Abstract
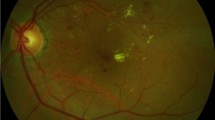
The aim of this study is to evaluate the effects of haemodialysis with a high ultrafiltration rate on the choroidal and retinal thickness of non-diabetic end-stage chronic renal failure (CRF) patients using optical coherence tomography (OCT). Twenty-one eyes of 21 male CRF patients aged between 46 and 80 years were included in this prospective study. Retinal and choroidal thicknesses of the patients were measured using high-resolution OCT line scans with the activated enhanced depth imaging mode before and shortly after haemodialysis. Retinal and choroidal thickness measurements were taken at the fovea and at two points that were 1,500 μm nasal and temporal to the fovea. The relationships between the haemodynamic changes, intraocular pressure (IOP) and central corneal thickness (CCT) were also evaluated. The mean choroidal thicknesses before haemodialysis at the subfoveal, temporal and nasal locations were 232.81 ± 71.92, 212.43 ± 70.50 and 182.14 ± 68.88 μm, respectively. The mean choroidal thicknesses after haemodialysis at the subfoveal, temporal and nasal locations were 210.90 ± 65.53, 195.38 ± 66.48 and 165.19 ± 66.73 μm, respectively. There were significant differences between the choroidal thicknesses before and after haemodialysis (p < 0.001 for all). The mean retinal thicknesses before haemodialysis at the foveal, temporal and nasal locations were 215.86 ± 41.06, 308.86 ± 37.73 and 338.00 ± 33.32 μm, respectively. The mean retinal thicknesses after haemodialysis at the foveal, temporal and nasal locations were 216.90 ± 39.70, 313.86 ± 32.89 and 335.29 ± 36.85 μm, respectively. There was no significant difference between the retinal thicknesses before and after haemodialysis (p > 0.05 for all). The mean CCT decreased insignificantly from 550.48 ± 17.46 to 548.10 ± 21.12 μm (p = 0.411). The mean IOP decreased significantly from 14.09 ± 2.58 to 12.54 ± 2.23 mmHg (p = 0.003), which did not correlate with the CCT [r = (−)0.134, p = 0.562]. Haemodialysis with a high ultrafiltration volume did not alter the retinal thickness but caused a significant choroidal thinning and an IOP decrease in non-diabetic end-stage CRF patients.

Similar content being viewed by others
References
Henderson LW (1980) Symptomatic hypotension during hemodialysis. Kidney Int 17(5):571–576
Mullaem G, Rosner MH (2012) Ocular problems in the patient with end-stage renal disease. Semin Dial 25(4):403–407
Tosun O, Davutluoglu B, Arda K, Boran M, Yarangumeli A, Kurt A, Ozkan D (2007) Determination of the effect of a single hemodialysis session on retrobulbar blood hemodynamics by color Doppler ultrasonography. Acta Radiol 48(7):763–767
Tokuyama T, Ikeda T, Sato K (1998) Effect of plasma colloid osmotic pressure on intraocular pressure during haemodialysis. Br J Ophthalmol 82(7):751–753
Dinc UA, Ozdek S, Aktas Z, Guz G, Onol M (2010) Changes in intraocular pressure, and corneal and retinal nerve fiber layer thickness during hemodialysis. Int Ophthalmol 30(4):337–340
Jung JW, Yoon MH, Lee SW, Chin HS (2012) Effect of hemodialysis (HD) on intraocular pressure, ocular surface, and macular change in patients with chronic renal failure : effect of hemodialysis on the ophthalmologic findings. Graefe’s Arch Clin Exp Ophthalmol. doi:10.1007/s00417-012-2032-6
Theodossiadis PG, Theodoropoulou S, Neamonitou G, Grigoropoulos V, Liarakos V, Triantou E, Theodossiadis GP, Vlahakos DV (2012) Hemodialysis-induced alterations in macular thickness measured by optical coherence tomography in diabetic patients with end-stage renal disease. Ophthalmologica 227(2):90–94
Auyanet I, Rodriguez LJ, Bosch E, Sanchez AY, Esparza N, Lago MM, Ramirez A, Checa MD (2011) Measurement of foveal thickness by optical coherence tomography in adult haemodialysis patients with diabetic nephropathy. Nefrologia 31(1):66–69
Inoue R, Sawa M, Tsujikawa M, Gomi F (2010) Association between the efficacy of photodynamic therapy and indocyanine green angiography findings for central serous chorioretinopathy. Am J Ophthalmol 149(3):441–446
Nagaoka T, Kitaya N, Sugawara R, Yokota H, Mori F, Hikichi T, Fujio N, Yoshida A (2004) Alteration of choroidal circulation in the foveal region in patients with type 2 diabetes. Br J Ophthalmol 88(8):1060–1063
Coleman DJ, Silverman RH, Chabi A, Rondeau MJ, Shung KK, Cannata J, Lincoff H (2004) High-resolution ultrasonic imaging of the posterior segment. Ophthalmology 111(7):1344–1351
Benavente-Perez A, Hosking SL, Logan NS, Bansal D (2010) Reproducibility-repeatability of choroidal thickness calculation using optical coherence tomography. Optom Vis Sci 87(11):867–872
Mountcastle VB, Milnor WR (1968) Capillaries and lymphatic vessels. In: Mountcastle VB (ed) Medical physiology, 12th edn. C.V. Mosby Co., St Louis, pp 134–149
Wallman J, Wildsoet C, Xu A, Gottlieb MD, Nickla DL, Marran L, Krebs W, Christensen AM (1995) Moving the retina: choroidal modulation of refractive state. Vis Res 35(1):37–50
Junghans BM, Crewther SG, Liang H, Crewther DP (1999) A role for choroidal lymphatics during recovery from form deprivation myopia? Optom Vis Sci 76(11):796–803
Nickla DL, Wallman J (2010) The multifunctional choroid. Prog Retin Eye Res 29(2):144–168
Converse RL Jr, Jacobsen TN, Toto RD, Jost CM, Cosentino F, Fouad-Tarazi F, Victor RG (1992) Sympathetic overactivity in patients with chronic renal failure. N Engl J Med 327(27):1912–1918
Chazot C, Jean G (2010) Intradialytic hypertension: it is time to act. Nephron Clin Pract 115(3):c182–c188
Sitprija V, Holmes JH, Ellis PP (1964) Changes in intraocular pressure during hemodialysis. Invest Ophthalmol 3:273–284
Leiba H, Oliver M, Shimshoni M, Bar-Khayim Y (1990) Intraocular pressure fluctuations during regular hemodialysis and ultrafiltration. Acta Ophthalmol (Copenh) 68(3):320–322
Doshiro A, Ban Y, Kobayashi L, Yoshida Y, Uchiyama H (2006) Intraocular pressure change during hemodialysis. Am J Ophthalmol 142(2):337–339
Austin JN, Klein M, Mishell J, Contiguglia SR, Levy J, Chan L, Shapiro JI (1990) Intraocular pressures during high-flux hemodialysis. Ren Fail 12(2):109–112
Perkovich BT, Meyers SM (1988) Systemic factors affecting diabetic macular edema. Am J Ophthalmol 105(2):211–212
Pahor D, Gracner B, Gracner T, Hojs R (2008) Optical coherence tomography findings in hemodialysis patients. Klin Monbl Augenheilkd 225(8):713–717
Fujiwara T, Imamura Y, Margolis R, Slakter JS, Spaide RF (2009) Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol 148(3):445–450
Disclosure
There is no funding/support from any institution for this study and none of the authors have any financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ulaş, F., Doğan, Ü., Keleş, A. et al. Evaluation of choroidal and retinal thickness measurements using optical coherence tomography in non-diabetic haemodialysis patients. Int Ophthalmol 33, 533–539 (2013). https://doi.org/10.1007/s10792-013-9740-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-013-9740-8