Abstract
Background
Many anti-nausea treatments are available for chronic gastrointestinal syndromes, but data on efficacy and comparative effectiveness are sparse.
Aims
To conduct a sectional survey study of patients with chronic nausea to assess comparative effectiveness of commonly used anti-nausea treatments.
Methods
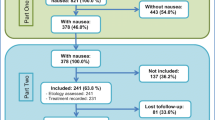
Outpatients at a single center presenting for gastroenterology evaluation were asked to rate anti-nausea efficacy on a scale of 0 (no efficacy) to 5 (very effective) of 29 commonly used anti-nausea treatments and provide other information about their symptoms. Additional information was collected from the patients’ chart. The primary outcome was to determine which treatments were better or worse than average using a t test. The secondary outcome was to assess differential response by individual patient characteristics using multiple linear regression.
Results
One hundred and fifty-three patients completed the survey. The mean efficacy score of all anti-nausea treatments evaluated was 1.73. After adjustment, three treatments had scores statically higher than the mean, including marijuana (2.75, p < 0.0001), ondansetron (2.64, p < 0.0001), and promethazine (2.46, p < 0.0001). Several treatments, including many neuromodulators, complementary and alternative treatments, erythromycin, and diphenhydramine had scores statistically below average. Patients with more severe nausea responded better to marijuana (p = 0.036) and diphenhydramine (p < 0.001) and less so to metoclopramide (p = 0.020). There was otherwise no significant differential response by age, gender, nausea localization, underlying gastrointestinal cause of nausea, and GCSI.
Conclusions
When treating nausea in patients with chronic gastrointestinal syndromes, clinicians may consider trying higher performing treatments first, and forgoing lower performing treatments. Further prospective research is needed, particularly with respect to highly effective treatments.



Similar content being viewed by others
References
Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the united states: update 2018. Gastroenterology. 2019;156:e211.
Singh P, Yoon SS, Kuo B. Nausea: a review of pathophysiology and therapeutics. Therap Adv Gastroenterol. 2016;9:98–112.
American Gastroenterological A. American Gastroenterological Association medical position statement: nausea and vomiting. Gastroenterology. 2001;120:261–263.
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. American College of G. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108:18–37. (quiz 38).
Saad RJ. The wireless motility capsule: a one-stop shop for the evaluation of GI motility disorders. Curr Gastroenterol Rep. 2016;18:14.
Solnes LB, Sheikhbahaei S, Ziessman HA. Nuclear scintigraphy in practice: gastrointestinal motility. AJR Am J Roentgenol. 2018;211:260–266.
Shankar A, Roy S, Malik A, Julka PK, Rath GK. Prevention of chemotherapy-induced nausea and vomiting in cancer patients. Asian Pac J Cancer Prev. 2015;16:6207–6213.
Yu D, Ramsey FV, Norton WF, et al. The burdens, concerns, and quality of life of patients with gastroparesis. Dig Dis Sci. 2017;62:879–893. https://doi.org/10.1007/s10620-017-4456-7.
Tricco AC, Blondal E, Veroniki AA, et al. Comparative safety and effectiveness of serotonin receptor antagonists in patients undergoing chemotherapy: a systematic review and network meta-analysis. BMC Med. 2016;14:216.
Christofaki M, Papaioannou A. Ondansetron: a review of pharmacokinetics and clinical experience in postoperative nausea and vomiting. Expert Opin Drug Metab Toxicol. 2014;10:437–444.
Deitrick CL, Mick DJ, Lauffer V, Prostka E, Nowak D, Ingersoll G. A comparison of two differing doses of promethazine for the treatment of postoperative nausea and vomiting. J Perianesth Nurs. 2015;30:5–13.
Furyk JS, Meek RA, Egerton-Warburton D. Drugs for the treatment of nausea and vomiting in adults in the emergency department setting. Cochrane Database Syst Rev. 2015;CD010106.
Allen JH, de Moore GM, Heddle R, Twartz JC. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut. 2004;53:1566–1570.
Tornblom H, Drossman DA. Psychotropics, antidepressants, and visceral analgesics in functional gastrointestinal disorders. Curr Gastroenterol Rep. 2018;20:58.
Parkman HP, Van Natta ML, Abell TL, et al. Effect of nortriptyline on symptoms of idiopathic gastroparesis: the NORIG randomized clinical trial. JAMA. 2013;310:2640–2649.
Janssens J, Peeters TL, Vantrappen G, et al. Improvement of gastric emptying in diabetic gastroparesis by erythromycin. Preliminary studies. N Engl J Med. 1990;322:1028–1031.
Richards RD, Davenport K, McCallum RW. The treatment of idiopathic and diabetic gastroparesis with acute intravenous and chronic oral erythromycin. Am J Gastroenterol. 1993;88:203–207.
Acosta A, Camilleri M. Prokinetics in gastroparesis. Gastroenterol Clin North Am. 2015;44:97–111.
Snape WJ Jr, Battle WM, Schwartz SS, Braunstein SN, Goldstein HA, Alavi A. Metoclopramide to treat gastroparesis due to diabetes mellitus: a double-blind, controlled trial. Ann Intern Med. 1982;96:444–446.
Perkel MS, Moore C, Hersh T, Davidson ED. Metoclopramide therapy in patients with delayed gastric emptying: a randomized, double-blind study. Dig Dis Sci. 1979;24:662–666. https://doi.org/10.1007/BF01314461.
McCallum RW, Ricci DA, Rakatansky H, et al. A multicenter placebo-controlled clinical trial of oral metoclopramide in diabetic gastroparesis. Diabetes Care. 1983;6:463–467.
Ricci DA, Saltzman MB, Meyer C, Callachan C, McCallum RW. Effect of metoclopramide in diabetic gastroparesis. J Clin Gastroenterol. 1985;7:25–32.
Patterson D, Abell T, Rothstein R, Koch K, Barnett J. A double-blind multicenter comparison of domperidone and metoclopramide in the treatment of diabetic patients with symptoms of gastroparesis. Am J Gastroenterol. 1999;94:1230–1234.
Rao AS, Camilleri M. Review article: metoclopramide and tardive dyskinesia. Aliment Pharmacol Ther. 2010;31:11–19.
Funding
The study was not funded.
Author information
Authors and Affiliations
Contributions
TAZ, JOC contributed to study concept and design, data acquisition, data/statistical analysis, drafting manuscript, revision of manuscript, and study supervision. LN, AK, NF-B, KR, MN, IS, MG, PO, LN, DG, PG, and GT helped in data acquisition, drafting manuscript, and revision of manuscript
Corresponding author
Ethics declarations
Conflict of interest
Nothing to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10620_2020_6195_MOESM1_ESM.pdf
Figure S1: Survey. Paper copies of this survey were distributed to eligible patients by clinical staff or physicians 1 (PDF 304 kb)
Rights and permissions
About this article
Cite this article
Zikos, T.A., Nguyen, L., Kamal, A. et al. Marijuana, Ondansetron, and Promethazine Are Perceived as Most Effective Treatments for Gastrointestinal Nausea. Dig Dis Sci 65, 3280–3286 (2020). https://doi.org/10.1007/s10620-020-06195-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06195-5