Abstract
Background
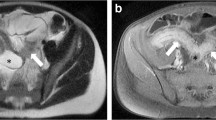
Chronic granulomatous disease (CGD) is a rare primary immunodeficiency which can lead to gastrointestinal (GI) complications including inflammatory bowel disease. Radiographic findings in this cohort have not been well described.
Aims
To describe the frequency and spectrum of gastrointestinal abnormalities seen on computed tomography (CT) in patients with CGD and determine whether radiography was predictive of endoscopic or histopathologic inflammatory findings.
Methods
A retrospective review was conducted on 141 consecutive CGD patients seen at the National Institutes of Health between 1988 and 2011. All corresponding CTs were reviewed for gastrointestinal abnormalities including wall thickening. Endoscopic and histopathologic findings were reviewed in subjects with documented endoscopy within 30 days of an imaging study. Findings were compared between patients with and without wall thickening on CT to determine whether bowel wall thickening was predictive of endoscopic or histologic inflammatory findings.
Results
Two hundred and ninety-two CTs were reviewed. GI wall thickening was present on CT in 61% of patients (n = 86). Among a subgroup of 20 patients who underwent endoscopy at the time of their imaging, there was a statistically significant correlation between radiographic gastrointestinal wall thickening and endoscopic inflammation in the same intestinal segment (p = 0.035). Additionally, there was a significant correlation between radiographic gastrointestinal wall thickening and inflammatory features on histopathology (p = 0.02).
Conclusions
GI abnormalities are commonly observed on CT in CGD patients. Bowel wall thickening correlates with endoscopic and histopathologic evidence of inflammation. These findings may be used to better facilitate directed endoscopic assessment and histopathologic sampling in patients with CGD.




Similar content being viewed by others
References
Winkelstein JA, Marino MC, Johnston RB Jr et al. Chronic granulomatous diseas.e Report on a national registry of 368 patients. Medicine (Baltimore). 2000;79:155–169.
Kuhns DB, Alvord WG, Heller T et al. Residual NADPH oxidase and survival in chronic granulomatous disease. New Engl J Med. 2010;363:2600–2610.
Holland SM. Chronic granulomatous disease. Hematol/Oncol Clin N Am. 2013;27:89–99.
Segal BH, Leto TL, Gallin JI, Malech HL, Holland SM. Genetic, biochemical, and clinical features of chronic granulomatous disease. Medicine (Baltimore). 2000;79:170–200.
Garcia-Eulate R, Hussain N, Heller T et al. CT and MRI of hepatic abscess in patients with chronic granulomatous disease. AJR Am J Roentgenol. 2006;187:482–490.
Towbin AJ, Chaves I. Chronic granulomatous disease. Pediatric Radiol 2010;40:657–668 (quiz 792-3).
Marciano BE, Rosenzweig SD, Kleiner DE et al. Gastrointestinal involvement in chronic granulomatous disease. Pediatrics. 2004;114:462–468.
Marks DJ, Miyagi K, Rahman FZ, Novelli M, Bloom SL, Segal AW. Inflammatory bowel disease in CGD reproduces the clinicopathological features of Crohn’s disease. Am J Gastroenterol. 2009;104:117–124.
Alimchandani M, Lai JP, Aung PP et al. Gastrointestinal histopathology in chronic granulomatous disease: a study of 87 patients. Am J Surg Pathol. 2013;37:1365–1372.
Angelino G, De Angelis P, Faraci S, F et al. Inflammatory bowel disease in chronic granulomatous disease: An emerging problem over a twenty years’ experience. Pediatr Allergy Immunol. 2017;28:801–809.
Kamal N, Marciano B, Curtin B et al. The response to vedolizumab in chronic granulomatous disease-related inflammatory bowel disease. Gastroenterol Rep. 2020;8:404.
Hahn KJ, Ho N, Yockey L et al. Treatment with Anakinra, a recombinant IL-1 receptor antagonist, unlikely to induce lasting remission in patients With CGD colitis. Am J Gastroenterol. 2015;110:938–939.
Uzel G, Orange JS, Poliak N, Marciano BE, Heller T, Holland SM. Complications of tumor necrosis factor-α blockade in chronic granulomatous disease-related colitis. Clin Infect Dis. 2010;51:1429–1434.
Alvarez-Downing MM, Kamal N, Inchauste SM et al. The role of surgery in the management of patients with refractory chronic granulomatous disease colitis. Dis Colon Rectum. 2013;56:609–614.
Marsh RA, Leiding JW, Logan BR et al. Chronic Granulomatous Disease-associated IBD resolves and does not adversely impact survival following allogeneic HCT. J Clin Immunol. 2019;39:653–667.
Feld JJ, Hussain N, Wright EC et al. Hepatic involvement and portal hypertension predict mortality in chronic granulomatous disease. Gastroenterology 2008;134:1917–1926.
Godoy MC, Vos PM, Cooperberg PL, Lydell CP, Phillips P, Müller NL. Chest radiographic and CT manifestations of chronic granulomatous disease in adults. AJR Am J Roentgenol. 2008;191:1570–1575.
Lee M, Lee MS, Lee JS, Ko SY, Jeong SY. Spectrum of imaging findings of chronic granulomatous disease: a single center experience. Diagn Interv Radiolgy (Ankara, Turkey). 2017;23:472–477.
Xia F, Mao J, Ding J, Yang H. Observation of normal appearance and wall thickness of esophagus on CT images. Eur J Radiol 2009;72:406–411.
Karahan OI, Dodd GD 3rd, Chintapalli KN, Rhim H, Chopra S. Gastrointestinal wall thickening in patients with cirrhosis: frequency and patterns at contrast-enhanced CT. Radiology. 2000;215:103–107.
Wiesner W, Mortele KJ, Ji H, Ros PR. Normal colonic wall thickness at CT and its relation to colonic distension. J Comput Assist Tomogr. 2002;26:102–106.
Horton KM, Corl FM, Fishman EK. CT evaluation of the colon: inflammatory disease. Radiographics. 2000;20:399–418.
Macari M, Balthazar EJ. CT of bowel wall thickening: significance and pitfalls of interpretation. AJR Am J Roentgenol. 2001;176:1105–1116.
Laskey HL, Gopal L, Gallin JI, Holland SM, Heller T. Twenty-year follow-up of esophageal involvement in chronic granulomatous disease. Am J Gastroenterol. 2009;104:2368–2370.
Golioto M, O’Connor JB. Esophageal dysmotility in an adult with chronic granulomatous disease. J Clin Gastroenterol 2001;33:330–332.
Khanna G, Kao SC, Kirby P, Sato Y. Imaging of chronic granulomatous disease in children. Radiographics. 2005;25:1183–1195.
Khangura SK, Kamal N, Ho N et al. Gastrointestinal features of chronic granulomatous disease found during endoscopy. Clin Gastroenterol Hepatol. 2016;14:395–402.
Goldblatt D. Recent advances in chronic granulomatous disease. The Journal of infection. 2014;69:S32–S35.
Huang A, Abbasakoor F, Vaizey CJ. Gastrointestinal manifestations of chronic granulomatous disease. Colorectal Dis Off J Assoc Coloproctol G B Irel 2006;8:637–644.
Schappi MG, Klein NJ, Lindley KJ et al. The nature of colitis in chronic granulomatous disease. J Pediatric Gastroenterol Nutr. 2003;36:623–631.
Hong SS, Kim AY, Byun JH et al. MDCT of small-bowel disease: value of 3D imaging. AJR Am J Roentgenol. 2006;187:1212–1221.
Gopal L, Forbes J, Uzel G, Holland SM, Heller T. Gastrointestinal fistulae in chronic granulomatous disease. Am J Gastroenterol. 2009;104:2112–2113.
Macari M, Megibow AJ, Balthazar EJ. A pattern approach to the abnormal small bowel: observations at MDCT and CT enterography. AJR Am J Roentgenol. 2007;188:1344–1355.
Funding
This work was supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Diabetes and Digestive and Kidney Diseases, National Institutes of Health Clinical Center, and the National Institutes of Health Intramural Research Program. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bhattacharya, S., Koethe, Y., Ling, A. et al. Gastrointestinal Computed Tomography Findings in Chronic Granulomatous Disease with Subgroup Clinicopathologic Analysis. Dig Dis Sci 67, 1831–1842 (2022). https://doi.org/10.1007/s10620-021-06978-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-06978-4