Abstract
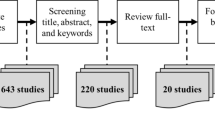
While healthcare entities have integrated various forms of health information technology (HIT) into their systems due to claims of increased quality and decreased costs, as well as various incentives, there is little available information about which applications of HIT are actually the most beneficial and efficient. In this study, we aim to assist administrators in understanding the characteristics of top performing hospitals. We utilized data from the Health Information and Management Systems Society and the Center for Medicare and Medicaid to assess 1039 hospitals. Inputs considered were full time equivalents, hospital size, and technology inputs. Technology inputs included personal health records (PHR), electronic medical records (EMRs), computerized physician order entry systems (CPOEs), and electronic access to diagnostic results. Output variables were measures of quality, hospital readmission and mortality rate. The analysis was conducted in a two-stage methodology: Data Envelopment Analysis (DEA) and Automatic Interaction Detector Analysis (AID), decision tree regression (DTreg). Overall, we found that electronic access to diagnostic results systems was the most influential technological characteristics; however organizational characteristics were more important than technological inputs. Hospitals that had the highest levels of quality indicated no excess in the use of technology input, averaging one use of a technology component. This study indicates that prudent consideration of organizational characteristics and technology is needed before investing in innovative programs.


Similar content being viewed by others
References
Rajagopal N (2013) Impact of information technology on service quality of health care dervices. Vilakshan: XIMB J Manag 10(1):79–96
Levaggi R, Moretto M, Rebba V (2009) Investment decisions in hospital technology when physicians are devoted workers. Econ Innov New Technol 18(5/6):487–512
Kunstova R, Potancok M (2013) How to measure benefits of non-standard healthcare systems. Eng Econ 24(2):119–125
Belanger E, Bartlett G, Dawes M, Rodriguez C, Hasson-Gidoni I (2012) Examining the evidence of the impact of health information technology in primary care: an argument for participatory research with health professionals and patients. Int J Med Inform 81:654–661
Archer N, Fevrier-Thomas U, Lokker C, McKibbon KA, Straus SE (2011) Personal health records: a scoping review. J Am Med Inform Assoc 18(4):515–522
Wynia M, Torres GW, Lemieux J (2011) Many physicians are willing to use patients’ electronic personal health records, but doctors differ by location, gender, and practice. Health Aff 30(2):266–273
Druss B, Ji X, Glick G, von Esenwein S (2014) Randomized trial of an electronic personal health record for patients with serious mental illnesses. Am J Psychiatr 171:360–368
Tenforde M, Nowacki A, Jain A, Hickner J (2012) The association between personal health record use and diabetes quality measures. J Gen Intern Med 27(4):420–424
Goodwin JS, Jinhyung L, Yong-Fang K (2013) The effect of electronic medical record adoption on outcomes in US hospitals. BMC Health Serv Res 13(1):1–7
Karsh B, Beasley J, Hagenauer M (2004) Are electronic medical records associated with improved perceptions of the quality of medical records, working conditions, or quality of working life? Behav Inform Technol 23(5):327–335
Rantz M, Hicks L, Petroski G, Madsen R, Alexander G et al (2010) Cost, staffing and quality impact of bedside electronic medical record (EMR) in nursing homes. J Am Med Dir Assoc 11:485–493
Fairley C, Vodstrcil L, Huffam S, Cummings R, Chen M (2013) Evaluation of electronic medical record (EMR) at large urban primary care sexual health centre. PLOS One 8(4)
Minesh P, Isha P, Chang J, Rachel R, Jatin SA, Rajesh B (2012) Computerized physician order entry (CPOE) systems- an introduction. J Pharm Res 5(10):4962–4967
Lluch M (2011) Healthcare professionals’ organizational barriers to health informationtechnologies—a literature review. Int J Med Inform 80(2011):849–862
Charles K, Cannon M, Hall R, Coustasse A (2014) Can utilizing a computerized provider order entry (CPOE) system prevent hospital medical errors and adverse drug events? Perspectives in Health Information Management 1–16
Simon S, Keohane C, Amato M, Coffey M, Cadet B et al (2013) Lessons learned from implementation of computerized provider order entry in 5 community hospitals: a qualitative study. BMC Med Inform Decis Mak 13(1):1–10
Teufel R, Kazley A, Basco W (2012) Is computerized physician order entry use associated with a decrease in hospital resource in hospitals that care for children? J Med Syst 36(4):2411–2420
Hurlen P, Østbye T, Borthne AS, Gulbrandsen P (2010) Does improved access to diagnostic imaging results reduce hospital length of stay? A retrospective study. BMC Health Serv Res 10:262–266
Byrne S, Barrett B, Bhatia R (2015) The impact of diagnostic imagining wait times on the prognosis of lung cancer. Can Assoc Radiol J 66:53–57
Kantor M, Evans K, Shieh L (2015) Pending studies at hospital discharge: a pre- post analysis of an electronic medical record too to improve communication at hospital. J Gen Intern Med 30(3):312–318
Patience A, Amir N, Ellis CJ, O’Sullivan AT, Faasse K, Gamble G, Petrie K (2015) Does the early feedback of results improve reassurance following diagnostic testing? A randomized controlled trial in patients undergoing cardiac investigation. Health Psychol 34(3):216–221
How can health IT improve efficiency of care delivery? http://www.hrsa.gov/healthit/toolbox/childrenstoolbox/improvingquality/efficiencyofcare.html. Accessed 25 Feb 2015
Donabedian A (1983) Quality, cost, and clinical decisions. Ann Am Acad Pol Soc Sci 468:196–204
Zervopoulos P, Palaskas T (2011) Applying quality-driven, efficiency-adjusted DEA (QE-DEA) in the pursuit of high-efficiency–high-quality service units: an input-oriented approach. IMA J Manag Math 22(4):401–417
Donabedian A, John RCW, Wyszewianski L (1982) Quality, cost, and health: an integrative model. Medical Care p. 976
Donabedian A, John RCW, Wyszewianski L (1982) Quality, cost, and health: an integrative model. Medical Care 975–992
McKinney M (2012) Right there all along. Latest IOM report lays out how to deliver safer, more effective care by using existing strategies, technology. Mod Healthc 42(37):6
Jones S, Rudin RS, Schneider EC, Heaton PS (2012) Unraveling the IT productivity paradox—lessons for health care. N Engl J Med 366(24):2243–2245
Hebert M (1998) Impact of IT on health care professionals: changes in work and the productivity paradox. Health Serv Manag Res 11(2):69–79
Salzbert C, Jang Y, Rozenblum R, Zimlichman E, Tamblyn R, Bates D (2012) Policy initiatives for health information technology: a qualitative study of U.S. expectations and Canada’s experience. Int J Med Inform 81:713–722
Silverman R (2013) EHRs, EMRs, and health information technology: to meaningful use and beyond. J Leg Med 34:1–6
Appari A, Carian EK, Johnson ME, Anthony DL (2012) Medication administration quality and health information technology: a national study of US hospitals. J Am Med Inform Assoc 19(3):360–367
Hikmet N, Bhattacherjee A, Menachemi N, Kkakyhan V, Brooks R (2008) The role of organizational factors in the adoption of healthcare information technology in Florida hospitals. Health Care Manag Sci 11:1–9
Navarro-Espigares JL, Torres EH (2011) Efficiency and quality in health services: a crucial link. Serv Ind J 31(3):385–403
Kern L, Wilcox A, Shapiro J, Yoon-Flannery K, Abramson E, Barron Y, Kaushal R (2011) Community-based health information technology alliances: potential predictors of early sustainability. Am J Manag Care 17(4):290–295
Buntin MB, Burke MF, Hoaglin MC, Blumenthal D (2011) The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff 30(3):464–471
Zhivan N, Diana M (2012) U.S. hospital efficiency and adoption of health information technology. Health Care Manag Sci 15(1):37–47
Chuang C-L, Chang P-C, Lin R-H (2011) An efficiency data envelopment analysis model reinforced by classification and regression tree for hospital performance evaluation. J Med Syst 35(5):1075–1083
Rahimi I, Behmanesh R (2012) Improve poultry farm efficiency in Iran: using combination neural networks, decision trees, and data envelopment analysis (DEA). Int J Appl Oper Res (3)
Ozcan YA (2014) Health care benchmarking and performance evaluation: an assessment using data envelopment analysis (Dea). Springer, New York
Kass GV (1975) Significance testing in automatic interaction detection (A.I.D). J R Stat Soc: Ser C: Appl Stat 24(2):178
HCAPHS Hospital Survey. http://www.hcahpsonline.org/. Accessed 20 Oct 2013
Dicks S, Chaplin R, Hood C (2013) Factors affecting care on acute hospital wards. Nurs Older People 25(1):18–23
Kuwahara Y, Nagata S, Taguchi A, Naruse T, Kawaguchi H, Murashima S (2013) Measuring the efficiencies of visiting nurse service agencies using data envelopment analysis. Health Care Manag Sci 16(3):228–235
McHugh M, Berez J, Small D (2013) Hospitals with higher nurse staffing had lower odds of readmissions penalties than hospitals with lower staffing. Health Aff 32(10):1740–1747
McFarland D, Ornstein K, & Holcombe R. (2015) Demographic factors and hospital size predict patient satisfaction variance-implications for hospital value-based purchasing. J Hosp Med
Lieberthal R, Comer D (2014) What are the characteristics that explain hospital quality? A longitudinal pridit approach. Risk Manage Insur Rev 17(1):17–35
Electronic access to results does not decrease use of diagnostic test (2012) Am Fam Phys 85(8): 754
McCormick D, Bor DH, Woolhandler S, Himmelstein DU (2012) Giving office- based physicians electronic access to patients’ prior imaging and lab resuls did not deer ordering of tests. Health Aff 31(3):488–496
Neale G, Hogan H, Sevdalis N (2011) Misdiagnosis: analysis based on case record review with proposals aimed to improve diagnostic processes. Clin Med 11(4):317–321
Boothby D, Dufour A, Tang J (2010) Technology adoption, training and productivity performance. Res Policy 39(5):650–661
Conflict of interest
The authors declare that they have no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Williams, C., Asi, Y., Raffenaud, A. et al. The effect of information technology on hospital performance. Health Care Manag Sci 19, 338–346 (2016). https://doi.org/10.1007/s10729-015-9329-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-015-9329-z