Abstract
Mastitis comprises an inflammation of the mammary gland, which is almost always linked with bacterial infection. The treatment of mastitis concerns antimicrobial substances, but not very successful. On the other hand, anti-inflammatory therapy with Chinese traditional medicine becomes an effective way for treating mastitis. Magnolol is a polyphenolic binaphthalene compound extracted from the stem bark of Magnolia sp., which has been shown to exert a potential for anti-inflammatory activity. The purpose of this study was to investigate the protective effects of magnolol on inflammation in lipopolysaccharide (LPS)-induced mastitis mouse model in vivo and the mechanism of this protective effects in LPS-stimulated mouse mammary epithelial cells (MMECs) in vitro. The damage of tissues was determined by histopathology and myeloperoxidase (MPO) assay. The expression of pro-inflammatory cytokines was determined by enzyme-linked immunosorbent assay (ELISA). Nuclear factor-kappa B (NF-κB), inhibitory kappa B (IκBα) protein, p38, extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and Toll-like receptor 4 (TLR4) were determined by Western blot. The results showed that magnolol significantly inhibit the LPS-induced TNF-α, IL-6, and IL-1β production both in vivo and vitro. Magnolol declined the phosphorylation of IκBα, p65, p38, ERK, and JNK in LPS-stimulated MMECs. Furthermore, magnolol inhibited the expression of TLR4 in LPS-stimulated MMECs. In vivo study, it was also observed that magnolol attenuated the damage of mastitis tissues in the mouse models. These findings demonstrated that magnolol attenuate LPS-stimulated inflammatory response by suppressing TLR4/NF-κB/mitogen-activated protein kinase (MAPK) signaling system. Thereby, magnolol may be a therapeutic agent against mastitis.
Similar content being viewed by others
INTRODUCTON
Mastitis refers to inflammation which is the normal defense reaction of the host immune system. Many different bacteria and fungi are known to cause mastitis, and Staphylococcus aureus and Streptococcus agalactiae are two of the most common species that have infected udder as main reservoir [1]. Moreover, Escherichia coli is considering correlation with mastitis, particularly around parturition or during early lactation [2]. Lipopolysaccharide (LPS), a major component of the outer membrane of gram-negative bacteria induces mouse or bovine mastitis models and causes the production of pro-inflammatory cytokines, which have proven to be invaluable tools for the study of coliform mastitis [3]. Mammary gland epithelial cells have shown the capacity to increase an inflammatory or active defense reaction in their own right mediated by cytokines [4]. While interacting with invading bacteria, mammary epithelial cells are able to generate multiple inflammatory cytokines as well as other immune cells [5]. Therefore, acute inflammatory response may cause tissue damages, and anti-inflammatory therapy is a crucial way to alleviate symptoms in mastitis.
The innate immune system is poised to rapidly respond to the earliest stages in infection through Toll-like receptors (TLRs) and other pattern recognition receptors (PRRs) [6]. TLR4, a key PRRs, ligated with LPS and recruited the downstream signaling pathway: NF-κB and mitogen-activated protein kinases (MAPKs) through receptor dimerization [7]. Activated NF-κB and MAPK signaling pathways regulated the inflammatory process by promoting the production of pro-inflammatory cytokines, such as tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) [8, 9]. Since severe inflammatory responses are representative features of mastitis and play a key role in the pathogenesis of tissue damage [10], any substances that inhibit the activation of TLR4 signaling pathways are considered as potential anti-inflammatory agents to prevent tissue damage during the development of mastitis.
Magnolol (5, 59-diallyl-2, 29-dihydroxybiphenyl) is a major component isolated from the stem bark of Magnolia sp. (Fig. 1), including Magnolia obovate and Magnolia officinalis [11]. It has been used to treat cough, diarrhea, and allergic rhinitis in China, Korea, and Japan [12]. Magnolol has been reported to suppress the overproduction of nitric oxide (NO) and TNF-α in LPS-stimulated macrophages [13], to decrease inflammatory cytokines production in THP-1 cells [14]. Recently, the mechanisms underlying the anti-inflammatory effect of magnolol have been reported. Fu et al. [15] confirmed that magnolol reveals an anti-inflammatory property by downregulating the activation of NF-κB and MAPK signaling pathways and the release of pro-inflammatory cytokines in LPS-stimulated macrophages RAW 264.7 cells. Thus, the objective of this study is to evaluate anti-inflammatory effect of magnolol using LPS-induced mastitis in mice then to investigate whether the effects are through the control of TLR4-mediated NF-kB and MPAK signaling pathways in LPS-stimulated mouse mammary epithelial cells (MMECs).
MATERIALS AND METHODS
Chemicals and Reagents
Magnolol (purity >98 %) was purchased from the National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China). Dimethyl sulfoxide (DMSO), LPS (E. coli 055:B5), and 3-(4, 5-dimethylthiazol-2-y1)-2, 5-diphenyltetrazolium bromide (MTT) were purchased from Sigma Chemical Co. (St. Louis, MO, USA). Dulbecco’s modified Eagle’s medium (DMEM F12/1:1) and fetal calf serum (FCS) and trypsin/EDTA were purchased from Hyclone (Logan, UT, USA). Collagenase I and II were purchased from Invitrogen Corp. (Carlsbad, California, USA). Epidermal growth factor (EGF), transferrin, and T3 were purchased from PeproTech. Dexamethasone (DEX) sodium phosphate injection (no. H41020055) was purchased from Changle Pharmaceutical Co. (Xinxiang, Henan, China). The myeloperoxidase (MPO) determination kit was purchased from the Jiancheng Bioengineering Institute of Nanjing (Nanjing, Jiangsu Province, China). Mouse TNF-α and IL-6 enzyme-linked immunosorbent assay (ELISA) kits were purchased from Biolegend (San Diego, CA, USA). All of the rabbit monoclonal antibodies and mouse monoclonal antibodies were purchased from Cell Signaling Technology Inc. (Beverly, MA, USA). Horseradish peroxidase-conjugated goat anti-rabbit and goat-mouse antibodies were provided by GE Healthcare (Buckinghamshire, UK). All other chemicals were of reagent grade.
In Vivo Study
Animals
BALB/c mice, 6–8 weeks old (18 male and 36 female), were purchased from the Center of Experimental Animals of Baiqiuen Medical College of Jilin University (Jilin, China). Mice were fed routinely for 2–3 days to fit the environment, and then one male and two female mice were housed in each cage with water and food supplied ad libitum. All mice were kept in a pathogen-free condition, with a 12-h light/dark cycle. The experiments followed the guidelines for the care and use of laboratory animals published by the US National Institutes of Health.
Mastitis Mouse Model and Grouping Design
The lactating mice, 5–7 days after birth of the offspring, were randomly divided into six groups: blank control group, LPS group, magnolol (5, 10, and 20 mg/kg) + LPS groups, and dexamethasone (DEX) + LPS group. Each group contained six mice. The establishment of mastitis mouse model was followed by Li et al. [16]. Briefly, the pups were removed 1 h before inducing inflammation of the mammary gland, then magnolol (5, 10, and 20 mg/kg) was given by intraperitoneal (i.p.) injection, and DEX (0.5 mg/kg) was used as a positive control. Blank control and LPS group mice were given an equal volume of sterile water intraperitoneally. After that, the lactating mice were anesthetized by urethane (15 g urethane dissolved in 150 ml physiological saline, 1.5 g/kg i.p.). A 100-μl syringe with a 30-gauge blunt needle was used to inoculate both L4 (on the left) and R4 (on the right) abdominal mammary glands. The anesthetized mice were laid on their backs under a binocular microscope. The teats and the surrounding area were prepped with 70 % ethanol. Each udder canal was exposed by a small cut at the near end of the teat and then challenged via teat canal catheterization with 10 μg of LPS dissolved in 50 μl non-pyrogenic phosphate-buffered saline (PBS). At 12 h after LPS infusion, the mice were killed using CO2 inhalation and mammary tissues were collected and stored at −80 °C until analysis.
Histopathological Examination
Mammary glands for histopathological examination were fixed in 10 % formalin for 48–72 h, dehydrated with graded alcohol and embedded in paraffin, and then stained with hematoxylin and eosin (H&E).
Myeloperoxidase Assay
The whole right mammary gland tissues were weighed and homogenized with PBS (1:9, w/v) on ice and then centrifuged (2,000g ×40 min at 4 °C). The supernatant was collected and centrifuged again (2,000g ×40 min at 4 °C) to remove any remaining lipid. MPO activity in homogenates was determined by the manufacturer’s instruction.
Enzyme-Linked Immunosorbent Assay
The preparation of tissue homogenates was the same to MPO assay, then the homogenate of mammary gland tissue samples was centrifuged to obtain the supernatant for analyzing the level of TNF-α, IL-1β, and IL-6 by ELISA kits in accordance with the manufacturer’s instructions.
In Vitro Study
Cell Culture and Treatment
Primary cultured MMECs were prepared as previously described by Smalley [17]. Briefly, mammary tissues were removed aseptically from 6–8 week-old gravid BALB/c mice and minced into pasties. The minced tissues were digested by collagenase I/II/trypsin mixture (Invitrogen, Carlsbad, California, USA) and shaken at 37 °C. After filtration, to remove unassociated tissue and debris, the cells were collected by centrifugation at 250g for 5 min three times. Cell pellets were resuspended in DMEM/F12 containing 10 % FCS and incubated for 1 h at 37 °C, then collected the supernatant. This step was repeated three times to clear away fibroblasts. After the last incubation, cells were resuspended in DMEM/F12 containing 10 % FCS, 0.5 % Transferrin, 0.1 % T3, and 0.5 % EGF and cultured at 37 °C with 5 % CO2. The medium was exchanged every day. For experiments, MMECs were stimulated with 1 μg/ml LPS alone or in the presence of various concentrations (12.5, 25, or 50 μg/ml) of magnolol. The magnolol stock solution was prepared with DMSO. The control cells were incubated for 24 h in the absence of LPS or magnolol.
MTT Assay for Cell Viability
Cell viability was measured using a standard MTT assay. MMECs were plated and incubated for 3 days in 96-well plate. Magnolol was dissolved in DMSO and the DMSO concentration in the assay did not exceed 0.1 %. Then various concentrations of magnolol (0, 12.5, 25, 50, 100, and 200 μg/ml) were added to the wells, followed by stimulation with 1 μg/ml of LPS for 18 h. Then, 20 μl MTT (5 mg/ml) was added to each well, and the cells were further incubated for an additional 4 h. The supernatants were removed and the formation of formazan was resolved with 150 μl/well of DMSO. The optical density was measured at 570 nm on a microplate reader (TECAN, Austria).
Enzyme-Linked Immunosorbent Assay
MMECs were seeded in 24-well plates and incubated in the presence of either LPS 1 μg/ml alone or LPS plus magnolol 12.5, 25, or 50 μg/ml for 18 h. Cell-free supernatants were subsequently employed for the proinflammatory cytokine assays using a mouse ELISA kit, according to the manufacturer’s instructions (BioLegend, Inc, San Diego, CA, USA).
Western Blot Analysis
MMECs were incubated, then pretreated with various concentrations of magnolol for 1 h and then stimulated with LPS (1 μg/ml) for 1 h. The control and magnolol-treated cells were washed triple with cold PBS and total proteins from cells were extracted by M-PER Mammalian Protein Extraction Reagent (Thermo Scientific, USA). Protein concentration was determined by bicinchoninic acid (BCA) method. The protein concentrations in supernatants were determined, and aliquots of protein (20 μg) were separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto a nitrocellulose membrane. The membrane was blocked with 5 % skim milk in Tris-buffered saline with Tween 20 (TBS-T) for 1 h and then incubated with various primary antibodies: phospho-IκBα, NF-κB p65, phospho-extracellular signal-regulated kinase (ERK)1/2, phospho-c-Jun N-terminal kinase (JNK), or phospho-p38 and β-actin at 4 °C overnight. Subsequently, the membrane was washed five times with TBS-T for 10 min and incubated with the secondary antibody conjugated with horseradish peroxidase at room temperature for 1 h. The membrane was again washed three times for 10 min with TBS-T, and finally, the results were visualized by using an enhanced chemiluminescence (ECL) Western blotting kit (Thermo Scientific, USA) and tested by ECL Plus Western Blotting Detection System (Amersham Life Science, UK).
Statistical Analysis
All of the data are expressed as the mean ± SEM. The differences among the various experimental groups were analyzed by a one-way ANOVA (Dunnett’s t test) and a two-tailed Student’s t test. P < 0.05 was considered to be statistically significant.
RESULTS
In Vivo Study
Histopathological Findings of Mammary Gland Tissues
Mammary gland tissues in different groups were harvested at 12 h after LPS challenge for evaluating the pathological changes. The mammary gland sections were subjected to H&E staining. There was no pathological change observed in blank control group (Fig. 2a). In LPS group (Fig. 2b), the mice exhibited obvious increase in inflammatory cell infiltration, containing neutrophils, macrophages, etc., and the construction of mammary gland tissues were significantly damaged, including interstitial edema and thickening of the alveolus wall. However, these pathological changes were relieved in DEX group (Fig. 2c) and magnolol treatment groups with the doses of 5 mg/kg (Fig. 2d), 10 mg/kg (Fig. 2e), and 20 mg/kg (Fig. 2f).
Effect of Magnolol on MPO Activity
MPO activity is a measure of mammary gland parenchymal phagocyte infiltration [18] as well as cytokines. The MPO activity of mammary glands in LPS group was obviously raised, compared with the blank control group. Treatment of magnolol at a dose of 5 mg/kg could not noticeably reduce the MPO activity, while significantly decline of MPO activity was appeared at doses of 10 and 20 mg/kg, compared with the LPS group. Meanwhile, the MPO activity of mammary gland tissue in DEX treatment group was significantly decreased, compared with the LPS group (Fig. 3).
Myeloperoxidase (MPO) activity assay. MPO activity in mammary tissue from blank control group, LPS group, and treatment groups administered 5, 10, and 20 mg/kg magnolol and 5 mg/kg DEX. Data are presented as mean ± SEM (n = 6). # p < 0.01 significantly different from blank control group; *p < 0.05; ** p < 0.01 significantly different from LPS group.
Magnolol Dose-Dependently Suppresses Pro-inflammatory Cytokine Production in LPS-Induced Mouse Mastitis
To evaluate the levels of cytokines in the tissue homogenate of LPS-induced mammary gland, the mammary gland was collected 12 h after LPS challenge. The level of TNF-α, IL-1β, and IL-6 were measured by ELISA. The above pro-inflammatory cytokines in LPS group were significantly increased compared with those in blank control group. However, magnolol inhibited the expression of TNF-α, IL-1β, and IL-6 in a dose-dependent manner, and DEX significantly reduced the expression of those compared to that in the LPS group (Fig. 4).
Cytokine assay. TNF-α, IL-1β, and IL-6 levels in mammary tissue from blank control group, LPS group and treatment groups administered magnolol 5, 10, and 20 mg/kg and 5 mg/kg DEX. Data represent the contents of 1 ml supernatant of mammary homogenate and are presented as mean ± SEM (n = 6). # p < 0.01 significantly different from blank control group; *p < 0.05; **p < 0.01 significantly different from LPS group.
In Vitro Study
Effects of Magnolol on Cell Viability of MMECs
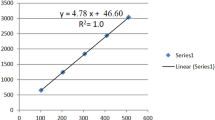
The potential cytotoxicity of magnolol was examined by MTT assay in the presence or absence of LPS (1 μg/ml) to determine the effective concentration for treatment. Cells were treated with various magnolol concentrations (0, 12.5, 25, 50, 100, and 200 μg/ml) and co-treated LPS (1 μg/ml) for 18 h. The results showed that LPS (1 μg/ml) and the concentrations of magnolol at 12.5, 2,5 and 50 μg/ml were not attributable to cytotoxic effects (Fig. 5).
Effects of magnolol on LPS-stimulated cell viability in MMECs. MMECs were treated with the different concentrations of magnolol (0, 12.5, 25, 50, 100, and 200 μg/ml) in the absence or presence of 1 μg/ml LPS for 18 h. Cell viability was assessed by MTT assay. The values are presented as mean ± SEM of three independent experiments.
Magnolol Dose-Dependently Represses Pro-inflammatory Cytokine Production in LPS-Stimulated MMECs
To determine the effects of magnolol on TNF-α and IL- 6 production by LPS-stimulated MMECs, ELISA analyses were conducted. Cells were pretreated with magnolol at different concentrations (12.5, 25, or 50 μg/ml), then stimulated with LPS, and the levels of TNF-α and IL-6 were measured by ELISA. As shown in Fig. 6, the group treatment with LPS showed significantly increased production of pro-inflammatory cytokines in culture supernatants of MMECs compared with the control group, while treatment with magnolol at concentrations of 12.5, 25, or 50 μg/ml showed markedly inhibited production of TNF-α, IL-1β, and IL-6 in LPS-stimulated MMECs (Fig. 6). Specially, magnolol showed a strong suppressive effect on the production of TNF-α, IL-1β, and IL-6 at concentration of 50 μg/ml, respectively, which indicated that magnolol inhibits the production of these proinflammatory cytokines involved in the inflammation process in a dose-dependent manner.
Magnolol inhibits LPS-stimulated cytokine production in a dose-dependent manner. Cells were treated with 1 μg/ml LPS in absence or presence of magnolol (12.5, 25, or 50 μg/ml) for 18 h. Levels of TNF-α and IL-6 in culture supernatants were measured by ELISA. The values presented are the mean ± SEM of three independent experiments. # p < 0.01 vs. the control group; *p < 0.05; **p < 0.01 vs. the LPS group.
Magnolol Inhibits the Degradation and Phosphorylaton of NF-κB Pathway in LPS-Stimulated MMECs
NF-κB regulates both innate and adaptive immune responses. It is activated rapidly in response to a wide range of stimuli, including pathogens, stress signals, and proinflammatory cytokines, such as LPS and TNF-α [19]. In order to evaluate the inhibitory effect of magnolol on NF-κB signaling pathway, the expression of phosphorylated-p65 and degraded-IκBα in LPS-stimulated MMECs, which pretreated with magnolol, were examined by Western blot analysis. In Fig. 7, the phosphorylation of p65 after LPS treatment was dramatically inhibited by magnolol in a dose-dependent manner when compared with the control group. Furthermore, IκB α was markedly degraded after treatment with LPS, whereas treatment with magnolol prevented this degradation in a dose-dependent manner. These data suggest that magnolol may block the activation of NF-κB signaling in LPS-stimulated MMECs.
Magnolol inhibits LPS-stimulated activation of NF-κB (p65), the degradation of IκBα, and the expression of TLR4. Cells were treated with various concentrations (12.5, 25, or 50 μg/ml) of magnolol for 1 h, followed by continuous incubation with or without LPS (1 μg/ml) for the next 1 h. Cell lysates were analyzed by the Western blot analysis using specific antibodies. β-actin was used as a control. The values presented are the mean ± SEM of three independent experiments. # p < 0.01 vs. the control group; *p < 0.05; **p < 0.01 vs. the LPS group.
Magnolol Suppresses the Phosphorylation of ERK, JNK, and p38 MAPKs in LPS-Stimulated MMECs
MAPK proteins play critical roles in the induction of pro-inflammatory mediators, such as TNF-α and IL-6 as well as in the activation of transcription factors, such as NF-κB [20]. Thus, MAPK signaling pathways provide specific targets for inflammatory responses. To confirm whether MAPKs are involved in the inhibition of proinflammatory cytokines production by magnolol, phosphorylation of ERK, JNK, and p38 MAPKs in LPS-stimulated MMECs (pretreatment with magnolol) was examined by Western blot. As shown in Fig. 8, LPS treatment caused a strong increase in the phosphorylation of ERK, JNK, and p38MAPKs. However, co-treatment with various concentrations of magnolol reduced the levels of all MAPK phosphorylations. Especially, magnolol significantly inhibited the activities of ERK MAPKs in a dose-dependent manner (Fig. 8). These suggests that magnolol decrease the phosphorylation of ERK, JNK, and p38 MAPKs in LPS-stimulated MMECs.
Magnolol inhibits LPS-stimulated MAPK activation. Cells were pretreated with magnolol (12.5, 25, or 50 μg/ml) for 1 h and then treated with 1 μg/ml LPS for 1 h. Protein samples were analyzed by Western blot with specific antibodies. β-actin was used as a control. The values presented are the mean ± SEM of three independent experiments. # p < 0.01 vs. the control group; *p < 0.05; **p < 0.01 vs. the LPS group.
Magnolol Reduces the Expression of TLR4 in LPS-Stimulated MMECs
TLR4 signaling plays a vital role in inflammatory response. Activation of TLR4 signaling by LPS induces the production of inflammatory cytokines through the activation of NF-κB and MAPK signaling pathways. To investigate whether magnolol affect TLR4 signaling, the expression of TLR4 was determined by Western blot. The results showed that magnolol downregulated the expression of TLR4 in LPS-stimulated MMECs in a dose-dependent manner (Fig. 7).
DISCUSSION
Mastitis is defined as an inflammation of the mammary gland. It usually occurs primarily in response to intramammary bacterial infection, but also to intramammary mycoplasmal, fungal, or algal infections [21]. Bovine mastitis is a major disease affecting dairy cattle worldwide and is a costly disease for dairy producers [22]. But in recent years, conventional methods have frequently been unable to prevent intramammary infection, antibiotics are not very effective in the treatment of mastitis and have a negative impact on human health [23]. Mammary epithelial cells, the most numerous cells in the mammary gland, are parts of the functional unit of the udder, which are responsible for the synthesis of many components in milk that provide nutritional and immunological support to the offspring [24]. Moreover, experiments with LPS-stimulated mastitis in rats suggest that large-scale production of proinflammatory cytokines, such as TNF-α, might contribute to tissue damage [25]. Many traditional Chinese medicines (TCM) extracts has been verified to have anti-inflammatory properties on mastitis [26, 27]. Magnolol has been reported the anti-inflammatory effect [28] and our lab further found that the role of magnolol mainly by downregulated the expression of TLR4 and thus attenuated TLR4-mediated activation of NF-κB and MAPK signaling and release of proinflammatory cytokines in LPS-stimulated macrophages RAW 264.7 cells [15]. Thus, in the present study, we evaluated the anti-inflammatory effects of magnolol in LPS-induced mastitis and elucidated the potential anti-inflammatory mechanism.
In vivo, histopathological observation indicated that magnolol markedly inhibited the infiltration of inflammatory cells and decreased mammary damage. Some cytokines were responsible for the damage of mammary gland tissues, such as TNF-α and IL-1β [29], and the results of cytokines assay were proved that in this study, magnolol inhibited the secretion of TNF-α, IL-6, and IL-1β in LPS-induced mastitis mouse model. The above results were consistent with MPO activity assay. MPO activity, a marker of neutrophil influx into tissue, is directly proportional to the number of neutrophils in the tissue [30]. As shown in Fig. 3, we confirmed that pretreatment with magnolol significantly reduced the MPO activity of mammary gland and decreased mammary neutrophilia. Accordingly, it is proposed that magnolol could reduce the inflammatory cell infiltration and decrease mammary damage through inhibiting the production of pro-inflammatory cytokines.
In vitro, we further confirmed the effects of magnolol in anti-inflammation by LPS-stimulated MMECs. Proinflammatory cytokines, such as IL-1β, IL-2, IL-6, IL-10, and TNF-α, are crucial mediators in a range of acute and chronic responses to inflammatory diseases, while TNF-α and IL-6, as the principal proinflammatory cytokines, are involved in the pathophysiology of endotoxin-induced mastitis, increase the expression of adhesion molecules, and trigger the production of reactive oxygen species (ROS) [31–34]. Accordingly, in this study, we first investigated the suppressive effect of magnolol on the production of TNF-α and IL-6 in LPS-stimulated MMECs by ELISA. Moreover, we checked the potential cytotoxicity of magnolol using MTT assay; magnolol did not affect the viability of MMECs, up to a concentration of 50 μg/ml (Fig. 5). The following experiments were in accordance with this concentration. The ELISA results showed that the production of TNF-α and IL-6 in LPS-stimulated MMECs was decreased by various concentrations of magnolol (12.5, 25, or 50 μg/ml) in a dose-dependent manner (Fig. 6). These findings indicated that the inhibitory effect of magnolol on TNF-α and IL-6 have important implications for decreasing the inflammatory response.
NF-κB, a main regulatory transcription factor, exists as homo-dimeric or hetero-dimeric complexes of p50 and p65 subunits bound to IκB and plays a key role in cellular responses to various stimuli such as stress, cytokines, free radicals, ultraviolet radiation, oxidized LDL, and bacterial or viral antigens [35]. Upon stimulation, activated IκBα kinase phosphorylates IκBα and phosphorylated IκBα are ubiquitinated and degraded through proteasome pathway and made the phosphorylation of NF-κB p65. Activated NF-κB induces the expression of numerous genes involved in innate and adaptive immune regulation, inflammatory responses, cell adhesion, osteogenesis, and anti-apoptosis [36, 37]. Thus, it is not surprising that the inhibition of NF-κB regulation is closely associated with inflammatory responses. In addition, it is well known that various natural herbs are responsible for anti-inflammatory responses via the suppression of NF-κB signaling pathway [38, 39]. Thus, in this study, we investigated whether magnolol inhibits the phosphorylation of NF-κB p65 and degradation of IκBα protein by Western blot. The data showed that LPS-stimulated phosphorylation of p65 was blocked by magnolol in a dose-dependent manner through the inhibition of IκBα degradation (Fig. 7). The results demonstrated that magnolol may inhibit the production of TNF-α and IL-6 via inhibition of NF-κB by blocking IκBα degradation and p65 phosphorylation.
Mitogen-activated protein kinase (MAPK) signaling pathways, comprised of three MAP kinase cascades (extracellular signal-regulated kinases (ERKs), c-Jun NH2-terminal kinases (JNKs,) and p38 MAP kinase), present in all eukaryotic cells. Upon activation of the MAP kinases, transcription factors present within the cytoplasm or nucleuses are phosphorylated and activated, leading to expression of target genes resulting in a biological response, including the regulation of proinflammatory mediator expression [40]. Thus, we investigated the effect of magnolol on the phosphorylation of ERK, JNK, and p38MAPKs in LPS-stimulated MMECs by Western blot. The results showed that magnolol reduced the production of proinflammatory cytokines in MMECs maybe by suppressing the MAPK signaling pathway, including the inhibition of the phosphorylation of ERK, JNK, and p38MAPKs (Fig. 8).
TLR4 is a pattern recognition receptor; it responds to LPS and triggers the activation of NF-κB and MAPK signaling pathways. The latter regulates the release of proinflammatory cytokines [41]. We investigated whether the anti-inflammatory activity of magnolol exerted though TLR4-mediated signaling in LPS-stimulated MMECs by Western blot. Our results showed that magnolol inhibits the expression of TLR4 in LPS-stimulated MMECs (Fig. 7). Based on all of the above, our results suggested that the magnolol suppresses the production of pro-inflammatory cytokine by decreasing the expression of TLR4 and inhibiting the activation of NF-κB and MAPKs in LPS-stimulated MMECs.
In conclusion, in vivo, magnolol could alleviate the inflammation reaction from mastitis caused by LPS. In vitro, magnolol suppressed the expression of TLR4 upregulated by LPS and reduced the production of pro-inflammatory mediators regulated by the NF-κB and MAPK in LPS-stimulated MMECs. These findings suggested that magnolol may be a useful agent for preventing and treating LPS-induced mastitis.
REFERENCES
Watts, J.L. 1988. Etiological agents of bovine mastitis. Veterinary Microbiology 16: 41–66.
Burvenich, C., V. Van Merris, J. Mehrzad, A. Diez-Fraile, and L. Duchateau. 2003. Severity of E. coli mastitis is mainly determined by cow factors. Veterinary Research 34: 521–564.
Vangroenweghe, F., P. Rainard, M. Paape, L. Duchateau, and C. Burvenich. 2004. Increase of Escherichia coli inoculum doses induces faster innate immune response in primiparous cows. Journal of Dairy Science 87: 4132–4144.
Li, Y., G.V. Limmon, F. Imani, and C. Teng. 2009. Induction of lactoferrin gene expression by innate immune stimuli in mouse mammary epithelial HC-11 cells. Biochimie 91: 58–67.
Strandberg, Y., C. Gray, T. Vuocolo, L. Donaldson, M. Broadway, and R. Tellam. 2005. Lipopolysaccharide and lipoteichoic acid induce different innate immune responses in bovine mammary epithelial cells. Cytokine 31: 72–86.
Reuven, E.M., A. Fink, and Y. Shai. 2014. Regulation of innate immune responses by transmembrane interactions: lessons from the TLR family. Biochimica et Biophysica Acta 1838(6): 1586–1593.
Ariyadi, B., N. Isobe, and Y. Yoshimura. 2014. Toll-like receptor signaling for the induction of mucin expression by lipopolysaccharide in the hen vagina. Poultry Science 93: 673–679.
Kyriakis, J.M., and J. Avruch. 2001. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiological Reviews 81: 807–869.
Lee, J.C., S. Kassis, S. Kumar, A. Badger, and J.L. Adams. 1999. p38 mitogen-activated protein kinase inhibitors-mechanisms and therapeutic potentials. Pharmacology and Therapeutics 82: 389–397.
Riollet, C., Rainard, P., Poutrel B. 2002 Cells and cytokines in inflammatory secretions of bovine mammary gland. In Biology of the Mammary Gland, 247-258. Springer.
Watanabe, K., H. Watanabe, Y. Goto, M. Yamaguchi, N. Yamamoto, and K. Hagino. 1983. Pharmacological properties of magnolol and honokiol extracted from Magnolia officinalis: central depressant effects. Planta Medica 49: 103–108.
Blakey, D.H., J.M. Bayley, and K.C. Huang. 1993. Suitability of human chromosome-specific DNA libraries for mutagenicity studies in Macaca fascicularis. Mutagenesis 8: 189–192.
Son, H.J., H.J. Lee, H.S. Yun-Choi, and J.H. Ryu. 2000. Inhibitors of nitric oxide synthesis and TNF-alpha expression from Magnolia obovata in activated macrophages. Planta Medica 66: 469–471.
Park, J., J. Lee, E. Jung, Y. Park, K. Kim, B. Park, K. Jung, E. Park, J. Kim, and D. Park. 2004. In vitro antibacterial and anti-inflammatory effects of honokiol and magnolol against Propionibacterium sp. European Journal of Pharmacology 496: 189–195.
Fu, Y., B. Liu, N. Zhang, Z. Liu, D. Liang, F. Li, Y. Cao, X. Feng, X. Zhang, and Z. Yang. 2013. Magnolol inhibits lipopolysaccharide-induced inflammatory response by interfering with TLR4 mediated NF-kappaB and MAPKs signaling pathways. Journal of Ethnopharmacology 145: 193–199.
Li, D., Y. Fu, W. Zhang, G. Su, B. Liu, M. Guo, F. Li, D. Liang, Z. Liu, X. Zhang, et al. 2013. Salidroside attenuates inflammatory responses by suppressing nuclear factor-kappaB and mitogen activated protein kinases activation in lipopolysaccharide-induced mastitis in mice. Inflammation Research 62: 9–15.
Smalley, M.J. 2010. Isolation, culture and analysis of mouse mammary epithelial cells. Methods in Molecular Biology 633: 139–170.
Li, D., N. Zhang, Y. Cao, W. Zhang, G. Su, Y. Sun, Z. Liu, F. Li, D. Liang, B. Liu, et al. 2013. Emodin ameliorates lipopolysaccharide-induced mastitis in mice by inhibiting activation of NF-κB and MAPKs signal pathways. European Journal of Pharmacology 705: 79–85.
Li, Q., and I.M. Verma. 2002. NF-kappaB regulation in the immune system. Nature Reviews Immunology 2: 725–734.
Jung, W.K., D.Y. Lee, C. Park, Y.H. Choi, I. Choi, S.G. Park, S.K. Seo, S.W. Lee, S.S. Yea, S.C. Ahn, et al. 2010. Cilostazol is anti-inflammatory in BV2 microglial cells by inactivating nuclear factor-kappaB and inhibiting mitogen-activated protein kinases. British Journal of Pharmacology 159: 1274–1285.
Zhao, X., and P. Lacasse. 2008. Mammary tissue damage during bovine mastitis: causes and control. Journal of Animal Science 86: 57–65.
Viguier, C., S. Arora, N. Gilmartin, K. Welbeck, and R. O’Kennedy. 2009. Mastitis detection: current trends and future perspectives. Trends in Biotechnology 27: 486–493.
Babra, C., J.G. Tiwari, G. Pier, T.H. Thein, R. Sunagar, S. Sundareshan, S. Isloor, N.R. Hegde, S. de Wet, and M. Deighton. 2013. The persistence of biofilm-associated antibiotic resistance of Staphylococcus aureus isolated from clinical bovine mastitis cases in Australia. Folia Microbiologica 58: 469–474.
Senegas, A., O. Villard, A. Neuville, L. Marcellin, A.W. Pfaff, T. Steinmetz, M. Mousli, J.P. Klein, and E. Candolfi. 2009. Toxoplasma gondii-induced foetal resorption in mice involves interferon-gamma-induced apoptosis and spiral artery dilation at the maternofoetal interface. International Journal for Parasitology 39: 481–487.
Takahashi, K., H. Harada, S.W. Schaffer, and J. Azuma. 1992. Effect of taurine on intracellular calcium dynamics of cultured myocardial cells during the calcium paradox. Advances in Experimental Medicine and Biology 315: 153–161.
Li, F., D. Liang, Z. Yang, T. Wang, W. Wang, X. Song, M. Guo, E. Zhou, D. Li, and Y. Cao. 2013. Astragalin suppresses inflammatory responses via down-regulation of NF-κB signaling pathway in lipopolysaccharide-induced mastitis in a murine model. International Immunopharmacology 17: 478–482.
Song, X., Zhang, W., Wang, T., Jiang, H., Zhang, Z., Fu, Y., Yang, Z., Cao, Y., Zhang, N. 2014. Geniposide plays an anti-inflammatory role via regulating TLR4 and downstream signaling pathways in lipopolysaccharide-induced mastitis in mice. Inflammation 1-11.
Fried, L.E., and J.L. Arbiser. 2009. Honokiol, a multifunctional antiangiogenic and antitumor agent. Antioxidants and Redox Signaling 11: 1139–1148.
Zheng, J., A.D. Watson, and D.E. Kerr. 2006. Genome-wide expression analysis of lipopolysaccharide-induced mastitis in a mouse model. Infection and Immunity 74: 1907–1915.
Krawisz, J., P. Sharon, and W. Stenson. 1984. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Gastroenterology 87: 1344–1350.
Higashimoto, T., A. Panopoulos, C.L. Hsieh, and E. Zandi. 2006. TNFalpha induces chromosomal abnormalities independent of ROS through IKK, JNK, p38 and caspase pathways. Cytokine 34: 39–50.
Yoon, W.J., J.Y. Moon, J.Y. Kang, G.O. Kim, N.H. Lee, and C.G. Hyun. 2010. Neolitsea sericea essential oil attenuates LPS-induced inflammation in RAW 264.7 macrophages by suppressing NF-kappaB and MAPK activation. Natural Product Communications 5: 1311–1316.
Ho, A.W., C.K. Wong, and C.W. Lam. 2008. Tumor necrosis factor-alpha up-regulates the expression of CCL2 and adhesion molecules of human proximal tubular epithelial cells through MAPK signaling pathways. Immunobiology 213: 533–544.
Shalaby, M.R., B.B. Aggarwal, E. Rinderknecht, L.P. Svedersky, B.S. Finkle, and M.A. Palladino Jr. 1985. Activation of human polymorphonuclear neutrophil functions by interferon-gamma and tumor necrosis factors. Journal of Immunology 135: 2069–2073.
Oh, Y.C., W.K. Cho, Y.H. Jeong, G.Y. Im, A. Kim, Y.H. Hwang, T. Kim, K.H. Song, and J.Y. Ma. 2012. A novel herbal medicine KIOM-MA exerts an anti-inflammatory effect in LPS-stimulated RAW 264.7 macrophage cells. Evidence-Based Complementary and Alternative Medicine 2012: 462383.
Hayden, M.S., and S. Ghosh. 2012. NF-kappaB, the first quarter-century: remarkable progress and outstanding questions. Genes and Development 26: 203–234.
Vallabhapurapu, S., and M. Karin. 2009. Regulation and function of NF-kappaB transcription factors in the immune system. Annual Review of Immunology 27: 693–733.
Liang, C.J., C.W. Lee, H.C. Sung, Y.H. Chen, Y.C. Chiang, H.Y. Hsu, Y.C. Tseng, C.Y. Li, S.H. Wang, and Y.L. Chen. 2014. Ganoderma lucidum polysaccharides reduce lipopolysaccharide-induced interleukin-1 beta expression in cultured smooth muscle cells and in thoracic aortas in mice. Evidence-based Complementary and Alternative Medicine 2014: 305149.
Remppis, A., F. Bea, H.J. Greten, A. Buttler, H. Wang, Q. Zhou, M.R. Preusch, R. Enk, R. Ehehalt, H. Katus, and E. Blessing. 2010. Rhizoma Coptidis inhibits LPS-induced MCP-1/CCL2 production in murine macrophages via an AP-1 and NFkappaB-dependent pathway. Mediators of Inflammation 2010: 194896.
Kaminska, B. 2005. MAPK signalling pathways as molecular targets for anti-inflammatory therapy-from molecular mechanisms to therapeutic benefits. Biochimica et Biophysica Acta 1754: 253–262.
Medzhitov, R., and J.C. Kagan. 2006. Phosphoinositide-mediated adaptor recruitment controls toll-like receptor signaling. Cell 125: 943–955.
ACKNOWLEDGMENTS
This work was supported by a grant from the National Natural Science Foundation of China (Nos. 31272622, 31201925), the Research Fund for the Doctoral Program of Higher Education of China (Nos. 20110061130010, 20120061120098), and Jilin Province Science Foundation for Youths (No. 20130522087JH).
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors’ Contributions
Naisheng Zhang and Zhengtao Yang conceived and designed the paper. Wei Wang, Xiaojing Song, and Tiancheng Wang executed the experiment and analyzed the samples. Dejie Liang and Yongguo Cao analyzed the data. All authors interpreted the data, critically revised the manuscript for important intellectual contents, and approved the final version.
Rights and permissions
About this article
Cite this article
Wei, W., Dejie, L., Xiaojing, S. et al. Magnolol Inhibits the Inflammatory Response in Mouse Mammary Epithelial Cells and a Mouse Mastitis Model. Inflammation 38, 16–26 (2015). https://doi.org/10.1007/s10753-014-0003-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-014-0003-2