens, Leah Phaneuf, and Lea Taylor for their assistance in the conceptualization and execution of this project. The authors would also like to thank the Nappi family for their generous support of this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rohacek, A., Baxter, E.L., Sullivan, W. et al. A Preliminary Evaluation of a Brief Behavioral Parent Training for Challenging Behavior in Autism Spectrum Disorder. J Autism Dev Disord 53, 2964–2974 (2023). https://doi.org/10.1007/s10803-022-05493-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05493-3