Abstract
Purpose
The aim of this study was to determine the diagnostic accuracy, sensitivity and specificity of isolated-check visual evoked potentials (icVEP) in primary open-angle glaucoma (POAG).
Methods
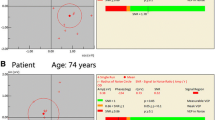
Ninety POAG patients and sixty-six healthy controls were recruited consecutively. All subjects underwent icVEP and visual field testing. Swept icVEP response functions were obtained by increasing contrast in six stimulus steps, recording the electroencephalogram synchronized to the stimulus display’s frame rate and calculating the corresponding signal-to-noise ratio (SNR) of the response at the fundamental frequency to evaluate visual function. Depth of modulation of the check luminance was increased as follows: 2, 4, 8, 14, 22 and 32%, about an equal level of standing contrast, so that the pattern appeared and disappeared at a frequency of 10.0 Hz. SNR above 0.85 was deemed to be significant at the 0.1 level and SNR above 1 significant at the 0.05 level.
Results
The results show that SNR is contrast dependent. It significantly rose as contrast increased. The areas under receiver-operating-characteristic curves (AUCs) indicating classification accuracy for all POAG cases in comparison with normal subjects were 0.790 (sensitivity 91.1%, specificity 69.7%) with the cutoff SNR of 0.85, and 0.706 (sensitivity 95.6%, specificity 51.5%) with the cutoff SNR of 1. The AUC of early glaucoma cases (EG) in comparison with normal subjects was 0.801 (sensitivity 93.3%, specificity 69.7%) with the cutoff SNR of 0.85, and 0.717 (sensitivity 97.8%, specificity 51.5%) with the cutoff SNR of 1.
Conclusion
icVEP has good diagnostic accuracy (high sensitivity and moderate specificity) in distinguishing early POAG patients from healthy subjects. It might be a promising device to use in conjunction with complementary functional and structural measures for early POAG detection.



Similar content being viewed by others
References
Leske MC et al (2003) Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol 121(1):48–56
Kerrigan-Baumrind LA et al (2000) Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Investig Ophthalmol Vis Sci 41(3):741–748
Quigley HA, Dunkelberger GR, Green WR (1989) Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol 107(5):453–464
Glovinsky Y, Quigley HA, Dunkelberger GR (1991) Retinal ganglion cell loss is size dependent in experimental glaucoma. Investig Ophthalmol Vis Sci 32(3):484–491
Glovinsky Y, Quigley HA, Pease ME (1993) Foveal ganglion cell loss is size dependent in experimental glaucoma. Investig Ophthalmol Vis Sci 34(2):395–400
Wen W et al (2015) A novel motion-on-color paradigm for isolating magnocellular pathway function in preperimetric glaucoma. Investig Ophthalmol Vis Sci 56(8):4439–4446
Quigley HA (1998) Identification of glaucoma-related visual field abnormality with the screening protocol of frequency doubling technology. Am J Ophthalmol 125(6):819–829
Kelly DH (1969) Diffusion model of linear flicker responses. J Opt Soc Am 59(12):1665–1670
Sample PA, Bosworth CF, Weinreb RN (1997) Short-wavelength automated perimetry and motion automated perimetry in patients with glaucoma. Arch Ophthalmol 115(9):1129–1133
Anderson AJ et al (2005) Characteristics of the normative database for the Humphrey matrix perimeter. Investig Ophthalmol Vis Sci 46(4):1540–1548
Colotto A et al (2000) Photopic negative response of the human ERG: losses associated with glaucomatous damage. Investig Ophthalmol Vis Sci 41(8):2205–2211
Towle VL et al (1983) The visual evoked potential in glaucoma and ocular hypertension: effects of check size, field size, and stimulation rate. Investig Ophthalmol Vis Sci 24(2):175–183
Baseler HA et al (1994) The topography of visual evoked response properties across the visual field. Electroencephalogr Clin Neurophysiol 90(1):65–81
Hood DC et al (2000) An interocular comparison of the multifocal VEP: a possible technique for detecting local damage to the optic nerve. Investig Ophthalmol Vis Sci 41(6):1580–1587
Mousa MF et al (2013) The role of hemifield sector analysis in multifocal visual evoked potential objective perimetry in the early detection of glaucomatous visual field defects. Clin Ophthalmol 7:843–858
Hicks TP, Lee BB, Vidyasagar TR (1983) The responses of cells in macaque lateral geniculate nucleus to sinusoidal gratings. J Physiol 337:183–200
Derrington AM, Lennie P (1984) Spatial and temporal contrast sensitivities of neurones in lateral geniculate nucleus of macaque. J Physiol 357:219–240
Zemon V et al (2008) Novel electrophysiological instrument for rapid and objective assessment of magnocellular deficits associated with glaucoma. Doc Ophthalmol 117(3):233–243
Zemon V, Gordon J (2006) Luminance-contrast mechanisms in humans: visual evoked potentials and a nonlinear model. Vis Res 46(24):4163–4180
Budenz DL et al (2002) Comparison of glaucomatous visual field defects using standard full threshold and Swedish interactive threshold algorithms. Arch Ophthalmol 120(9):1136–1141
Anderson DR, Parrish RK, Hodapp E (1993) Clinical decisions in glaucoma. St. Louis, Mosby, p 204
Zemon V, Gordon J, Welch J (1988) Asymmetries in ON and OFF visual pathways of humans revealed using contrast-evoked cortical potentials. Vis Neurosci 1(1):145–150
Greenstein VC et al (1998) Visual evoked potential assessment of the effects of glaucoma on visual subsystems. Vis Res 38(12):1901–1911
Victor JD, Mast J (1991) A new statistic for steady-state evoked potentials. Electroencephalogr Clin Neurophysiol 78(5):378–388
Homan RW, Herman J, Purdy P (1987) Cerebral location of international 10–20 system electrode placement. Electroencephalogr Clin Neurophysiol 66(4):376–382
Peirce JW (2007) The potential importance of saturating and supersaturating contrast response functions in visual cortex. J Vis 7(6):13
Sackett DL (1991) Clinical epidemiology: a basic science for clinical medicine, 2nd edn. Little Brown, Boston, p 441
Fortune B et al (2007) Comparing multifocal VEP and standard automated perimetry in high-risk ocular hypertension and early glaucoma. Investig Ophthalmol Vis Sci 48(3):1173–1180
Balachandran C et al (2006) Comparison of objective diagnostic tests in glaucoma: Heidelberg retinal tomography and multifocal visual evoked potentials. J Glaucoma 15(2):110–116
Ito Y et al (2009) Morphological changes in the visual pathway induced by experimental glaucoma in Japanese monkeys. Exp Eye Res 89(2):246–255
Zhang P et al (2016) Selective reduction of fMRI responses to transient achromatic stimuli in the magnocellular layers of the LGN and the superficial layer of the SC of early glaucoma patients. Hum Brain Mapp 37(2):558–569
Dacey DM, Petersen MR (1992) Dendritic field size and morphology of midget and parasol ganglion cells of the human retina. Proc Natl Acad Sci USA 89(20):9666–9670
Sun H et al (2008) Assessment of contrast gain signature in inferred magnocellular and parvocellular pathways in patients with glaucoma. Vis Res 48(26):2633–2641
Johnson CA (1994) Selective versus nonselective losses in glaucoma. J Glaucoma 3(Suppl 1):S32–S44
Kaplan E, Shapley RM (1986) The primate retina contains two types of ganglion cells, with high and low contrast sensitivity. Proc Natl Acad Sci USA 83(8):2755–2757
Soodak RE, Shapley RM, Kaplan E (1991) Fine structure of receptive-field centers of X and Y cells of the cat. Vis Neurosci 6(6):621–628
Sclar G, Maunsell JH, Lennie P (1990) Coding of image contrast in central visual pathways of the macaque monkey. Vis Res 30(1):1–10
Zemon V et al (1995) Contrast-dependent responses in the human visual system: childhood through adulthood. Int J Neurosci 80(1–4):181–201
Colon EJ, Visser SL (1990) Evoked Potential Manual
Tabachnick BG, Fidell LS (2013) Using multivariate statistics, 6th edn. Pearson Education, Boston, pp 74–76
Mozaffarieh M, Grieshaber MC, Flammer J (2008) Oxygen and blood flow: players in the pathogenesis of glaucoma. Mol Vis 14:224–233
Delaney Y, Walshe TE, O’Brien C (2006) Vasospasm in glaucoma: clinical and laboratory aspects. Optom Vis Sci 83(7):406–414
Mackenzie PJ, Cioffi GA (2008) Vascular anatomy of the optic nerve head. Can J Ophthalmol 43(3):308–312
Agarwal R et al (2009) Current concepts in the pathophysiology of glaucoma. Indian J Ophthalmol 57(4):257–266
Curcio CA, Allen KA (1990) Topography of ganglion cells in human retina. J Comp Neurol 300(1):5–25
Wassle H et al (1990) Retinal ganglion cell density and cortical magnification factor in the primate. Vis Res 30(11):1897–1911
Leung CK et al (2005) Comparison of macular and peripapillary measurements for the detection of glaucoma: an optical coherence tomography study. Ophthalmology 112(3):391–400
Sharma R et al (2015) Visual evoked potentials: normative values and gender differences. J Clin Diagn Res 9(7):CC12–5
Rutjes AW et al (2005) Case–control and two-gate designs in diagnostic accuracy studies. Clin Chem 51(8):1335–1341
Funding
The study is funded by Wenzhou Medical University R&D fund, No. QTJ13009 and Health Innovation Talents in Zhejiang Province (2016). No. 25. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript, with the exception of Zemon who, as a principal in VeriSci Corp., has a financial interest in Huzhou Medconova Medical Technology Co. LTD.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Statement on the welfare of animals
No animals were involved in the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Xu, L.J., Zhang, L., Li, S.L. et al. Accuracy of isolated-check visual evoked potential technique for diagnosing primary open-angle glaucoma. Doc Ophthalmol 135, 107–119 (2017). https://doi.org/10.1007/s10633-017-9598-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-017-9598-6