Abstract
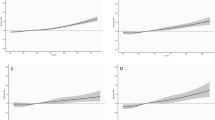
Previous studies suggest that abnormal energy balance status may dysregulate intestinal epithelial homeostasis and promote colorectal carcinogenesis, yet little is known about how host energy balance and obesity influence enterocyte differentiation during carcinogenesis. We hypothesized that the association between high body mass index (BMI) and colorectal carcinoma incidence might differ according to tumor histopathologic differentiation status. Using databases of the Nurses’ Health Study and Health Professionals Follow-up Study, and duplication-method Cox proportional hazards models, we prospectively examined an association between BMI and the incidence of colorectal carcinoma subtypes classified by differentiation features. 120,813 participants were followed for 26 or 32 years and 1528 rectal and colon cancer cases with available tumor pathological data were documented. The association between BMI and colorectal cancer risk significantly differed depending on the presence or absence of poorly-differentiated foci (Pheterogeneity = 0.006). Higher BMI was associated with a higher risk of colorectal carcinoma without poorly-differentiated foci (≥30.0 vs. 18.5–22.4 kg/m2: multivariable-adjusted hazard ratio, 1.87; 95% confidence interval, 1.49–2.34; Ptrend < 0.001), but not with risk of carcinoma with poorly-differentiated foci (Ptrend = 0.56). This differential association appeared to be consistent in strata of tumor microsatellite instability or FASN expression status, although the statistical power was limited. The association between BMI and colorectal carcinoma risk did not significantly differ by overall tumor differentiation, mucinous differentiation, or signet ring cell component (Pheterogeneity > 0.03, with the adjusted α of 0.01). High BMI was associated with risk of colorectal cancer subtype containing no poorly-differentiated focus. Our findings suggest that carcinogenic influence of excess energy balance might be stronger for tumors that retain better intestinal differentiation throughout the tumor areas.
Similar content being viewed by others
Abbreviations
- AHEI:
-
Alternate Healthy Eating Index
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- FFPE:
-
Formalin-fixed paraffin-embedded
- HPFS:
-
Health Professionals Follow-up Study
- HR:
-
Hazard ratio
- ISC:
-
Intestinal stem cells
- METS:
-
Metabolic equivalent task score
- MPE:
-
Molecular pathological epidemiology
- MSI:
-
Microsatellite instability
- MSS:
-
Microsatellite stable
- NHS:
-
Nurses’ Health Study
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- SD:
-
Standard deviation
- WHO:
-
World Health Organization
References
Renehan AG, Soerjomataram I, Tyson M, Egger M, Zwahlen M, Coebergh JW, Buchan I. Incident cancer burden attributable to excess body mass index in 30 European countries. Int J Cancer. 2010;126(3):692–702.
Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet. 2014;384(9945):755–65.
Kuipers EJ, Grady WM, Lieberman D, Seufferlein T, Sung JJ, Boelens PG, van de Velde CJH, Watanabe T. Colorectal cancer. Nat Rev Dis Primers. 2015;1:15065.
Martinez-Useros J, Garcia-Foncillas J. Obesity and colorectal cancer: molecular features of adipose tissue. J Transl Med. 2016;14(1):21.
Ma Y, Yang Y, Wang F, Zhang P, Shi C, Zou Y, Qin H. Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS ONE. 2013;8(1):e53916.
Booth A, Magnuson A, Fouts J, Foster M. Adipose tissue, obesity and adipokines: role in cancer promotion. Horm Mol Biol Clin Investig. 2015;21(1):57–74.
Fedirko V, Romieu I, Aleksandrova K, Pischon T, Trichopoulos D, Peeters PH, Romaguera-Bosch D, Bueno-de-Mesquita HB, Dahm CC, Overvad K, Chirlaque MD, Johansen C, Bidstrup PE, Dalton SO, Gunter MJ, Wark PA, Norat T, Halkjaer J, Tjonneland A, Dik VK, Siersema PD, Boutron-Ruault MC, Dossus L, Bastide N, Kuhn T, Kaaks R, Boeing H, Trichopoulou A, Klinaki E, Katsoulis M, Pala V, Panico S, Tumino R, Palli D, Vineis P, Weiderpass E, Skeie G, Gonzalez CA, Sanchez MJ, Barricarte A, Amiano P, Quiros JR, Manjer J, Jirstrom K, Ljuslinder I, Palmqvist R, Khaw KT, Wareham N, Bradbury KE, Stepien M, Duarte-Salles T, Riboli E, Jenab M. Pre-diagnostic anthropometry and survival after colorectal cancer diagnosis in Western European populations. Int J Cancer. 2014;135(8):1949–60.
Campbell PT, Newton CC, Newcomb PA, Phipps AI, Ahnen DJ, Baron JA, Buchanan DD, Casey G, Cleary SP, Cotterchio M, Farris AB, Figueiredo JC, Gallinger S, Green RC, Haile RW, Hopper JL, Jenkins MA, Le Marchand L, Makar KW, McLaughlin JR, Potter JD, Renehan AG, Sinicrope FA, Thibodeau SN, Ulrich CM, Win AK, Lindor NM, Limburg PJ. Association between body mass index and mortality for colorectal cancer survivors: overall and by tumor molecular phenotype. Cancer Epidemiol Biomarkers Prev. 2015;24(8):1229–38.
McLeod CJ, Wang L, Wong C, Jones DL. Stem cell dynamics in response to nutrient availability. Curr Biol. 2010;20(23):2100–5.
O’Brien LE, Soliman SS, Li X, Bilder D. Altered modes of stem cell division drive adaptive intestinal growth. Cell. 2011;147(3):603–14.
Stelzner M, Helmrath M, Dunn JC, Henning SJ, Houchen CW, Kuo C, Lynch J, Li L, Magness ST, Martin MG, Wong MH, Yu J. A nomenclature for intestinal in vitro cultures. Am J Physiol Gastrointest Liver Physiol. 2012;302(12):G1359–63.
Yilmaz OH, Katajisto P, Lamming DW, Gultekin Y, Bauer-Rowe KE, Sengupta S, Birsoy K, Dursun A, Yilmaz VO, Selig M, Nielsen GP, Mino-Kenudson M, Zukerberg LR, Bhan AK, Deshpande V, Sabatini DM. mTORC1 in the Paneth cell niche couples intestinal stem-cell function to calorie intake. Nature. 2012;486(7404):490–5.
Mah AT, Van Landeghem L, Gavin HE, Magness ST, Lund PK. Impact of diet-induced obesity on intestinal stem cells: hyperproliferation but impaired intrinsic function that requires insulin/IGF1. Endocrinology. 2014;155(9):3302–14.
Beyaz S, Mana MD, Roper J, Kedrin D, Saadatpour A, Hong SJ, Bauer-Rowe KE, Xifaras ME, Akkad A, Arias E, Pinello L, Katz Y, Shinagare S, Abu-Remaileh M, Mihaylova MM, Lamming DW, Dogum R, Guo G, Bell GW, Selig M, Nielsen GP, Gupta N, Ferrone CR, Deshpande V, Yuan GC, Orkin SH, Sabatini DM, Yilmaz OH. High-fat diet enhances stemness and tumorigenicity of intestinal progenitors. Nature. 2016;531(7592):53–8.
Blomain ES, Waldman SA. Does obesity promote the development of colorectal cancer? Expert Rev Anticancer Ther. 2016;16(5):465–7.
Wang D, Fu L, Ning W, Guo L, Sun X, Dey SK, Chaturvedi R, Wilson KT, DuBois RN. Peroxisome proliferator-activated receptor δ promotes colonic inflammation and tumor growth. Proc Natl Acad Sci USA. 2014;111(19):7084–9.
Colussi D, Brandi G, Bazzoli F, Ricciardiello L. Molecular pathways involved in colorectal cancer: implications for disease behavior and prevention. Int J Mol Sci. 2013;14(8):16365–85.
Kocarnik JM, Shiovitz S, Phipps AI. Molecular phenotypes of colorectal cancer and potential clinical applications. Gastroenterol Rep (Oxf). 2015;3(4):269–76.
Kudryavtseva AV, Lipatova AV, Zaretsky AR, Snezhkina AV, Kaprin AD, Alekseev BY. Important molecular genetic markers of colorectal cancer. Oncotarget. 2016;7(33):53959–83.
Ogino S, Brahmandam M, Cantor M, Namgyal C, Kawasaki T, Kirkner G, Meyerhardt JA, Loda M, Fuchs CS. Distinct molecular features of colorectal carcinoma with signet ring cell component and colorectal carcinoma with mucinous component. Mod Pathol. 2006;19(1):59–68.
Ogino S, Odze RD, Kawasaki T, Brahmandam M, Kirkner GJ, Laird PW, Loda M, Fuchs CS. Correlation of pathologic features with CpG island methylator phenotype (CIMP) by quantitative DNA methylation analysis in colorectal carcinoma. Am J Surg Pathol. 2006;30(9):1175–83.
Ogino S, Kawasaki T, Ogawa A, Kirkner GJ, Loda M, Fuchs CS. Fatty acid synthase overexpression in colorectal cancer is associated with microsatellite instability, independent of CpG island methylator phenotype. Hum Pathol. 2007;38(6):842–9.
Haydon AMM, Jass JR. Emerging pathways in colorectal-cancer development. Lancet Oncol. 2002;3(2):83–8.
Rossi S, Graner E, Febbo P, Weinstein L, Bhattacharya N, Onody T, Bubley G, Balk S, Loda M. Fatty acid synthase expression defines distinct molecular signatures in prostate cancer. Mol Cancer Res. 2003;1(10):707–15.
Kuhajda FP. Fatty acid synthase and cancer: new application of an old pathway. Cancer Res. 2006;66(12):5977–80.
Rashid A, Pizer ES, Moga M, Milgraum LZ, Zahurak M, Pasternack GR, Kuhajda FP, Hamilton SR. Elevated expression of fatty acid synthase and fatty acid synthetic activity in colorectal neoplasia. Am J Pathol. 1997;150(1):201–8.
Luque-Garcia JL, Martinez-Torrecuadrada JL, Epifano C, Canamero M, Babel I, Casal JI. Differential protein expression on the cell surface of colorectal cancer cells associated to tumor metastasis. Proteomics. 2010;10(5):940–52.
Carvalho MA, Zecchin KG, Seguin F, Bastos DC, Agostini M, Rangel AL, Veiga SS, Raposo HF, Oliveira HC, Loda M, Coletta RD, Graner E. Fatty acid synthase inhibition with Orlistat promotes apoptosis and reduces cell growth and lymph node metastasis in a mouse melanoma model. Int J Cancer. 2008;123(11):2557–65.
Murata S, Yanagisawa K, Fukunaga K, Oda T, Kobayashi A, Sasaki R, Ohkohchi N. Fatty acid synthase inhibitor cerulenin suppresses liver metastasis of colon cancer in mice. Cancer Sci. 2010;101(8):1861–5.
Slattery ML, Curtin K, Anderson K, Ma KN, Ballard L, Edwards S, Schaffer D, Potter J, Leppert M, Samowitz WS. Associations between cigarette smoking, lifestyle factors, and microsatellite instability in colon tumors. J Natl Cancer Inst. 2000;92(22):1831–6.
Satia JA, Keku T, Galanko JA, Martin C, Doctolero RT, Tajima A, Sandler RS, Carethers JM. Diet, lifestyle, and genomic instability in the North Carolina Colon Cancer Study. Cancer Epidemiol Biomarkers Prev. 2005;14(2):429–36.
Campbell PT, Jacobs ET, Ulrich CM, Figueiredo JC, Poynter JN, McLaughlin JR, Haile RW, Jacobs EJ, Newcomb PA, Potter JD, Le ML, Green RC, Parfrey P, Younghusband HB, Cotterchio M, Gallinger S, Jenkins MA, Hopper JL, Baron JA, Thibodeau SN, Lindor NM, Limburg PJ, Martinez ME, Family CC, Colon Cancer Family R. Case-control study of overweight, obesity, and colorectal cancer risk, overall and by tumor microsatellite instability status. J Natl Cancer Inst. 2010;102(6):391–400.
Hughes LA, Williamson EJ, van Engeland M, Jenkins MA, Giles GG, Hopper JL, Southey MC, Young JP, Buchanan DD, Walsh MD, van den Brandt PA, Alexandra Goldbohm R, Weijenberg MP, English DR. Body size and risk for colorectal cancers showing BRAF mutations or microsatellite instability: a pooled analysis. Int J Epidemiol. 2012;41(4):1060–72.
Hoffmeister M, Blaker H, Kloor M, Roth W, Toth C, Herpel E, Frank B, Schirmacher P, Chang-Claude J, Brenner H. Body mass index and microsatellite instability in colorectal cancer: a population-based study. Cancer Epidemiol Biomarkers Prev. 2013;22(12):2303–11.
Hanyuda A, Ogino S, Rong Qian Z, Nishihara R, Song M, Mima K, Inamura K, Masugi Y, Wu K, Meyerhardt JA, Chan AT, Fuchs CS, Giovannucci EL, Cao Y. Body mass index and risk of colorectal cancer according to tumor lymphocytic infiltrate. Int J Cancer. 2016;139:854–68.
Kuchiba A, Morikawa T, Yamauchi M, Imamura Y, Liao X, Chan AT, Meyerhardt JA, Giovannucci E, Fuchs CS, Ogino S. Body mass index and risk of colorectal cancer according to fatty acid synthase expression in the Nurses’ Health Study. J Natl Cancer Inst. 2012;104(5):415–20.
Ogino S, Chan AT, Fuchs CS, Giovannucci E. Molecular pathological epidemiology of colorectal neoplasia: an emerging transdisciplinary and interdisciplinary field. Gut. 2011;60(3):397–411.
Ogino S, Lochhead P, Chan AT, Nishihara R, Cho E, Wolpin BM, Meyerhardt JA, Meissner A, Schernhammer ES, Fuchs CS, Giovannucci E. Molecular pathological epidemiology of epigenetics: emerging integrative science to analyze environment, host, and disease. Mod Pathol. 2013;26(4):465–84.
Ogino S, Campbell PT, Nishihara R, Phipps AI, Beck AH, Sherman ME, Chan AT, Troester MA, Bass AJ, Fitzgerald KC, Irizarry RA, Kelsey KT, Nan H, Peters U, Poole EM, Qian ZR, Tamimi RM, Tchetgen Tchetgen EJ, Tworoger SS, Zhang X, Giovannucci EL, van den Brandt PA, Rosner BA, Wang M, Chatterjee N, Begg CB. Proceedings of the second international molecular pathological epidemiology (MPE) meeting. Cancer Causes Control. 2015;26(7):959–72.
Hamada T, Keum N, Nishihara R, Ogino S. Molecular pathological epidemiology: new developing frontiers of big data science to study etiologies and pathogenesis. J Gastroenterol. 2017;52(3):265–75.
Rimm EB, Giovannucci EL, Willett WC, Colditz GA, Ascherio A, Rosner B, Stampfer MJ. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet. 1991;338(8765):464–8.
Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Women’s Heal. 1997;6(1):49–62.
Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1(6):466–73.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–12, 1–253.
World Health Organization Classification of Tumours of the Digestive System. Lyon: International Agency for Research on Cancer (IARC); 2010. p. 134–146.
Ogino S, Nosho K, Kirkner GJ, Kawasaki T, Meyerhardt JA, Loda M, Giovannucci EL, Fuchs CS. CpG island methylator phenotype, microsatellite instability, BRAF mutation and clinical outcome in colon cancer. Gut. 2009;58(1):90–6.
Wang M, Spiegelman D, Kuchiba A, Lochhead P, Kim S, Chan AT, Poole EM, Tamimi R, Tworoger SS, Giovannucci E, Rosner B, Ogino S. Statistical methods for studying disease subtype heterogeneity. Stat Med. 2016;35(5):782–800.
Cao Y, Nishihara R, Qian ZR, Song M, Mima K, Inamura K, Nowak JA, Drew DA, Lochhead P, Nosho K, Morikawa T, Zhang X, Wu K, Wang M, Garrett WS, Giovannucci EL, Fuchs CS, Chan AT, Ogino S. Regular aspirin use associates with lower risk of colorectal cancers with low numbers of tumor-infiltrating lymphocytes. Gastroenterology. 2016;151(5):879–92.
Song M, Nishihara R, Wang M, Chan AT, Qian ZR, Inamura K, Zhang X, Ng K, Kim SA, Mima K, Sukawa Y, Nosho K, Fuchs CS, Giovannucci EL, Wu K, Ogino S. Plasma 25-hydroxyvitamin D and colorectal cancer risk according to tumour immunity status. Gut. 2016;65(2):296–304.
Aleman JO, Eusebi LH, Ricciardiello L, Patidar K, Sanyal AJ, Holt PR. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology. 2014;146(2):357–73.
Hagland HR, Soreide K. Cellular metabolism in colorectal carcinogenesis: influence of lifestyle, gut microbiome and metabolic pathways. Cancer Lett. 2015;356(2 Pt A):273–80.
Renehan AG, Zwahlen M, Egger M. Adiposity and cancer risk: new mechanistic insights from epidemiology. Nat Rev Cancer. 2015;15(8):484–98.
Hughes LA, Simons CC, van den Brandt PA, Goldbohm RA, de Goeij AF, de Bruine AP, van Engeland M, Weijenberg MP. Body size, physical activity and risk of colorectal cancer with or without the CpG island methylator phenotype (CIMP). PLoS ONE. 2011;6(4):e18571.
Wang D, Dubois RN. Associations between obesity and cancer: the role of fatty acid synthase. J Natl Cancer Inst. 2012;104(5):343–5.
Song M, Garrett WS, Chan AT. Nutrients, foods, and colorectal cancer prevention. Gastroenterology. 2015;148(6):1244–60.
Buron Pust A, Alison R, Blanks R, Pirie K, Gaitskell K, Barnes I, Gathani T, Reeves G, Beral V, Green J. Heterogeneity of colorectal cancer risk by tumour characteristics: large prospective study of UK women. Int J Cancer. 2017;140(5):1082–90.
Mihaylova MM, Sabatini DM, Yilmaz OH. Dietary and metabolic control of stem cell function in physiology and cancer. Cell Stem Cell. 2014;14(3):292–305.
Tomasetti C, Vogelstein B. Cancer etiology. Variation in cancer risk among tissues can be explained by the number of stem cell divisions. Science (80-). 2015;347(6217):78–81.
Wu S, Powers S, Zhu W, Hannun YA. Substantial contribution of extrinsic risk factors to cancer development. Nature. 2016;529(7584):43–7.
Uddin S, Hussain AR, Ahmed M, Abubaker J, Al-Sanea N, Abduljabbar A, Ashari LH, Alhomoud S, Al-Dayel F, Bavi P, Al-Kuraya KS. High prevalence of fatty acid synthase expression in colorectal cancers in Middle Eastern patients and its potential role as a therapeutic target. Am J Gastroenterol. 2009;104(7):1790–801.
Zaidi N, Lupien L, Kuemmerle NB, Kinlaw WB, Swinnen JV, Smans K. Lipogenesis and lipolysis: the pathways exploited by the cancer cells to acquire fatty acids. Prog Lipid Res. 2013;52(4):585–9.
Ogino S, Nishihara R, VanderWeele TJ, Wang M, Nishi A, Lochhead P, Qian ZR, Zhang X, Wu K, Nan H, Yoshida K, Milner DA Jr, Chan AT, Field AE, Camargo CA Jr, Williams MA, Giovannucci EL. Review article: the role of molecular pathological epidemiology in the study of neoplastic and non-neoplastic diseases in the era of precision medicine. Epidemiology. 2016;27(4):602–11.
Ikram MA, van der Lugt A, Niessen WJ, Koudstaal PJ, Krestin GP, Hofman A, Bos D, Vernooij MW. The Rotterdam Scan Study: design update 2016 and main findings. Eur J Epidemiol. 2015;30(12):1299–315.
Nishihara R, VanderWeele TJ, Shibuya K, Mittleman MA, Wang M, Field AE, Giovannucci E, Lochhead P, Ogino S. Molecular pathological epidemiology gives clues to paradoxical findings. Eur J Epidemiol. 2015;30(10):1129–35.
Snijder MB, van Dam RM, Visser M, Seidell JC. What aspects of body fat are particularly hazardous and how do we measure them? Int J Epidemiol. 2006;35(1):83–92.
Acknowledgements
We would like to thank the participants and staff of the Nurses’ Health Study and the Health Professionals Follow-up Study for their valuable contributions as well as the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. The authors assume full responsibility for analyses and interpretation of these data.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by US National Institutes of Health (NIH) Grants [UM1 CA186107 and P01 CA87969 to Meir J. Stampfer; P01 CA55075 and UM1 CA167552 to Walter C. Willett; K07 CA190673 to R.N.; R01 CA137178 and K24 DK098311 to A.T.C.; P50 CA127003 to C.S.F.; R01 CA151993 and R35 CA197735 to S.O.], by Nodal Award from the Dana-Farber Harvard Cancer Center (to S.O.); and by grants from the Project P Fund, the Friends of the Dana-Farber Cancer Institute, the Bennett Family Fund and the Entertainment Industry Foundation through National Colorectal Cancer Research Alliance. A.H. was supported by the Japan-United States Educational Exchange Promotion Foundation (Fulbright Foundation), Japan and the U.S. T.H. was supported by a fellowship grant from the Uehara Memorial Foundation and by a grant from the Mochida Memorial Foundation for Medical and Pharmaceutical Research. Y.M. was supported by a fellowship grant of the Keio Gijuku Fukuzawa Memorial Fund for the Advancement of Education and Research. A.T.C. was a Damon Runyon Clinical Investigator.
Conflict of interest
A.T.C. previously served as a consultant for Bayer Healthcare, Pozen Inc, and Pfizer Inc. This study was not funded by Bayer Healthcare, Millennium Pharmaceuticals, or Pfizer Inc. All remaining authors have declared no conflicts of interest.
Additional information
We use HUGO (Human Genome Organisation)-approved official symbols for genes (italics) and gene products (non-italics), including CTNNB1, FASN, and PPARD; all of which are described at www.genenames.org.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hanyuda, A., Cao, Y., Hamada, T. et al. Body mass index and risk of colorectal carcinoma subtypes classified by tumor differentiation status. Eur J Epidemiol 32, 393–407 (2017). https://doi.org/10.1007/s10654-017-0254-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-017-0254-y