Abstract
Acute respiratory distress syndrome (ARDS) is accompanied by severe lung inflammation induced by various diseases. Despite the severity of symptoms, therapeutic strategies for this pathologic condition are still poorly developed. Interferon (IFN)-α is well known as an antiviral cytokine and low-dose IFN-α has been reported to show antiinflammatory effects. Therefore, we investigated how this cytokine affected ARDS in a mouse model. C57BL/6 mice received sequential intratracheal administration of α-galactosylceramide (α-GalCer) and lipopolysaccharide (LPS), which resulted in the development of fulminant ARDS. These mice were then treated intranasally with IFN-α and their survival, lung weight, pathological findings, and cytokine production were evaluated. Administration of low-dose IFN-α prolonged survival of fulminant ARDS mice, but higher doses of IFN-α did not. Histological analysis showed that low-dose IFN-α treatment improved findings of diffuse alveolar damage in fulminant ARDS mice, which was associated with reduction in the wet/dry (W/D) lung weight ratio. Furthermore, IFN-γ production in the lungs was significantly reduced in IFN-α-treated mice, compared with control mice, but tumor necrosis factor (TNF)-α production was almost equivalent for both groups. Low-dose IFN-α shows antiinflammatory and therapeutic effects in a mouse model of fulminant ARDS, and reduced production of IFN-γ in the lung may be involved in the beneficial effect of this treatment.
Similar content being viewed by others
INTRODUCTION
Acute respiratory distress syndrome (ARDS) is characterized as a diffuse lung injury with severe hypoxemia and a high rate of fatality even now, roughly 25–30 %, which develops under various pathogenic conditions [1]. Lung injury is triggered by inhalation of airborne causative agents, designated as direct lung injury, and develops in the context of systemic disorders such as sepsis, designated as indirect lung injury [2]. Direct lung injury has been reported to occur during infection with severe acute respiratory syndrome (SARS) virus [3] or H5N1, a highly pathogenic avian influenza virus [4, 5]. The serum levels of interferon (IFN)-γ, tumor necrosis factor (TNF)-α, and IL-6 were elevated in the cases of fatal human H5N1 influenza virus infection [6], and several cytokines, including TNF-α, IL-1β, IL-6, IL-8, and IL-10 showed strikingly increased concentrations in the bronchoalveolar lavage (BAL) fluids of these patients [7–9].
In animal models of direct lung injury induced by intratracheal administration of lipopolysaccharide (LPS), acute and robust influx of inflammatory cells into the lungs is observed but these inflammatory changes are completely resolved within 48 h, without demonstration of either alveolar epithelial injury or vascular leakage, typical histopathological features of ARDS [10, 11]. Recently, we reported an animal model of fulminant ARDS established by sensitizing mice with α-galactosylceramide (α-GalCer), a potent activator of natural killer T (NKT) cells, followed by a challenge with LPS [12]. In this model, all mice rapidly died with diffuse alveolar damage in the lungs, which was accompanied by a striking increase of IFN-γ and TNF-α concentrations in BAL fluids [12].
A variety of proinflammatory cytokines and chemokines, such as TNF-α, IL-1β, IL-6, and IL-8, are reported to play critical roles in the pathogenic mechanism of ARDS [7–9], whereas lower production of antiinflammatory mediators such as IL-10 and IL-1 receptor antagonist is associated with the generally poor prognosis [13]. Based on an understanding of the involvement of these cytokines, various antiinflammatory agents, including corticosteroids [14, 15], statins [16], prostaglandin E1 [17], neutrophil elastase inhibitors [18], and inhibitors of arachidonic acid metabolism [19, 20], have been tested for their clinical efficacy in ARDS therapy. However, a truly efficacious agent has not yet been established.
Type I IFN, discovered as an endogenously synthesized antiviral protein [21], is deeply involved in acute and chronic inflammatory responses, including delayed-type hypersensitivity [22], experimental autoimmune encephalomyelitis [23], and collagen-induced arthritis [24]. In addition to these nonantiviral actions, this cytokine inhibits division of certain tumor cell lines [25], promotes cytolytic activity of NK cells and T cells [26], and enhances expression of MHC molecules [27]. Thus, type I IFN has been gradually recognized as an important player in the cytokine network that leads to regulation of innate and acquired immune responses [21]. In clinical settings, type I IFN is used for the treatment of viral hepatitis and multiple sclerosis [21]. Recently, in animal experiments, antiinflammatory effects as a result of type I IFN administration have been reported in experimental autoimmune encephalomyelitis [28], rheumatoid arthritis [29], bacterial peritonitis [30], and lung inflammation [31].
With this background in mind, the present study addressed how type I IFNs affect the clinical course and inflammatory responses in our mouse model of fulminant ARDS sensitized with α-GalCer and challenged with LPS. We found that low-dose administration of IFN-α improved survival and attenuated inflammatory responses in fulminant ARDS mice and that these effects were associated with suppression of IFN-γ synthesis in the lung.
MATERIALS AND METHODS
Animals
C57BL/6 mice were bred in a pathogen-free environment at the Institute for Animal Experimentation, Tohoku University Graduate School of Medicine. All mice were used for experiments at 7–8 weeks of age. All experimental protocols described in the present study were approved by the Ethics Review Committee for Animal Experimentation of Tohoku University.
Reagents
α-GalCer, purchased from Funakoshi (Tokyo, Japan), was dissolved in dimethyl sulfoxide (DMSO) (Sigma-Aldrich, St. Louis, MO, USA) at 5 mg/ml and then diluted with phosphate-buffered saline (PBS) to a final dose of 0.4 % DMSO for in vivo use. LPS from Escherichia coli (O111: B4) was purchased from Sigma-Aldrich.
Fulminant ARDS Model
To induce lung injury, mice were anesthetized by intraperitoneal injection of 70 mg/kg of pentobarbital (Abbott Laboratories, North Chicago, IL, USA) and then restrained on a small board and 50 μl of α-GalCer (1 μg) was injected into each mouse by inserting a 24-gauge intravenous catheter (Terumo, Tokyo, Japan) into the trachea. Twenty-four hours later, 50 μl of LPS (50 μg) was administered via the same route. Sham-operated mice were injected with 0.4 % DMSO-containing PBS (dPBS) into the trachea and 24 h later, 50 μl of PBS was administered via the same route.
Treatment with IFN-α
Recombinant human IFN-αA/D was provided by the Nippon Roche Research Center (Kamakura, Japan). Mice were administered various amounts of IFN-α intranasally at various time intervals after LPS injection. IFN-α was administrated intratracheally with LPS at the same time only at 0 h.
Wet/Dry Lung Weight Ratio
The lungs of mice treated with IFN-α or PBS were weighed 48 h after LPS challenge to determine the final wet lung weight. They were then dried in an oven at 60 °C for 48 h and weighed again to determine the dry weight. The wet/dry (W/D) weight ratio was then calculated.
Histological Examination
The lung specimens obtained from mice were fixed in 10 % buffered formalin, dehydrated, and embedded in paraffin. Sections were cut and stained with hematoxylin–eosin (HE) stains using standard staining procedures at the Biomedical Research Core, the Animal Pathology Platform of Tohoku University Graduate School of Medicine. We measured histological evidence of tissue injury using the Lung Injury Scoring System recommended by the American Thoracic Society (ATS) [32]. Lung Injury Scoring System parameters include neutrophils in the alveolar space, neutrophils in the interstitial space, hyaline membranes, proteinaceous debris filling the airspaces, and alveolar septal thickening. At least 20 random high-power fields (400× total magnification) were independently scored in a blinded fashion. Each of five histological findings was graded using a three-tiered scheme that is summarized in Table 1. The sum of each of the five independent variables shown in Table 1 was weighted according to the relevance ascribed to each feature by the ATS Committee and then was normalized to the number of fields evaluated.
Preparation of BAL Fluids and Lung Homogenates
Mice were sacrificed at 6 h after LPS exposure. Their chests were opened, their tracheae were cannulated (22 G I.V. catheter), and 1 ml of PBS was infused intratracheally and withdrawn. This procedure was performed three times. BAL fluids were stored at −80 °C until cytokines were measured. After collecting BAL fluids, pulmonary circulation was rinsed by injection of 3 ml PBS into the right ventricle. Lungs were then harvested and stored in 1.5 ml of PBS. The lungs in PBS were later homogenized and centrifuged at 1,600 rpm for 10 min at 4 °C, and the supernatants were stored at −80 °C until cytokines were measured.
Measurement of Cytokine Concentrations
The concentrations of IFN-γ and TNF-α in the supernatants of lung homogenates and BAL fluids were measured by ELISA using capture and biotinylated developing antibodies (BD Biosciences, Franklin Lakes, NJ, USA). The detection limits were 15 and 5 pg/ml, respectively.
Statistical Analysis
Analysis of data was conducted using JMP Pro® 9.0.2 software (SAS Institute Inc., Cary, NC, USA) on a Macintosh computer. Data are expressed as mean ± SD. Statistical analysis between groups was performed using analysis of variance with a post hoc analysis (Fisher’s protected least significant difference test). Survival data were analyzed using the logrank test. A p value <0.05 was considered significant.
RESULTS
Effect of IFN-α on the Survival of Fulminant ARDS Mice
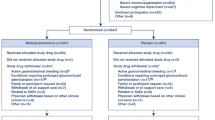
In our earlier studies [12], intratracheal administration of LPS following sensitization with α-GalCer led to the development of fulminant ARDS in mice, which caused fatal outcomes within 72 h after LPS injection. In the current study, we investigated whether IFN-α affected the clinical course of fulminant ARDS mice. For this purpose, mice were treated with various doses of IFN-α (100 IU, 1,000 IU, and 10,000 IU/mouse) or with PBS as a vehicle control 12 h before, simultaneously, and 24 h, 48 h, and 72 h after LPS injection. As shown in Fig. 1, all mice treated with PBS died within 72 h, whereas treatment with low-dose IFN-α, 100 IU/mouse, significantly prolonged the survival duration of fulminant ARDS mice. However, higher doses of IFN-α (1,000 IU and 10,000 IU/mouse) did not prolong survival. These results demonstrated that low-dose, but not high-dose, IFN-α protected mice from death caused by fulminant ARDS.
Effect of IFN-α treatment on the survival of fulminant ARDS mice. Mice received intratracheal instillation of LPS 24 h after administration of α-GalCer via the same route. These mice were treated with various doses of IFN-α or PBS as a control 12 h before (intranasally: i.n.), simultaneously (intratracheally), and 24 h (i.n.), 48 h (i.n.) and 72 h (i.n.) after LPS injection. The number of live mice was counted every 24 h after the LPS challenge. Each group consisted of five mice. Circles IFN-α 100 IU, squares IFN-α 1,000 IU, diamonds IFN-α 10,000 IU, triangles PBS. NS not significant; *P < 0.05 compared with PBS-treated mice.
Effect of Low-dose IFN-α Treatment on Lung Injury in Fulminant ARDS Mice
Next, we addressed the effect of IFN-α administration on lung injuries developed in fulminant ARDS mice by conducting histopathological analyses. Using the results illustrated in Fig. 1 as a basis, α-GalCer-sensitized and LPS-challenged mice were treated with low-dose IFN-α (100 IU/mouse) or PBS, and lung sections stained with HE were analyzed under a microscope 72 h after LPS challenge. As shown in Fig. 2, massive infiltration of neutrophils not only into the intraalveolar septa but also into the alveolar spaces was observed in the α-GalCer-sensitized and LPS-challenged mice that received PBS treatment, whereas these inflammatory responses were strikingly attenuated when mice were treated with low-dose IFN-α. For an objective evaluation of the inflammatory changes, we quantified the histological changes of the tissue injuries using a Lung Injury Scoring System. As shown in Fig. 2b, the lung injury scores were significantly lower in low-dose IFN-α-treated mice than those in control mice. These results indicate that low-dose IFN-α effectively inhibited the development of FARDS caused by α-GalCer sensitization and LPS challenge.
Effect of low-dose IFN-α treatment on histological changes in fulminant ARDS mice. Mice received intratracheal instillation of LPS 24 h after administration of α-GalCer via the same route (α-GalCer/LPS). These mice were treated with IFN-α (100 IU) or PBS 12 h before (intranasally: i.n.), simultaneously (intratracheally), and 24 h (i.n.) and 48 h (i.n.) after LPS injection. Sections of lungs 72 h after LPS challenge were stained with hematoxylin and eosin and observed under a light microscope. Representative pictures of three mice are shown at magnifications of ×40 (left) and ×400 (right).
In addition, to evaluate the degree of lung edema, a characteristic of ARDS, we examined W/D lung weight ratios 48 h after LPS challenge. As Fig. 3 shows, the W/D lung weight ratios were significantly lower in mice treated with IFN-α than in PBS-treated mice, and the levels in the former mice were almost equivalent to those in sham-operated mice. These results clearly demonstrated that low-dose IFN-α treatment mitigated the development of fulminant ARDS by attenuating inflammatory responses in the lung.
Effect of low-dose IFN-α treatment on lung edema in fulminant ARDS mice. Mice received intratracheal instillation of LPS 24 h after administration of α-GalCer via the same route (α-GalCer/LPS). In a sham group, mice received intratracheal instillation of PBS 24 h after administration of PBS via the same route (sham). The wet and dry lung weight ratio was examined 48 h after challenge injection of LPS or PBS. Each column represents the mean ± SD of five mice. NS not significant; *P < 0.05.
Effect of Low-dose IFN-α Treatment on Cytokine Synthesis in the Lungs
To further investigate the mechanism for the beneficial effects of IFN-α on fulminant ARDS, we evaluated the synthesis in the lungs of IFN-γ and TNF-α, both of which were reported as critical cytokines in our mouse model of fulminant ARDS [12]. For this purpose, concentrations of these cytokines in BAL fluids and lung homogenates were measured 6 h after LPS challenge. As shown in Fig. 4a, treatment with low-dose IFN-α significantly reduced the IFN-γ levels in both BAL fluids and lung homogenates in α-GalCer-sensitized and LPS-challenged mice, compared to those in PBS-treated mice, and the IFN-γ levels in the lung homogenates of IFN-α-treated mice were almost as low as those in sham-operated mice. TNF-α synthesis in the lung, as determined by assay of BAL fluids and lung homogenates, was also augmented in mice sensitized with α-GalCer and challenged with LPS. In striking contrast to the observed impact upon IFN-γ levels, low-dose IFN-α treatment did not reduce the synthesis of TNF-α in the lung, measured by assaying the two types of lung specimens (Fig. 4b).
Effect of low-dose IFN-α treatment on cytokine synthesis in fulminant ARDS mice. Mice received intratracheal instillation of LPS 24 h after administration of α-GalCer via the same route (α-GalCer/LPS). In a sham group, mice received intratracheal instillation of PBS 24 h after administration of PBS via the same route (sham). These mice were treated with IFN-α (100 IU) or PBS 12 h before (intranasally: i.n.) and simultaneously (intratracheally) after LPS injection. The concentrations of IFN-γ and TNF-α in lung homogenates and BAL fluids were measured 6 h after challenge injection of LPS or PBS. Each column represents the mean ± SD of four or five mice. NS not significant; *P < 0.05.
DISCUSSION
In the present study, we demonstrated that (1) administration of low-dose IFN-α prolonged the survival of fulminant ARDS mice sensitized with α-GalCer and challenged with LPS, but high dose IFN-α did not provide this benefit; (2) low-dose IFN-α treatment attenuated the diffuse alveolar damage that occurs as a consequence of massive infiltration of neutrophils, a typical histological feature of ARDS, and it reduced the W/D lung weight ratio, an indicator of lung edema, compared to that in the PBS-treated group; and (3) low-dose IFN-α treatment led to decreased production of IFN-γ, but not of TNF-α, according to assays of BAL fluids and lung homogenates in fulminant ARDS mice. These results indicate that low-dose IFN-α has an antiinflammatory and therapeutic effect in a mouse model of fulminant ARDS and suggest that reduced production of IFN-γ in the lungs may be involved in the beneficial effects of this treatment.
Infection with H5N1, a highly pathogenic avian influenza virus, is reported to cause fulminant ARDS with histopathologically defined diffuse alveolar damage in the lung, which is often refractory even to advanced medical therapy [4, 5]. This pathogenic condition is associated not only with viral replication in bronchial epithelial cells but also with uncontrolled production of inflammatory cytokines, the so-called “cytokine storm” in the lungs that is associated with a fatal outcome in many cases [4, 32]. Thus, control of excessive inflammatory responses may provide an effective therapeutic target against fulminant ARDS caused by the H5N1 influenza virus. Type I IFNs are synthesized and secreted by virus-infected cells, which upregulate the expression of antiviral genes and render the host resistant to this infection [21]. Recently, Haasbach et al. demonstrated that low-dose type I IFN treatment was effective in protecting mice from infection with H5N1 influenza virus [33]. Though this effect is thought to be due to the antiviral activity of type I IFN, it remains unanswered whether this treatment leads to suppression of the inflammatory response at the infected sites. In the present study, on the other hand, we examined the effect of type I IFN treatment on the fulminant ARDS developed by a mechanism unrelated to viral infection, which may aid in an understanding of its therapeutic potential via an antiinflammatory effect separate from antiviral activity, although it remains unclear if our model is valid for analyzing the pathogenic mechanism of fulminant ARDS caused by influenza virus infection and other clinically important conditions.
In animal models of bacterial peritonitis [30] and acute lung injury associated with subarachnoid hemorrhage [31], high-dose IFN-β was used to demonstrate antiinflammatory effects. However, the present study showed that low-dose IFN-α was effective in extending the survival time of fulminant ARDS mice. The antiinflammatory effects of lower doses of IFN-α, as recognized in our current study, have been reported in previous investigations in various animal models of inflammatory diseases [33–37]. In in vitro experiments by Amadori et al. [38], IFN-α was shown to suppress the expression of a TNF-α gene by swine alveolar macrophages at dosages as low as 0.5 IU/ml. The same investigators also reported that orally administered IFN-α suppressed the expression of inflammatory cytokines such as IFN-γ, TNF-α, and IL-6 after weaning in piglets [39]. In contrast, in cattle, parenteral administration of high-dose, but not low-dose IFN-α, actually promoted inflammatory responses [40]. Taken together with these previous studies, our present findings suggest that low-dose administration of IFN-α may exert antiinflammatory effects by inhibiting the production of proinflammatory cytokines, although the precise mechanism remains to be elucidated.
Several mechanisms have been proposed to explain the antiinflammatory effects of type I IFN. In previous studies by Quin et al., interaction of IFN-β with its receptor was shown to trigger the induction of suppressor of cytokine signaling 1 (SOCS1), which then regulated IFN-γ synthesis by inhibiting the signal transducer and activator of transcription (STAT1α) [41]. Other investigators have also reported that the antiinflammatory effects of type I IFNs are mediated by the production of IL-10 [42] and by suppressing TNF-α synthesis through the generation of tristetraprolin (TTP), an antiinflammatory protein [43]. In our study, the antiinflammatory effects of IFN-α were not associated with alteration of TNF-α synthesis, unlike the remarkable reduction of IFN-γ synthesis, and IL-10 was not detected in the lungs of mice in any of the groups (data not shown). In agreement with these results, we previously reported on the critical role of IFN-γ, rather than TNF-α, which role was limited, in the pathogenesis of fulminant ARDS developed in α-GalCer-sensitized and LPS-challenged mice. In this model, NKT cells and Gr-1+ monocytes were involved in the synthesis of IFN-γ [12]. These findings raise the possibility that IFN-α may ameliorate the effects of fulminant ARDS by accelerating SOCS1 activation, which leads to the suppression of IFN-γ synthesis by NKT cells and Gr-1+ monocytes. However, in the present study, attempts to address the precise mechanism in the beneficial effect of IFN-α remain to be made, and further investigation is needed to clarify this possibility.
In conclusion, we demonstrated that low-dose IFN-α improved the survival of fulminant ARDS mice that were sensitized with α-GalCer and challenged with LPS by suppressing the production of IFN-γ and subsequent inflammatory responses. These results suggest that this cytokine could be a possible therapeutic option for ARDS, which is refractory even to advanced medical therapies currently available in clinical settings. In general, higher doses of type I IFNs are administered to patients with hepatitis virus infection and multiple sclerosis [44–46]. However, higher dose treatments are known to be associated with various adverse effects such as chills, fever, muscle aches, headaches, and depression. In this respect, less frequent adverse effects might be expected as an additional benefit of lower dose IFN-α treatment. Thus, the present study may provide a significant impetus for further development of promising ARDS treatments.
References
Wheeler, A.P., G.R. Bernard, B.T. Thompson, D. Schoenfeld, H.P. Wiedemann, B. de Boisblanc, A.F. Connors Jr., R.D. Hite, and A.L. Harabin. 2006. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. The New England Journal of Medicine 354: 2213–2224.
Ware, L.B., and M.A. Matthay. 2000. The acute respiratory distress syndrome. The New England Journal of Medicine 342: 1334–1349.
Lee, N., D. Hui, A. Wu, P. Chan, P. Cameron, G.M. Joynt, A. Ahuja, M.Y. Yung, C.B. Leung, K.F. To, S.F. Lui, C.C. Szeto, S. Chung, and J.J. Sung. 2003. A major outbreak of severe acute respiratory syndrome in Hong Kong. The New England Journal of Medicine 348: 1986–1994.
Beigel, J.H., J. Farrar, A.M. Han, F.G. Hayden, R. Hyer, M.D. de Jong, S. Lochindarat, T.K. Nguyen, T.H. Nguyen, T.H. Tran, A. Nicoll, S. Touch, and K.Y. Yuen. 2005. Avian influenza A (H5N1) infection in humans. The New England Journal of Medicine 353: 1374–1385.
Kawachi, S., S.T. Luong, M. Shigematsu, H. Furuya, T.T. Phung, P.H. Phan, H. Nunoi, L.T. Nguyen, and K. Suzuki. 2009. Risk parameters of fulminant acute respiratory distress syndrome and avian influenza (H5N1) infection in Vietnamese children. Journal of Infectious Diseases 200: 510–515.
To, K.F., P.K. Chan, K.F. Chan, W.K. Lee, W.Y. Lam, K.F. Wong, N.L. Tang, D.N. Tsang, R.Y. Sung, T.A. Buckley, J.S. Tam, and A.F. Cheng. 2001. Pathology of fatal human infection associated with avian influenza A H5N1 virus. Journal of Medical Virology 63: 242–246.
Bhatia, M., and S. Moochhala. 2004. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. The Journal of Pathology 202: 145–156.
Park, W.Y., R.B. Goodman, K.P. Steinberg, J.T. Ruzinski, F. Radella 2nd, D.R. Park, J. Pugin, S.J. Skerrett, L.D. Hudson, and T.R. Martin. 2001. Cytokine balance in the lungs of patients with acute respiratory distress syndrome. American Journal of Respiratory and Critical Care Medicine 164: 1896–1903.
Shimabukuro, D.W., T. Sawa, and M.A. Gropper. 2003. Injury and repair in lung and airways. Critical Care Medicine 31: S524–S531.
Bastarache, J.A., and T.S. Blackwell. 2009. Development of animal models for the acute respiratory distress syndrome. Disease Models & Mechanisms 2: 218–223.
Matute-Bello, G., C.W. Frevert, and T.R. Martin. 2008. Animal models of acute lung injury. American Journal of Physiology. Lung Cellular and Molecular Physiology 295: L379–L399.
Aoyagi, T., N. Yamamoto, M. Hatta, D. Tanno, A. Miyazato, K. Ishii, K. Suzuki, T. Nakayama, M. Taniguchi, H. Kunishima, Y. Hirakata, M. Kaku, and K. Kawakami. 2011. Activation of pulmonary invariant NKT cells leads to exacerbation of acute lung injury caused by LPS through local production of IFN-γ and TNF-α by Gr-1+ monocytes. International Immunology 23: 97–108.
Donnelly, S.C., R.M. Strieter, P.T. Reid, S.L. Kunkel, M.D. Burdick, I. Armstrong, A. Mackenzie, and C. Haslett. 1996. The association between mortality rates and decreased concentrations of interleukin-10 and interleukin-1 receptor antagonist in the lung fluids of patients with the adult respiratory distress syndrome. Annals of Internal Medicine 125: 191–196.
Peter, J.V., P. John, P.L. Graham, J.L. Moran, I.A. George, and A. Bersten. 2008. Corticosteroids in the prevention and treatment of acute respiratory distress syndrome (ARDS) in adults: meta-analysis. BMJ 336: 1006–1009.
Tang, B.M., J.C. Craig, G.D. Eslick, I. Seppelt, and A.S. McLean. 2009. Use of corticosteroids in acute lung injury and acute respiratory distress syndrome: a systematic review and meta-analysis. Critical Care Medicine 37: 1594–1603.
Craig, T.R., M.J. Duffy, M. Shyamsundar, C. McDowell, C.M. O’Kane, J.S. Elborn, and D.F. McAuley. 2011. A randomized clinical trial of hydroxymethylglutaryl-coenzyme a reductase inhibition for acute lung injury (The HARP Study). American Journal of Respiratory and Critical Care Medicine 183: 620–626.
Bone, R.C., G. Slotman, R. Maunder, H. Silverman, T.M. Hyers, M.D. Kerstein, and J.J. Ursprung. 1989. Randomized double-blind, multicenter study of prostaglandin E1 in patients with the adult respiratory distress syndrome. Prostaglandin E1 Study Group. Chest 96: 114–119.
Zeiher, B.G., A. Artigas, J.L. Vincent, A. Dmitrienko, K. Jackson, B.T. Thompson, and G. Bernard. 2004. Neutrophil elastase inhibition in acute lung injury: results of the STRIVE study. Critical Care Medicine 32: 1695–1702.
2000. Ketoconazole for early treatment of acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. The ARDS Network. Journal of the American Medical Association 283:1995–2002.
Bernard, G.R., A.P. Wheeler, J.A. Russell, R. Schein, W.R. Summer, K.P. Steinberg, W.J. Fulkerson, P.E. Wright, B.W. Christman, W.D. Dupont, S.B. Higgins, and B.B. Swindell. 1997. The effects of ibuprofen on the physiology and survival of patients with sepsis. The Ibuprofen in Sepsis Study Group. The New England Journal of Medicine 336: 912–918.
Billiau, A. 2006. Anti-inflammatory properties of type I interferons. Antiviral Research 71: 108–116.
De Maeyer, E., J. De Maeyer-Guignard, and M. Vandeputte. 1975. Inhibition by interferon of delayed-type hypersensitivity in the mouse. Proceedings of the National Academy of Sciences of the United States of America 72: 1753–1757.
Abreu, S.L. 1982. Suppression of experimental allergic encephalomyelitis by interferon. Immunological Communications 11: 1–7.
Triantaphyllopoulos, K.A., R.O. Williams, H. Tailor, and Y. Chernajovsky. 1999. Amelioration of collagen-induced arthritis and suppression of interferon-gamma, interleukin-12, and tumor necrosis factor alpha production by interferon-beta gene therapy. Arthritis and Rheumatism 42: 90–99.
Uno, K., S. Shimizu, K. Inaba, M. Kitaura, K. Nakahira, T. Kato, Y. Yamaguchi, and S. Muramatsu. 1988. Effect of recombinant human interferon-alpha A/D on in vivo murine tumor cell growth. Cancer Research 48: 2366–2371.
Moore, M., W.J. White, and M.R. Potter. 1980. Modulation of target cell susceptibility to human natural killer cells by interferon. International Journal of Cancer 25: 565–572.
Ransohoff, R.M., C. Devajyothi, M.L. Estes, G. Babcock, R.A. Rudick, E.M. Frohman, and B.P. Barna. 1991. Interferon-beta specifically inhibits interferon-gamma-induced class II major histocompatibility complex gene transcription in a human astrocytoma cell line. Journal of Neuroimmunology 33: 103–112.
Billiau, A., H. Heremans, F. Vandekerckhove, R. Dijkmans, H. Sobis, E. Meulepas, and H. Carton. 1988. Enhancement of experimental allergic encephalomyelitis in mice by antibodies against IFN-gamma. Journal of Immunology 140: 1506–1510.
van Holten, J., K. Reedquist, P. Sattonet-Roche, T.J. Smeets, C. Plater-Zyberk, M.J. Vervoordeldonk, and P.P. Tak. 2004. Treatment with recombinant interferon-beta reduces inflammation and slows cartilage destruction in the collagen-induced arthritis model of rheumatoid arthritis. Arthritis Research & Therapy 6: R239–R249.
Weighardt, H., S. Kaiser-Moore, S. Schlautkotter, T. Rossmann-Bloeck, U. Schleicher, C. Bogdan, and B. Holzmann. 2006. Type I IFN modulates host defense and late hyperinflammation in septic peritonitis. Journal of Immunology 177: 5623–5630.
Cobelens, P.M., I.A. Tiebosch, R.M. Dijkhuizen, P.H. van der Meide, R. Zwartbol, C.J. Heijnen, J. Kesecioglu, and W.M. van den Bergh. 2010. Interferon-β attenuates lung inflammation following experimental subarachnoid hemorrhage. Critical Care 14: R157.
Matute-Bello, G., G. Downey, B.B. Moore, et al. 2011. An official American Thoracic Society workshop report: Features and measurements of experimental acute lung injury in animals. American Journal of Respiratory Cell and Molecular Biology 44: 725–738.
Liem, N.T., N. Nakajima, P. Phat le, Y. Sato, H.N. Thach, P.V. Hung, L.T. San, H. Katano, T. Kumasaka, T. Oka, S. Kawachi, T. Matsushita, T. Sata, K. Kudo, and K. Suzuki. 2008. H5N1-infected cells in lung with diffuse alveolar damage in exudative phase from a fatal case in Vietnam. Japanese Journal of Infectious Diseases 61: 157–160.
Haasbach, E., K. Droebner, A.B. Vogel, and O. Planz. 2011. Low-dose interferon type I treatment is effective against H5N1 and swine-origin H1N1 influenza A viruses in vitro and in vivo. Journal of Interferon and Cytokine Research 31: 515–525.
Beilharz, M.W., J.M. Cummins, and A.L. Bennett. 2007. Protection from lethal influenza virus challenge by oral type 1 interferon. Biochemical and Biophysical Research Communications 355: 740–744.
Cummins, M.J., A. Papas, G.M. Kammer, and P.C. Fox. 2003. Treatment of primary Sjogren’s syndrome with low-dose human interferon alfa administered by the oromucosal route: combined phase III results. Arthritis and Rheumatism 49: 585–593.
Ito, A., E. Isogai, K. Yoshioka, K. Sato, N. Himeno, and T. Gotanda. 2010. Ability of orally administered IFN-α4 to inhibit naturally occurring gingival inflammation in dogs. Journal of Veterinary Medical Science 72: 1145–1151.
Ohya, K., T. Matsumura, N. Itchoda, K. Ohashi, M. Onuma, and C. Sugimoto. 2005. Ability of orally administered IFN-alpha-containing transgenic potato extracts to inhibit Listeria monocytogenes infection. Journal of Interferon and Cytokine Research 25: 459–466.
Begni, B., M. Amadori, M. Ritelli, and D. Podavini. 2005. Effects of IFN-alpha on the inflammatory response of swine leukocytes to bacterial endotoxin. Journal of Interferon and Cytokine Research 25: 202–208.
Amadori, M., M. Farinacci, B. Begni, R. Faita, D. Podavini, and M. Colitti. 2009. Effects of interferon-α on the inflammatory response of swine peripheral blood mononuclear cells. Journal of Interferon and Cytokine Research 29: 241–247.
Straub, O.C. 1995. Studies on the suitability of alpha-hybrid interferon application in cattle. Comparative Immunology, Microbiology and Infectious Diseases 18: 239–243.
Qin, H., C.A. Wilson, S.J. Lee, and E.N. Benveniste. 2006. IFN-beta-induced SOCS-1 negatively regulates CD40 gene expression in macrophages and microglia. The FASEB Journal 20: 985–987.
Chang, E.Y., B. Guo, S.E. Doyle, and G. Cheng. 2007. Cutting edge: Involvement of the type I IFN production and signaling pathway in lipopolysaccharide-induced IL-10 production. Journal of Immunology 178: 6705–6709.
Sauer, I., B. Schaljo, C. Vogl, I. Gattermeier, T. Kolbe, M. Muller, P.J. Blackshear, and P. Kovarik. 2006. Interferons limit inflammatory responses by induction of tristetraprolin. Blood 107: 4790–4797.
Cooksley, W.G. 2004. The role of interferon therapy in hepatitis B. MedGenMed 6: 16.
Pereira, A.A., and I.M. Jacobson. 2009. New and experimental therapies for HCV. Nature Reviews. Gastroenterology & Hepatology 6: 403–411.
Acknowledgments
This study was supported by a grant from the Ministry of Education, Culture, Sports, Science, and Technology (Grant-in-Aid for Challenging Exploratory Research (23659841)) and a grant from the Ministry of Health, Labor, and Welfare of Japan (Research on Emerging and Re-emerging Infectious Diseases; 22-SHINKOU-IPPAN-014).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kudo, D., Uno, K., Aoyagi, T. et al. Low-dose Interferon-α Treatment Improves Survival and Inflammatory Responses in a Mouse Model of Fulminant Acute Respiratory Distress Syndrome. Inflammation 36, 812–820 (2013). https://doi.org/10.1007/s10753-013-9607-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-013-9607-1