Abstract
Symptoms of depression and eating disorders increase during adolescence, particularly among girls, and they tend to co-occur. Despite this evidence, there is meager research on whether depression increases the risk of future eating pathology, or vice versa, and we do not know whether these processes are different for adolescent girls and boys. Accordingly, this study explored the prospective reciprocal associations between depressive symptoms and disordered eating at different time points from preadolescence to mid-adolescence and tested the moderator effect of gender on these associations. A community-based sample of Spanish youth (N = 942, 49 % female) was assessed at ages of approximately 10-11 (T1), 12-13 (T2), 14-15 (T3), and 16-17 (T4) years. The bidirectional relationships between depressive symptoms and disordered eating were estimated in an autoregressive cross-lagged model with latent variables. A unidirectional, age-specific association between depressive symptoms at T1 and disordered eating at T2 was found. No other significant cross-lagged effect emerged, but the stability of the constructs was considerable. Gender did not moderate any of the links examined. Regardless of gender, the transition from childhood to adolescence appears to be a key period when depressive symptoms foster the development of disordered eating. These findings suggest that early prevention and treatment of depression targeting both girls and boys may result in lower levels of depressive symptoms and disordered eating in adolescence.
Similar content being viewed by others
Adolescence is a period of high risk for the onset of depression (Hankin et al. 1998) and eating pathology (Lewinsohn et al. 2000), especially among girls (Ferreiro et al. 2012). In particular, many adolescents experience subthreshold forms of depression (Kessler and Walters 1998) and eating disorders (Chamay-Weber et al. 2005) but nonetheless undergo similar psychological impairment as those recognized as clinically affected (Ackard et al. 2011; Gotlib et al. 1995). Whether considering clinical or subclinical syndromes, depressive and eating disturbances tend to co-occur (Godart et al. 2007; Santos et al. 2007) and some underlying factors may contribute to the etiology of both problems (Johnson and Wardle 2005; Nolen-Hoeksema et al. 2007). For example, dissatisfaction with one’s body may precipitate depressed mood as well as disordered eating behaviors (e.g., McCarthy 1990). Despite all this evidence indicating a strong association between depressive and eating psychopathology, the developmental course of their relationship remains unclear.
It has been suggested that depression may give rise to eating problems. According to the affect regulation theory, overeating initiates as an attempt to cope with negative emotions (Heatherton and Baumeister 1991; Stice et al. 1998). Depressed mood is also hypothesized to interfere with healthy self-care behaviors, including eating habits (Fulkerson et al. 2004). Moreover, depressed individuals may resort to harmful weight-control practices in an effort to counter their low self-esteem by altering their body shape to align with the thin ideal for females (McCarthy 1990) or the muscular ideal for males (Cafri et al. 2005). It should also be noted that appetite and weight disturbances are acknowledged symptoms of depression (American Psychiatric Association [APA], 2000; Maxwell and Cole 2009), and hence a correlation between both constructs is expected. Conversely, eating pathology may increase the risk of depression for several reasons. It is well-known that dietary restriction negatively affects mood, as shown by classic experiments on semi-starvation (Franklin et al. 1948). Dieting may also result in failure to control weight in the long term (Neumark-Sztainer et al. 2006; Neumark-Sztainer et al. 2012) and recurrent cycles of binge eating and purging may lead to feelings of shame and guilt (Stice et al. 2000), thus promoting depressed affect. Additionally, because body image is an important source of self-esteem among adolescents (Wichstrøm 1998), youth who are discontented with their appearance may gradually feel dissatisfied with their overall self and become depressed (Marmorstein et al. 2008; Rawana et al. 2010). Given that both directional effects are theoretically well-founded, negative affect and eating pathology may also foster each other through a transactional, circular process (Stice 1998).
A number of longitudinal studies conducted in community samples have explored the predictive ability of depression on eating problems, or vice versa. In this regard, it has been reported that depressive disorders (Johnson et al. 2002) and depressed mood (Hautala et al. 2011; Leon et al. 1999; Linde et al. 2009; Tyrka et al. 2002) in adolescence are associated with a heightened risk of future disordered eating. Similarly, there is evidence that eating problems, including dietary restraint and bulimic symptoms, predict onset of depression (Stice et al. 2000) and increases in depressive symptoms (Stice and Bearman 2001) in adolescent girls. Nonetheless, other studies with community adolescents do not support the pathway either from depressive symptoms to later disordered eating (Keel et al. 1997; Wichstrøm 2000) or the other way around (Ferreiro et al. 2011). Although past results are on the whole suggestive of possible prospective associations between depression and eating problems, the temporal nature of these associations cannot be ascertained by examining unidirectional relationships because this approach does not allow researchers to rule out reverse causation (Cole and Maxwell 2003).
Only recently have a number of researchers addressed the bidirectional relationships between depression and eating problems. In particular, we have located eight longitudinal studies examining the reciprocal association between these two disturbances in community samples. Unfortunately, the results are inconsistent. Three of these studies have found a prospective reciprocal association between depressive and bulimic symptoms in adolescent girls and young women (Presnell et al. 2009; Skinner et al. 2012; Stice et al. 2004). However, three other studies targeting female youth have reported only unidirectional effects, either from depressive symptoms to subsequent eating pathology (Measelle et al. 2006; Spoor et al. 2006) or from eating pathology to later depressive symptoms (Marmorstein et al. 2008). Further, two additional studies have failed to detect a prospective relationship between depressive and eating disturbances in either direction among adolescent girls (Stice 1998) and women (Procopio et al. 2006). These discrepancies may be partly due to divergences in the measures (bulimic symptoms vs. general eating pathology), the inter-assessment intervals (from 9 months to 3 years), or the participants’ age (from early adolescence to middle adulthood). Nevertheless, some sort of analytic artifacts could have affected the results. Specifically, most studies treated depression and eating pathology as two variables to be predicted in different models rather than two correlated outcomes within the same model (Measelle et al. 2006; Presnell et al. 2009; Procopio et al. 2006; Skinner et al. 2012; Stice et al. 2004), so that the models may be biased because of the omission of relevant relations between variables (Cole and Maxwell 2003).
Existing research on the reciprocal association between depressive and eating disturbances is limited by the use of female-only samples. However, despite the female overrepresentation in these psychopathologies (APA 2000), depression is a common diagnosis in the male population (Alonso et al. 2004) and eating problems afflict males as well, perhaps more than previously thought (Darcy 2011). Therefore, it is also timely to elucidate the etiology of these problems in boys. In light of the gendered nature of depression and eating disorders, the reciprocal relationships between both disturbances may be more evident in girls than boys (Ferreiro et al. 2012). In fact, some school-based longitudinal studies support the existence of a female-specific pathway from affective symptoms to the development of eating problems among adolescents (Beato-Fernández et al. 2007; Jackson and Chen 2008). In contrast, other studies have not found gender differences in the effect of depression on concurrent (Hautala et al. 2008; Wichstrøm 1995) and subsequent (Ferreiro et al. 2011; Johnson et al. 2002; Wichstrøm 2000) disordered eating in community samples of adolescents. Likewise, there is conflicting evidence coming from community-based studies that suggests either that eating-related variables exert unique risk for depression onset in girls (Bearman and Stice 2008) or that girls and boys are more similar than different with respect to the impact of disordered eating on depressive symptoms both concurrently (Santos et al. 2007) and prospectively (Vaughan and Halpern 2010). Thus, there remain important gaps in knowledge regarding the interplay among gender, depression, and disordered eating.
As far as we know, the current study is the first longitudinal investigation devoted to clarifying the temporal nature of the association between depressive symptoms and disordered eating among adolescents of both genders. Accordingly, the specific goals of this study were to explore the prospective bidirectional relations between depressive symptoms and disordered eating across adolescence and to determine whether these relations differed by gender. To enable a powerful test of these aims, a large community-based sample of youth was repeatedly followed-up from preadolescence to mid-adolescence, thus capturing a critical developmental period for the onset of depressive symptoms and disordered eating and for the occurrence of gender differences (e.g., Ferreiro et al. 2012).
Method
Participants
The initial sample was recruited from different public and private schools, which were randomly selected by stratification by geographical areas in the province of A Coruña (Galicia, Spain) to maximize representativeness. Out of the 15 schools contacted, three declined to participate. Enrollment was open to all students in grades 5-6 of primary school who did not have any problems that would preclude them from understanding the assessment. Of the eligible students in the participating schools, 98 % agreed to take part in the study, with 942 pupils (465 [49 %] girls and 477 [51 %] boys) providing data at baseline (T1). These youth were followed-up in alternate academic years across three additional waves of data, so that 882 adolescents (437 [50 %] girls and 445 [50 %] boys), 748 participants (376 [50 %] girls and 372 [50 %] boys), and 476 adolescents (247 [52 %] girls and 229 [48 %] boys) completed the second (T2), third (T3), and fourth (T4) assessments, respectively. Although the assessments were planned to minimize age differences, there was slight variability in age at each wave because the schools were visited at different times within the same academic year and repeat students attending the grades targeted were also included in the sample (M ageT1 [SD] = 10.83 [0.75]; M ageT2 [SD] = 12.85 [0.77]; M ageT3 [SD] = 14.98 [0.84]; M ageT4 [SD] = 16.40 [0.82]).
According to the characteristics of the sample at study entry, the parents’ educational level (measured as the highest educational level attained by either parent) was as follows: 68 % primary education, 20 % secondary education, and 12 % higher education. The ethnic composition of the sample was 98 % Caucasian, 1 % Arab, and 1 % “other”, which is consistent with the relatively homogeneous ethnic breakdown of the population of reference (Instituto Galego de Estatística 2010).
Measures
Children’s Depression Inventory (CDI; Kovacs 1992)
The CDI is a 27-item self-report measure that evaluates depressive symptomatology in children and adolescents. Total scores range from 0 to 54, with a cutoff score of 19 suggesting significant depression. The Spanish version of the CDI used in this study has demonstrated adequate internal consistency, test-retest reliability, and concurrent and convergent validity (del Barrio et al. 1999). The α coefficient was 0.84 at T1, 0.86 at T2 and T3, and 0.85 at T4.
Children’s Eating Attitudes Test (ChEAT; Maloney et al. 1988)
The ChEAT is a 26-item self-report scale that assesses dysfunctional eating attitudes and behaviors among children and adolescents. Total scores range from 0 to 78, with a cutoff score of 20 as indicative of eating disorder risk. The Spanish version of the ChEAT used in this study has shown satisfactory internal consistency and concurrent validity (Senra et al. 2007). Items 9 (“I vomit after I have eaten”) and 26 (“I have the urge to vomit after eating”) were not administered at T1 because they were deemed unsuitable for the age group studied. These items were therefore deleted at all time points to maximize measurement equivalence. The α coefficient was 0.80 at T1, 0.85 at T2, 0.88 at T3, and 0.89 at T4.
Procedure
The research received approval from the Bioethics Committee of the University of Santiago de Compostela and the Galician Regional Government. Permission to carry out the study was requested from the school boards. Informed consent was obtained from the parents of the pupils who took part in the study. Moreover, the youth themselves were allowed to withdraw from the study (one student at T1, five at T2, four at T3, and none at T4 chose to do so). Participation was rewarded by inclusion in a prize draw for five laptops and four tablet computers after T3 and T4, respectively.
The data were collected in classrooms of 20-25 students. All groups were told that the purpose of the research was to explore a variety of protective and risk behaviors associated with youth wellbeing and were given standard instructions for filling out the questionnaires. Two trained research assistants unrelated to the schools enrolled in the study monitored the assessment session. Administration of the questionnaires of interest for this investigation took about 15 min. When a large group of students were absent on the day of the survey because of attendance at extracurricular academic activities, they were rescheduled for later assessment as soon as possible.
Statistical Analyses
To accomplish the study aims, we conducted a series of analyses using structural equation modeling (SEM). As latent variable models outperform those based on manifest variables (Kline 2011) and parcelling can be a good solution to create latent variables (Coffman and MacCallum 2005), we first examined the factor structure of depressive symptoms and disordered eating and established a number of parcels as indicators of each latent construct. After confirming the measurement model, we tested the temporal relationship between depressive symptoms and disordered eating by fitting a latent variable autoregressive cross-lagged model. In this model, variance in each outcome (latent depressive symptoms and latent disordered eating) at T2, T3, and T4 was derived from two main sources: the effect of the same construct at T1, T2, and T3 (autoregressive paths) and the effect of the other construct at T1, T2, and T3 (cross-lagged paths). Because χ 2 is very sensitive to sample size and tends to be significant (leading to rejection of the model) when sample sizes are large, as in the present study, we considered other fit indices, including the comparative fit index (CFI), the Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA). Finally, we carried out a two-group comparison to assess the moderator effect of gender and evaluated differences in model fit according to Satorra’s (2000) procedure. All of the models were computed using a robust maximum likelihood estimator and missing data were handled using a full information maximum likelihood approach in Mplus 6.1.
Results
Attrition Analyses
Considering the number of respondents at baseline as a benchmark, the retention rate was 94 % at T2, 79 % at T3, and 51 % at T4. Heightened attrition at T4 mainly occurred because by this time most participants had completed compulsory education and those who left school could not be followed-up. Participants available at all assessments were not significantly different from those who missed one or more assessments on any baseline clinical or demographic variable except age (t = 9.49, p < 0.001). Study completers were younger than non-completers, which is probably an artifact reflecting that older participants were more likely to have finished elementary education and left school during the study period.
Descriptive Statistics
Means and standard deviations for the observed variables at each measurement occasion are presented in Table 1 for the total sample and by gender, along with the results of t tests comparing girls and boys. Girls scored higher than boys on depressive symptoms at T3 and T4 and disordered eating at T2, T3, and T4. Thus, gender differences in depressive symptoms emerged at some point between T2 and T3 (i.e., approximately between ages 12-13 and 14-15), whereas gender differences in disordered eating emerged between T1 and T2 (i.e., approximately between ages 10-11 and 12-13).
Measurement Model Specification and Confirmation
Although there has been some variation in the number of factors found for the CDI, a sizable body of research converges in suggesting five factors as appropriate (Craighead et al. 1995; Kovacs 1992; Steele et al. 2006). Using data from the approximate mid-point of the observational period (T2), a five-factor structure consisting of Self-criticism (items 2, 3, 7, 8, 14, and 24), Dysphoria (items 1, 10, and 17), Social Isolation (items 12, 20, 22, 25, and 27), Externalizing (items 15, 23, and 26), and Worry (items 6, 11, and 19) fitted the data well, CFI = 0.94, TLI = 0.92, RMSEA = 0.03. A latent depressive symptom variable was thereby created at each time point from the above five factors, represented as observed sum of scores. The factor loadings of identical indicators were constrained to be equal across time to avoid confounding actual change in depressive symptoms and measurement change. Residuals of the same indicators at different time points were allowed to correlate. The hypothesized measurement model for the CDI across time provided a good fit, CFI = 0.97, TLI = 0.96, RMSEA = 0.03.
A latent disordered eating measure was then created following the same procedures. Although prior research has generally found four factors underlying the structure of the ChEAT (Senra et al. 2007; Smolak and Levine 1994), there is also some evidence that a three-factor solution may work better for boys (Thomas et al. 2000). In this case, a three-factor model consisting of Fear of Getting Fat (items 1, 3, 10, 11, 12, 14, and 22), Dieting (items 2, 6, 7, 16, 17, 19, and 23), and Bulimic Symptoms (items 4, 18, 21, and 24) provided the best fit for the entire sample at T2, CFI = 0.94, TLI = 0.92, RMSEA = 0.04, and across time, CFI = 0.97, TLI = 0.95, RMSEA = 0.05, and was therefore used.
Autoregressive Cross-lagged Model
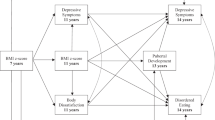
On the basis of measurement models, an autoregressive cross-lagged model linking latent depressive symptoms and latent disordered eating was tested (see Fig. 1). The model fitted the data well, CFI = 0.94, TLI = 0.93, RMSEA = 0.04. The autoregressive paths for both depressive symptoms and disordered eating were significant at each time interval, peaking between T3 and T4. In contrast, only one cross-lagged path emerged as significant, namely between depressive symptoms at T1 and disordered eating at T2.
Moderator Tests
To test whether the autoregressive cross-lagged model was moderated by gender, a model in which all paths were constrained to be equal across genders was compared with a model in which the paths were freely estimated for girls and boys. Chi-square difference tests revealed that the unconstrained model fitted the data slightly better than the constrained model, Δχ2 = 38.35, df = 12, p = 0.005. However, fixing individual paths did not result in significantly poorer fit, so that none of the stability or cross-lagged coefficients was significantly different between girls and boys.
Discussion
The current study explored the prospective reciprocal associations between depressive symptoms and disordered eating at four different time points spanning approximately from preadolescence to mid-adolescence and tested whether these associations differed by gender. Overall, the results showed that both depressive symptoms and disordered were relatively stable throughout the study period, whereas only a time-specific cross-lagged association between depressive symptoms at T1 (approximately age 10-11) and disordered eating at T2 (approximately age 12-13) emerged as significant over and above stability. These effects held for both girls and boys. The lack of significance of most of the associations across psychopathological domains partially converges with some studies documenting no longitudinal relationship between depressive and bulimic symptoms in girls and women beyond the impact of preexisting symptomatology (Procopio et al. 2006; Stice 1998). In addition, the results also provide partial support for a unidirectional influence of depressive symptoms on later disordered eating, in accordance with some prior studies involving adolescent girls and young women (Measelle et al. 2006; Spoor et al. 2006). In contrast, the present findings are at odds with other female-specific studies reporting a reciprocal relationship between depressive and bulimic symptoms (Presnell et al. 2009; Skinner et al. 2012; Stice et al. 2004) or a unidirectional effect of eating pathology on later depressive symptoms (Marmorstein et al. 2008).
The effect of depressive symptoms at T1 on disordered eating at T2 dovetails with the affect regulation theory (Heatherton and Baumeister 1991) and reveals that depressive symptomatology may indeed lead to eating problems during adolescence, which is consistent with previous data (Hautala et al. 2011; Johnson et al. 2002; Leon et al. 1999; Linde et al. 2009; Tyrka et al. 2002). However, because this association was only found between the earliest assessments, depressive symptoms appear to give rise to disordered eating primarily during a crucial period covering the transition from childhood to adolescence. In this regard, early adolescence is a demanding developmental phase involving major life events such as puberty and initiation of dating behaviors (Simmons et al. 1987), which may render youth particularly vulnerable to appearance-related concerns. Thus, depressed individuals navigating the challenges of early adolescence may be especially inclined to turn to disordered eating in an attempt to achieve an attractive body that makes up for their low self-worth (McCarthy 1990). Additionally, the smaller predictive effect of depressive symptoms in later assessments may reflect the decline in statistical power due to sample attrition –although the sample size was moderate even at T4 (N = 476)– or the increasing stability in disordered eating over time –so that less variance in this outcome was left to explain as youth grew older.
The lack of a predictive effect of disordered eating on depressive symptoms casts doubt on the hypothesis that eating pathology itself is a harbinger of affective disturbances (e.g., Stice et al. 2000). This evidence is contrary to that of some analogous studies (Marmorstein et al. 2008; Presnell et al. 2009; Skinner et al. 2012; Stice et al. 2004), although the inconsistency may have partly arisen because most of these studies focused on bulimic symptoms (Presnell et al. 2009; Skinner et al. 2012; Stice et al. 2004). In this respect, the bulimotypic features of binge eating and purging may be particularly damaging for emotional adjustment because they probably elicit shame and guilt (Stice et al. 2000), whereas a broader constellation of eating problems including anorexic-like behaviors may temporarily result in effective weight loss and a sense of personal control (Fairburn et al. 1999). The null findings may also be related to the developmental period investigated, the time lag between follow-ups, or the analytic approach. For instance, given that the peak risk of developing full-blown eating disorders extends into late adolescence and young adulthood (Hoek and van Hoeken 2003), eating pathology may be unlikely to carry a true emotional burden before such developmental phases. Alternatively, the influence of disordered eating on mood may occur in the short term and then fade, which may help explain why some studies with shorter inter-assessment periods yielded a significant relationship between bulimic symptoms and later depressive symptoms (Presnell et al. 2009; Stice et al. 2004). Finally, the use of a conservative analytic technique may also have favored non-significant results, as indicated in a methodologically similar study (Stice 1998).
One important novelty of this study was the use of a sample of girls and boys. Interestingly, gender was not found to moderate any of the paths linking depressive symptoms and disordered eating. Thus, our results support the notion that the relationship between depressive symptoms and disordered eating is essentially the same across genders, as pointed out by other authors (Hautala et al. 2008; Santos et al. 2007; Vaughan and Halpern 2010). In particular, depressive symptoms at T1 posed a similar risk of engaging in disordered eating at T2 in girls and boys. This parallels some evidence indicating that depression in adolescence increases the risk of eating pathology regardless of gender (Johnson et al. 2002), but contradicts the results of other studies showing that affective disturbances are a female-specific predictor of eating problems (Beato-Fernández et al. 2007; Jackson and Chen 2008) –although these studies analyzed girls and boys separately rather than conducting formal, more restrictive moderator tests (Whisman and McClelland 2005). In any case, girls surpassed boys in mean levels of depressive symptoms and disordered eating from T3 and T2, respectively, which suggests that some factors omitted in the current study may selectively jeopardize girls’ wellbeing across early to mid-adolescence. However, it may not be that risk factors for depression and eating problems work differently for girls and boys, but simply that girls have higher levels of such risk factors (Hautala et al. 2008; Vaughan and Halpern 2010).
Although the main interest of this study was in the cross-lagged relations between psychopathological domains, our findings also yield relevant data concerning the stability of each outcome. Depressive symptoms were fairly stable over time, with the highest level of stability between T3 and T4. Likewise, other studies have indicated that depressive symptomatology in youth remains relatively stable over a 2-year period (Devine et al. 1994; DuBois et al. 1995; Holsen et al. 2000). It should be noted that depressive symptoms were already rather stable by early adolescence, which implies that subclinical affective disturbances prior to adolescence may be more persistent and deleterious than previously thought. Furthermore, there were no gender differences in the stability of depressive symptoms, which is in keeping with recent evidence (Tram and Cole 2006). With respect to disordered eating, the stability ranged from moderate to large, with increasing estimates as youth progressed through adolescence. Comparable estimates of 2-year stability have been reported in other studies with adolescents (Leon et al. 1995; Wichstrøm 2000). Moreover, our results resemble previous evidence that disordered eating is more stable in older girls than their younger peers (Wertheim et al. 2001), thus suggesting increasing chronicity with age. On the contrary, the absence of gender differences in the stability of disordered eating contrasts with some findings supportive of greater stability in girls than boys (Leon et al. 1995; Wichstrøm 2000). This inconsistency may be partly due to differences in the study design, the aspects of eating problems addressed, and the sample characteristics, but it is also possible that eating problems are becoming less transient among boys because of increasing pressures on boys to attain idealized bodies (e.g., Darcy 2011).
Strengths, Limitations, and Future Prospects
As far as we know, the current investigation is the first prospective study exploring the bidirectional association between depressive symptoms and disordered eating in a sample of girls and boys. The strengths of this study include the recruitment of a large community sample of adolescents, which maximizes the generalizability of the results; the multiwave design, which allowed a comprehensive developmental approach; the use of latent variables, thus controlling for measurement error; and the application of an appropriate analytic technique that tested the relationship between depressive symptoms and disordered eating in a unique, parsimonious model.
Despite these assets, there are also several limitations worth noting. First, the participants were Spanish and predominantly Caucasian. Therefore, caution is needed in extrapolating the data to other countries and ethnic groups. Second, younger participants were slightly overrepresented in later assessments because of selective attrition with respect to age. Thus, this may have introduced some sort of systematic errors in the results pertaining to T3 and T4. Third, the study relied solely on self-reports. Hence, some response biases may have affected the findings. Fourth, the measures used do not correspond to diagnosable depression or eating disorders. Consequently, the results cannot be directly generalized to the interplay between clinical disorders. Fifth, disordered eating was treated as a single latent construct. This implies that different associations between specific disordered eating symptoms (dieting, binge eating, purging, etc.) and depressive symptoms could have been obscured. Similarly, the disordered eating construct on which this study was based does not specifically capture those behaviors designed to enhance muscularity, which may be a salient eating-related problem among boys (Labre 2002). Finally, potentially relevant variables that may act as confounders of the relationship between depressive symptoms and disordered eating were not controlled for in the model. This is particularly true with respect to those variables that appear to be associated with both outcomes, such as body dissatisfaction (Johnson and Wardle 2005; Stice and Shaw 2002) and Body Mass Index (Loth et al. 2011; Neumark-Sztainer and Hannan 2000).
Future studies seeking to elucidate the relationship between depression and eating problems should target different populations, such as clinical samples, adults, and participants from diverse locations and ethnic backgrounds. Because the optimal time lag for examining the association between depressive symptoms and disordered eating is unknown, another recommendation is replication of the current study with different time intervals between assessments. Finally, a necessary further step to gain a better understanding of the interplay between depressive and eating psychopathology involves examination of the variables that may underlie their relationship. For instance, it would be of interest to investigate whether the link between depressive symptoms and later disordered eating is mediated by several factors (e.g., body dissatisfaction) or whether eating problems predict depressive symptoms in the presence of some moderator variables (e.g., failure to control weight).
Theoretical and Clinical Implications
This investigation has both theoretical and clinical implications. On a theoretical basis, our findings shed some light on the etiological associations between depressive symptoms and disordered eating. Specifically, the results illustrate a unidirectional, age-specific effect whereby depressive symptoms in preadolescence trigger the development of disordered eating in early adolescence. The findings also demonstrate that both disturbances are considerably stable by early adolescence, although there is a tendency that depressive symptoms and particularly disordered eating are more stable in older adolescents. Moreover, girls and boys are apparently more alike than different regarding the relationship between depressive symptoms and disordered eating and the extent to which each construct remains stable over time.
From a clinical point of view, our results suggest that prevention and treatment of depression in preadolescence may be effective in reducing eating pathology in early adolescence, whereas the reverse may be of little avail. In this respect, there is evidence that a brief prevention program for depression produces decreases in depressive symptoms as well as in bulimic tendencies among female students (Burton et al. 2007). However, our results indicate that these interventions should target both girls and boys. Finally, public health policies should also promote the implementation of preventive strategies for these disturbances at early stages of development because both depressive symptoms and disordered eating appear to be relatively stable in early adolescence.
References
Ackard, D. M., Fulkerson, J. A., & Neumark-Sztainer, D. (2011). Psychological and behavioral risk profiles as they relate to eating disorder diagnoses and symptomatology among a school-based sample of youth. International Journal of Eating Disorders, 44, 440–446.
Alonso, J., Angermeyer, M. C., Bernert, S., Bruffaerts, R., Brugha, T. S., Bryson, H., et al. (2004). Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica, 109, 21–27.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author.
Bearman, S. K., & Stice, E. (2008). Testing a gender additive model: the role of body image in adolescent depression. Journal of Abnormal Child Psychology, 36, 1251–1263.
Beato-Fernández, L., Rodríguez-Cano, T., Pelayo-Delgado, E., & Calaf, M. (2007). Are there gender-specific pathways from early adolescence psychological distress symptoms toward the development of substance use and abnormal eating behavior? Child Psychiatry and Human Development, 37, 193–203.
Burton, E., Stice, E., Bearman, S. K., & Rohde, P. (2007). Experimental test of the affect-regulation theory of bulimic symptoms and substance use: a randomized trial. International Journal of Eating Disorders, 40, 27–36.
Cafri, G., Thompson, J. K., Ricciardelli, L., McCabe, M., Smolak, L., & Yesalis, C. (2005). Pursuit of the muscular ideal: Physical and psychological consequences and putative risk factors. Clinical Psychology Review, 25, 215–239.
Chamay-Weber, C., Narring, F., & Michaud, P.-A. (2005). Partial eating disorders among adolescents: a review. Journal of Adolescent Health, 37, 417–427.
Coffman, D. L., & MacCallum, R. C. (2005). Using parcels to convert path analysis models into latent variable models. Multivariate Behavioral Research, 40, 235–259.
Cole, D. A., & Maxwell, S. E. (2003). Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112, 558–577.
Craighead, W. E., Curry, J. F., & Ilardi, S. S. (1995). Relationship of children’s depression inventory factors to major depression among adolescents. Psychological Assessment, 7, 171–176.
Darcy, A. M. (2011). Eating disorders in adolescent males: a critical examination of five common assumptions. Adolescent Psychiatry, 1, 307–312.
del Barrio, M. V., Moreno, C., & López, R. (1999). El Children’s Depression Inventory (CDI; Kovacs, 1992). Su aplicación en población española [The Children’s Depression Inventory (CDI; Kovacs, 1992) in a Spanish sample]. Clínica y Salud, 10, 393–416.
Devine, D., Kempton, T., & Forehand, R. (1994). Adolescent depressed mood and young adult functioning: a longitudinal study. Journal of Abnormal Child Psychology, 22, 629–640.
DuBois, D. L., Felner, R. D., Bartels, C. L., & Silverman, M. M. (1995). Stability of self-reported depressive symptoms in a community sample of children and adolescents. Journal of Clinical Child Psychology, 24, 386–396.
Fairburn, C. G., Shafran, R., & Cooper, Z. (1999). A cognitive behavioural theory of anorexia nervosa. Behaviour Research and Therapy, 37, 1–13.
Ferreiro, F., Seoane, G., & Senra, C. (2011). A prospective study of risk factors for the development of depression and disordered eating in adolescents. Journal of Clinical Child & Adolescent Psychology, 40, 500–505.
Ferreiro, F., Seoane, G., & Senra, C. (2012). Gender-related risk and protective factors for depressive symptoms and disordered eating in adolescence: A 4-year longitudinal study. Journal of Youth and Adolescence, 41, 607–622.
Franklin, J. C., Schiele, B. C., Brozek, J., & Keys, A. (1948). Observations on human behavior in experimental semistarvation and rehabilitation. Journal of Clinical Psychology, 4, 28–45.
Fulkerson, J. A., Sherwood, N. E., Perry, C. L., Neumark-Sztainer, D., & Story, M. (2004). Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Preventive Medicine, 38, 865–875.
Godart, N. T., Perdereau, F., Rein, Z., Berthoz, S., Wallier, J., Jeammet, P., et al. (2007). Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. Journal of Affective Disorders, 97, 37–49.
Gotlib, I. H., Lewinsohn, P. M., & Seeley, J. R. (1995). Symptoms versus a diagnosis of depression: differences in psychosocial functioning. Journal of Consulting and Clinical Psychology, 63, 90–100.
Hankin, B. L., Abramson, L. Y., Moffitt, T. E., Silva, P. A., McGee, R., & Angell, K. E. (1998). Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology, 107, 128–140.
Hautala, L. A., Junnila, J., Helenius, H., Väänänen, A.-M., Liuksila, P.-R., Räihä, H., et al. (2008). Towards understanding gender differences in disordered eating among adolescents. Journal of Clinical Nursing, 17, 1803–1813.
Hautala, L., Helenius, H., Karukivi, M., Maunula, A.-M., Nieminen, J., Aromaa, M., et al. (2011). The role of gender, affectivity and parenting in the course of disordered eating: a 4-year prospective case–control study among adolescents. International Journal of Nursing Studies, 48, 959–972.
Heatherton, T. F., & Baumeister, R. F. (1991). Binge eating as escape from self-awareness. Psychological Bulletin, 110, 86–108.
Hoek, H. W., & van Hoeken, D. (2003). Review of the prevalence and incidence of eating disorders. International Journal of Eating Disorders, 34, 383–396.
Holsen, I., Kraft, P., & Vittersø, J. (2000). Stability in depressed mood in adolescence: results from a 6-year longitudinal panel study. Journal of Youth and Adolescence, 29, 61–78.
Instituto Galego de Estatística. (2010). Galicia en cifras: anuario 2009 [Galicia’s figures: 2009 yearbook]. Online document. Xunta de Galicia. http://www.ige.eu/estatico/html/gl/galicia_en_cifras/galicia_2009/gcifras_2009_c00.pdf. Accessed 28 June 2013
Jackson, T., & Chen, H. (2008). Predicting changes in eating disorder symptoms among adolescents in China: an 18-month prospective study. Journal of Clinical Child & Adolescent Psychology, 37, 874–885.
Johnson, F., & Wardle, J. (2005). Dietary restraint, body dissatisfaction, and psychological distress: a prospective analysis. Journal of Abnormal Psychology, 114, 119–125.
Johnson, J. G., Cohen, P., Kotler, L., Kasen, S., & Brook, J. S. (2002). Psychiatric disorders associated with risk for the development of eating disorders during adolescence and early adulthood. Journal of Consulting and Clinical Psychology, 70, 1119–1128.
Keel, P. K., Fulkerson, J. A., & Leon, G. R. (1997). Disordered eating precursors in pre- and early adolescent girls and boys. Journal of Youth and Adolescence, 26, 203–216.
Kessler, R. C., & Walters, E. E. (1998). Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depression and Anxiety, 7, 3–14.
Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd ed.). New York: Guilford Press.
Kovacs, M. (1992). The Children’s Depression Inventory (CDI). Manual. Toronto: Multi Health Systems.
Labre, M. P. (2002). Adolescent boys and the muscular male body ideal. Journal of Adolescent Health, 30, 233–242.
Leon, G. R., Fulkerson, J. A., Perry, C. L., & Early-Zald, M. B. (1995). Prospective analysis of personality and behavioral vulnerabilities and gender influences in the later development of disordered eating. Journal of Abnormal Psychology, 104, 140–149.
Leon, G. R., Fulkerson, J. A., Perry, C. L., Keel, P. K., & Klump, K. L. (1999). Three to four year prospective evaluation of personality and behavioral risk factors for later disordered eating in adolescent girls and boys. Journal of Youth and Adolescence, 28, 181–196.
Lewinsohn, P. M., Striegel-Moore, R. H., & Seeley, J. R. (2000). Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 1284–1292.
Linde, J. A., Wall, M. M., Haines, J., & Neumark-Sztainer, D. (2009). Predictors of initiation and persistence of unhealthy weight control behaviours in adolescents. International Journal of Behavioral Nutrition and Physical Activity, 6, 72–81.
Loth, K. A., Mond, J., Wall, M., & Neumark-Sztainer, D. (2011). Weight status and emotional well-being: Longitudinal findings from project EAT. Journal of Pediatric Psychology, 36, 216–225.
Maloney, M. J., McGuire, J. B., & Daniels, S. R. (1988). Reliability testing of a children’s version of the eating attitude test. Journal of the American Academy of Child & Adolescent Psychiatry, 27, 541–543.
Marmorstein, N. R., von Ranson, K. M., Iacono, W. G., & Malone, S. M. (2008). Prospective associations between depressive symptoms and eating disorder symptoms among adolescent girls. International Journal of Eating Disorders, 41, 118–123.
Maxwell, M. A., & Cole, D. A. (2009). Weight change and appetite disturbance as symptoms of adolescent depression: toward an integrative biopsychosocial model. Clinical Psychology Review, 29, 260–273.
McCarthy, M. (1990). The thin ideal, depression and eating disorders in women. Behaviour Research and Therapy, 28, 205–215.
Measelle, J. R., Stice, E., & Hogansen, J. M. (2006). Developmental trajectories of co-occurring depressive, eating, antisocial, and substance abuse problems in female adolescents. Journal of Abnormal Psychology, 115, 524–538.
Neumark-Sztainer, D., & Hannan, P. J. (2000). Weight-related behaviors among adolescent girls and boys: Results from a national survey. Archives of Pediatrics & Adolescent Medicine, 154, 569–577.
Neumark-Sztainer, D., Wall, M., Guo, J., Story, M., Haines, J., & Eisenberg, M. (2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? Journal of the American Dietetic Association, 106, 559–568.
Neumark-Sztainer, D., Wall, M., Story, M., & Standish, A. R. (2012). Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. Journal of Adolescent Health, 50, 80–86.
Nolen-Hoeksema, S., Stice, E., Wade, E., & Bohon, C. (2007). Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology, 116, 198–207.
Presnell, K., Stice, E., Seidel, A., & Madeley, M. C. (2009). Depression and eating pathology: Prospective reciprocal relations in adolescents. Clinical Psychology & Psychotherapy, 16, 357–365.
Procopio, C. A., Holm-Denoma, J. M., Gordon, K. H., & Joiner, T. E., Jr. (2006). Two-three-year stability and interrelations of bulimotypic indicators and depressive and anxious symptoms in middle-aged women. International Journal of Eating Disorders, 39, 312–319.
Rawana, J. S., Morgan, A. S., Nguyen, H., & Craig, S. G. (2010). The relation between eating- and weight-related disturbances and depression in adolescence: a review. Clinical Child and Family Psychology Review, 13, 213–230.
Santos, M., Richards, C. S., & Bleckley, M. K. (2007). Comorbidity between depression and disordered eating in adolescents. Eating Behaviors, 8, 440–449.
Satorra, A. (2000). Scaled and adjusted restricted tests in multi-sample analysis of moment structures. In R. D. H. Heijmans, D. S. G. Pollock, & A. Satorra (Eds.), Innovations in multivariate statistical analysis. A Festschrift for Heinz Neudecker (pp. 233–247). London: Kluwer Academic Publishers.
Senra, C., Seoane, G., Vilas, V., & Sánchez-Cao, E. (2007). Comparison of 10- to 12-year-old boys and girls using a Spanish version of the Children’s eating attitudes test. Personality and Individual Differences, 42, 947–957.
Simmons, R. G., Burgeson, R., Carlton-Ford, S., & Blyth, D. A. (1987). The impact of cumulative change in early adolescence. Child Development, 58, 1220–1234.
Skinner, H. H., Haines, J., Austin, S. B., & Field, A. E. (2012). A prospective study of overeating, binge eating, and depressive symptoms among adolescent and young adult women. Journal of Adolescent Health, 50, 478–483.
Smolak, L., & Levine, M. P. (1994). Psychometric properties of the Children’s eating attitudes test. International Journal of Eating Disorders, 16, 275–282.
Spoor, S. T. P., Stice, E., Bekker, M. H. J., Van Strien, T., Croon, M. A., & Van Heck, G. L. (2006). Relations between dietary restraint, depressive symptoms, and binge eating: a longitudinal study. International Journal of Eating Disorders, 39, 700–707.
Steele, R. G., Little, T. D., Ilardi, S. S., Forehand, R., Brody, G. H., & Hunter, H. L. (2006). A confirmatory comparison of the factor structure of the Children’s Depression Inventory between European American and African American youth. Journal of Child and Family Studies, 15, 779–794.
Stice, E. (1998). Relations of restraint and negative affect to bulimic pathology: a longitudinal test of three competing models. International Journal of Eating Disorders, 23, 243–260.
Stice, E., & Bearman, S. K. (2001). Body-image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: a growth curve analysis. Developmental Psychology, 37, 597–607.
Stice, E., & Shaw, H. (2002). Role of body dissatisfaction in the onset and maintenance of eating pathology: a synthesis of research findings. Journal of Psychosomatic Research, 53, 985–993.
Stice, E., Shaw, H., & Nemeroff, C. (1998). Dual pathway model of bulimia nervosa: Longitudinal support for dietary restraint and affect-regulation mechanisms. Journal of Social and Clinical Psychology, 17, 129–149.
Stice, E., Hayward, C., Cameron, R. P., Killen, J. D., & Taylor, C. B. (2000). Body-image and eating disturbances predict onset of depression among female adolescents: A longitudinal study. Journal of Abnormal Psychology, 109, 438–444.
Stice, E., Burton, E. M., & Shaw, H. (2004). Prospective relations between bulimic pathology, depression, and substance abuse: Unpacking comorbidity in adolescent girls. Journal of Consulting and Clinical Psychology, 72, 62–71.
Thomas, K., Ricciardelli, L. A., & Williams, R. J. (2000). Gender traits and self-concept as indicators of problem eating and body dissatisfaction among children. Sex Roles, 43, 441–458.
Tram, J. M., & Cole, D. A. (2006). A multimethod examination of the stability of depressive symptoms in childhood and adolescence. Journal of Abnormal Psychology, 115, 674–686.
Tyrka, A. R., Waldron, I., Graber, J. A., & Brooks-Gunn, J. (2002). Prospective predictors of the onset of anorexic and bulimic syndromes. International Journal of Eating Disorders, 32, 282–290.
Vaughan, C. A., & Halpern, C. T. (2010). Gender differences in depressive symptoms during adolescence: the contributions of weight-related concerns and behaviors. Journal of Research on Adolescence, 20, 389–419.
Wertheim, E. H., Koerner, J., & Paxton, S. J. (2001). Longitudinal predictors of restrictive eating and bulimic tendencies in three different age groups of adolescent girls. Journal of Youth and Adolescence, 30, 69–81.
Whisman, M. A., & McClelland, G. H. (2005). Designing, testing, and interpreting interactions and moderator effects in family research. Journal of Family Psychology, 19, 111–120.
Wichstrøm, L. (1995). Social, psychological and physical correlates of eating problems. A study of the general adolescent population in Norway. Psychological Medicine, 25, 567–579.
Wichstrøm, L. (1998). Self-concept development during adolescence: Do American truths hold for Norwegians? In E. Skoe & A. von der Lippe (Eds.), Personality development in adolescence: A cross national and life span perspective (pp. 98–122). London: Routledge.
Wichstrøm, L. (2000). Psychological and behavioral factors unpredictive of disordered eating: A prospective study of the general adolescent population in Norway. International Journal of Eating Disorders, 28, 33–42.
Acknowledgments
The authors acknowledge financial support from the Ministry of Education (AP2008-01526) and the Ministry of Science and Innovation (PSI2010-19793) of the Spanish Government and from the Regional Ministry of Education and University Planning of the Galician Regional Government (PGIDIT05 CSO21101PR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ferreiro, F., Wichstrøm, L., Seoane, G. et al. Reciprocal Associations Between Depressive Symptoms and Disordered Eating Among Adolescent Girls and Boys: A Multiwave, Prospective Study. J Abnorm Child Psychol 42, 803–812 (2014). https://doi.org/10.1007/s10802-013-9833-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-013-9833-x