Summary
Salinomycin (Sal) is potentially useful for the treatment of cancer. The present study examined a novel mechanism of Sal sensitization in cancer cells. Sal sensitized radiation-treated cancer cells by inducing G2 arrest and causing DNA damage. Sal treatment also reduced p21 levels in radiation-treated cells. Considering that Sal sensitizes doxorubicin (DOX)- or etoposide (ETO)-treated cancer cells by causing DNA damage and reducing p21 expression, the results from our study suggest that the mechanism underlying Sal sensitization is conserved in both chemo- and radiation-treated cells. We also tested the ability of Sal to inhibit p-glycoprotein (P-gp), which plays a role in the efflux of anti-cancer drugs to reduce cellular damage. In particular, we compared Sal to verapamil (Ver), a well-known P-gp inhibitor. Sal inhibits P-gp with a different substrate distinct from that of Ver. In addition, Sal sensitized Ver-resistant cells, indicating that this compound is more effective for sensitizing than Ver. Taken together, the results from our study may contribute to the development of Sal-based therapy for cancer patients treated with P-gp-inhibiting drugs or radiation therapy.




Similar content being viewed by others
Abbreviations
- DOX:
-
doxorubicin
- DMSO:
-
dimethylsulfoxide
- ETO:
-
etoposide
- Sal:
-
salinomycin
- Ver:
-
verapamil
- MDR:
-
multi-drug resistance
- P-gp:
-
p-glycoprotein
- FACS:
-
fluorescence-activated cell sorting
- Rho:
-
rhodamin123
- CFDA:
-
carboxyfluorescein diacetate
- DAPI:
-
4′-6-diamidino-2-phenylindole
- FBS:
-
fetal bovine serum
- BSA:
-
bovine serum albumin
- TCA:
-
trichloroacetic acid
- PBS:
-
phosphate buffered saline
- SDS-PAGE:
-
sodium dodecyl sulfate-polyacrylamide gel electrophoresis
- TUNEL:
-
terminal transferase dUTP nick end labeling
References
Miyazaki Y, Shibuya M, Sugawara H, Kawaguchi O, Hirsoe C (1974) Salinomycin, a new polyether antibiotic. J Antibiot 27:814–821
Mahmoudi N, de Julián-Ortiz JV, Ciceron L, Gálvez J, Mazier D, Danis M, Derouin F, Garcia-Domenech R (2006) Identification of new antimalarial drugs by linear discriminant analysis and topological virtual screening. J Antimicrob Chemother 57:489–497. doi:10.1093/jac/dki470
Gupta PB, Onder TT, Jiang G, Tao K, Kuperwasser C, Weinberg RA, Lander ES (2009) Identification of selective inhibitors of cancer stem cells by high-throughput screening. Cell 138:645–659. doi:10.1016/j.cell.2009.06.034
O’Connor R (2007) The pharmacology of cancer resistance. Anticancer Res 27:1267–1272
Yang K, Wu J, Li X (2008) Recent advances in the research of P-glycoprotein inhibitors. Biosci Trends 2:137–146
Shukla S, Wu CP, Ambudkar SV (2008) Development of inhibitors of ATP-binding cassette drug transporters: present status and challenges. Expert Opin Drug Metab Toxicol 4:205–223. doi:10.1517/17425255.4.2.205
Fuchs D, Heinold A, Opelz G, Daniel V, Naujokat C (2009) Salinomycin induces apoptosis and overcomes apoptosis resistance in human cancer cells. Biochem Biophys Res Commun 390:743–749. doi:10.1016/j.bbrc.2009.10.042
Fuchs D, Daniel V, Sadeghi M, Opelz G, Naujokat C (2010) Salinomycin overcomes ABC transporter-mediated multidrug and apoptosis resistance in human leukemia stem cell-like KG-1a cells. Biochem Biophys Res Commun 394:1098–1104. doi:10.1016/j.bbrc.2010.03.138
Riccioni R, Dupuis ML, Bernabei M, Petrucci E, Pasquini L, Mariani G, Cianfriglia M, Testa U (2010) The cancer stem cell selective inhibitor salinomycin is a p-glycoprotein inhibitor. Blood Cells Mol Dis 45:86–92. doi:10.1016/j.bcmd.2010.03.008
Wang Y (2011 Jan 11) Effects of salinomycin on cancer stem cell in human lung adenocarcinoma A549 cells. Med Chem [Epub ahead of print]
Dong TT, Zhou HM, Wang LL, Feng B, Lv B, Zheng MH (2011 Jan 26) Salinomycin selectively targets ‘CD133+’ cell subpopulations and decreases malignant traits in colorectal cancer lines. Ann Surg Oncol [Epub ahead of print]. doi:10.1245/s10434-011-1561-2
Gong C, Yao H, Liu Q, Chen J, Shi J, Su F, Song E (2010) Markers of tumor-initiating cells predict chemoresistance in breast cancer. PLoS ONE 5:e15630. doi:10.1371/journal.pone.0015630
Bardsley MR, Horvàth VJ, Asuzu DT, Lorincz A, Redelman D, Hayashi Y, Popko LN, Young DL, Lomberk GA, Urrutia RA, Farrugia G, Rubin BP, Ordog T (2010) Kitlow stem cells cause resistance to Kit/platelet-derived growth factor alpha inhibitors in murine gastrointestinal stromal tumors. Gastroenterology 139:942–952. doi:10.1053/j.gastro.2010.05.083
Kim JH, Chae MJ, Kim WK, Kim YJ, Kang HS, Kim HS, Yoon S (2011) Salinomycin sensitizes cancer cells to the effects of doxorubicin and etoposide treatment by increasing DNA damage and reducing p21 protein. Br J Pharmacol 162:773–784. doi:10.1111/j.1476-5381.2010.01089.x
Kim JH, Lee SC, Ro J, Kang HS, Kim HS, Yoon S (2010) Jnk signaling pathway-mediated regulation of Stat3 activation is linked to the development of doxorubicin resistance in cancer cell lines. Biochem Pharmacol 7:373–380. doi:10.1016/j.bcp.2009.09.008
Kim JH, Kim TH, Kang HS, Ro J, Kim HS, Yoon S (2009) SP600125, an inhibitor of Jnk pathway, reduces viability of relatively resistant cancer cells to doxorubicin. Biochem Biophys Res Commun 387:450–455. doi:10.1016/j.bbrc.2009.07.036
Lee KH, Moon KJ, Kim HS, Yoo BC, Park S, Lee H, Kwon S, Lee ES, Yoon S (2008) Increased cytoplasmic levels of CIS, SOCS1, SOCS2, or SOCS3 are required for nuclear translocation. FEBS Lett 582:2319–2324. doi:10.1016/j.febslet.2008.05.039
Dogan AL, Legreand O, Faussat AM, Perrot JY, Marie JP (2004) Evaluation and comparison of MRP1 activity with three fluorescent dyes and three modulators in leukemic cell lines. Leuk Res 28:619–622. doi:10.1016/j.leukres.2003.10.015
Kim YK, Song YJ, Seo DW, Kang DW, Lee HY, Rhee DK, Han JW, Ahn CM, Lee S, Kim SN (2007) Reversal of multidrug resistance by 4-chloro-N-(3-((E)-3-(4-hydroxy-3-methoxyphenyl)acryloyl)phenyl)benzamide through the reversible inhibition of P-glycoprotein. Biochem Biophys Res Commun 355:136–142. doi:10.1016/j.bbrc.2007.01.117
Kweon SH, Song JH, Kim TS (2010) Reveratrol-mediated reversal of doxorubicin resistance in acute myeloid leukemia cells via downregulation of MRP1 expression. Biochem Biophys Res Commun 395:104–110. doi:10.1016/j.bbrc.1010.03.147
Kawabe T (2004) G2 checkpoint abrogators as anticancer drugs. Mol Cancer Ther 3:513–519
Solier S, Sordet O, Kohn KW, Pommier Y (2009) Death receptor-induced activation of the Chk2- and histone H2AX-associated DNA damage response pathways. Mol Cell Biol 29:68–82. doi:10.1128/MCB.00581-08
Inskip PD, Robison LL, Stovall M, Smith SA, Hammond S, Mertens AC, Whitton JA, Diller L, Kenney L, Donaldson SS, Meadows AT, Neglia JP (2009) Radiation dose and breast cancer risk in the childhood cancer survivor study. J Clin Oncol 27:3901–3907. doi:10.1200/JCO.2008.20.7738
Shin HJ, Kim JY, Hampson L, Pyo H, Baek HJ, Roberts SA, Hendry JH, Hampson IN (2010) Human papillomavirus 16 E6 increases the radiosensitivity of p53-mutated cervical cancer cells, associated with up-regulation of aurora A. Int J Radiat Biol 86:769–779. doi:10.3109/09553002.2010.484477
Weiss RH (2003) p21Waf1/Cip1 as a therapeutic target in breast and other cancers. Cancer Cell 4:425–429. doi:10.1016/S1535-6108(03)03308-8
Radhakrishnan SK, Bhat UG, Halasi M, Gartel AL (2008) P-TEFb inhibitors interfere with activation of p53 by DNA-damaging agents. Oncogene 27:1306–1309. doi:10.1038/sj.onc.1210737
Park SH, Wang X, Liu R, Lam KS, Weiss RH (2008) High throughput screening of a small molecule one-bead-one-compound combinatorial library to identify attenuators of p21 as chemotherapy sensitizers. Cancer Biol Ther 7:2015–2022. doi:10.4161/cbt.7.12.7069
Idogawa M, Sasaki Y, Suzuki H, Mita H, Imai K, Shinomura Y, Tokino T (2009) A single recombinant adenovirus expressing p53 and p21-targeting artificial microRNAs efficiently induces apoptosis in human cancer cells. Clin Cancer Res 15:3725–3732. doi:10.1158/1078-0432.CCR-08-2396
Lee EW, Lee MS, Camus S, Ghim J, Yang MR, Oh W, Ha NC, Lane DP, Song J (2009) Differential regulation of p53 and p21 by MKRN1 E3 ligase controls cell cycle arrest and apoptosis. EMBO J 28:2100–2113. doi:10.1038/emboj.2009.164
Acknowledgements
This work was supported by research grant (NCC0910170) from the National Cancer Center, South Korea.
Author information
Authors and Affiliations
Corresponding author
Additional information
Won Ki Kim and Ju-Hwa Kim contributed equally to this work.
Electronic Supplementary Materials
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
Co-treatment with radiation and Sal increases apoptosis. (A-B) Hs578T cells were grown on 60 mm-diameter dishes and then treated with 4 Gy of radiation, 5 μM Sal, 5 μM Sal with 4 Gy of radiation (4 Gy+Sal), or DMSO (Control). After 48 h, Annexin V (A) and TUNEL analyses (B) were performed as described in the “Materials and method” section. (JPEG 16 kb)
Supplementary Fig. 2
Quantification of CFDA and Rho staining confirms that Sal and Ver inhibit different P-gp substrates. (A-B) MCF7 cells were grown and treated for 24 h with 40 μM Ver, 5 μM Sal, or DMSO (Con). The cells were then stained with CFDA (A) or Rho (B). The stained cells were subsequently analyzed using a FACSCalibur flow cytometry system as described in the “Materials and method” section. (JPEG 18 kb)
Supplementary Fig. 3
Higher Sal concentrations do not contribute to increased Rho staining. (A-B) Hs578T and MCF7 cells were grown and treated for 24 h with 5 μM Sal (Sal-5), 10 μM Sal (Sal-10), 15 μM Sal (Sal-15), or DMSO (Con). The cells were then stained with Rho as described in the “Materials and method” section. The stained cells were subsequently examined using an inverted fluorescence microscope with 10× (A) and 16× (B) objective lenses. (JPEG 31 kb)
Supplementary Fig. 4
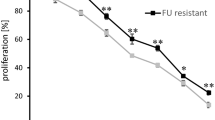
Sal sensitizes relatively Ver-resistant cancer cells. (A-B) Hs578T and MCF7 cells were grown and treated for 24 h with 20 μM Ver (Ver-20), 40 μM Ver (Ver-40), 80 μM Ver (Ver-80), 5 μM Sal (Sal-5), or DMSO (Con). They were subsequently observed using an inverted microscope with a 10× objective lens. (JPEG 35 kb)
Rights and permissions
About this article
Cite this article
Kim, W.K., Kim, JH., Yoon, K. et al. Salinomycin, a p-glycoprotein inhibitor, sensitizes radiation-treated cancer cells by increasing DNA damage and inducing G2 arrest. Invest New Drugs 30, 1311–1318 (2012). https://doi.org/10.1007/s10637-011-9685-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-011-9685-6