Abstract
Background
The epidemiology of upper gastrointestinal (L4) Crohn’s disease in China remains poorly characterized.
Aims
We aimed to identify the clinical characteristics of L4 disease and clarify the relationship between disease characteristics at diagnosis and early outcomes.
Methods
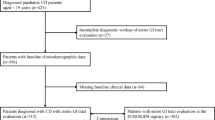
We retrospectively enrolled 246 patients diagnosed between 2013 and 2017 and followed up for > 1 year post-diagnosis. Primary outcomes included the 1-year rates of hospitalization and abdominal surgery according to disease location and behavior.
Results
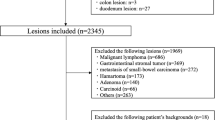
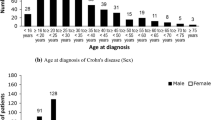
Of 80 patients with L4 disease (61, 25, and 18 with esophagogastroduodenal, jejunal, and proximal ileal involvement, respectively), none had granuloma, whereas 66.7%, 50%, 46.9%, 75%, and 70% had disease-specific endoscopic lesions in the esophagus, stomach, duodenum, jejunum, and proximal ileum, respectively. Compared to non-L4 disease, L4 disease was associated with higher rates of abdominal surgery (41.3% vs. 11.4%, P < 0.001) but similar rates of hospitalization within 1 year post-diagnosis. In L4 disease, jejunal and proximal ileal involvement was associated with stricturing behavior (P = 0.034, P < 0.001) and higher abdominal surgery rate (both: P < 0.001). Risk factors for abdominal surgery within 1 year post-diagnosis included age ≥ 40 years (OR 1.920; 95% CI 1.095–3.367), L4 phenotype (OR 6.335; 95% CI 3.862–10.390), stricturing disease (OR 3.162; 95% CI 1.103–9.866), and penetrating disease (OR 11.504; 95% CI 3.409–38.825), whereas the protective factor was female sex (OR 0.214; 95% CI 0.123–0.373).
Conclusions
Early outcomes are worse for L4 than for non-L4 disease. Jejunoileum involvement predicts stricturing disease and early surgery. More aggressive initial therapy is needed to improve L4-disease prognosis.


Similar content being viewed by others
References
Satsangi J. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749–753.
Chow DK, Sung JJ, Wu JC, Tsoi KK, Leong RW, Chan FK. Upper gastrointestinal tract phenotype of Crohn’s disease is associated with early surgery and further hospitalization. Inflamm Bowel Dis. 2009;15:551–557.
Wolters FL, Russel MG, Sijbrandij J, et al. Phenotype at diagnosis predicts recurrence rates in Crohn’s disease. Gut. 2006;55:1124–1130.
Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg. 2000;231:38–45.
Lazarev M, Huang C, Bitton A, et al. Relationship between proximal Crohn’s disease location and disease behavior and surgery: a cross-sectional study of the IBD Genetics Consortium. Am J Gastroenterol. 2013;108:106–112.
Park SK, Yang SK, Park SH, et al. Long-term prognosis of the jejunal involvement of Crohn’s disease. J Clin Gastroenterol. 2013;47:400–408.
Kim OZ, Han DS, Park CH, et al. The clinical characteristics and prognosis of Crohn’s disease in Korean patients showing proximal small bowel involvement: results from the CONNECT study. Gut Liver. 2018;12:67–72.
Mao R, Tang RH, Qiu Y, et al. Different clinical outcomes in Crohn’s disease patients with esophagogastroduodenal, jejunal, and proximal ileal disease involvement: is L4 truly a single phenotype? Therap Adv Gastroenterol. 2018;11:1756284818777938.
Dassopoulos T, Sultan S, Falck-Ytter YT, Inadomi JM, Hanauer SB. American Gastroenterological Association Institute technical review on the use of thiopurines, methotrexate, and anti-TNF-α biologic drugs for the induction and maintenance of remission in inflammatory Crohn’s disease. Gastroenterology. 2013;145:1464.e5–1478.e5.
Yang RP, Gao X, Chen MH, Xiao YL, Chen BL. Hu PJ [Risk factors for initial bowel resection and postoperative recurrence in patients with Crohn disease]. Zhonghua Wei Chang Wai Ke Za Zhi. 2011;14:176–180.
Louis E, Collard A, Oger A, Degroote E, El Yafi FAN, Belaiche J. Behaviour of Crohn’s disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777–782.
Binder V, Hendriksen C, Kreiner S. Prognosis in Crohn’s disease—based on results from a regional patient group from the county of Copenhagen. Gut. 1985;26:146–150.
Song X, Gao X, Li M, et al. Clinical features and risk factors for primary surgery in 205 patients with Crohnʼs disease: analysis of a South China cohort. Dis Colon Rectum. 2011;54:1147–1154.
Sakuraba A, Iwao Y, Matsuoka K, et al. Endoscopic and pathologic changes of the upper gastrointestinal tract in Crohn’s disease. BioMed Res Int. 2014;2014:610767.
Park JH, Nam HN, Lee J, et al. Characteristics of upper gastrointestinal tract involvement in Korean pediatric Crohn’s disease: a multicenter study. Pediatr Gastroenterol Hepatol Nutr. 2017;20:227–235.
Annunziata ML, Caviglia R, Papparella LG, Cicala M. Upper gastrointestinal involvement of Crohn’s disease: a prospective study on the role of upper endoscopy in the diagnostic work-up. Dig Dis Sci. 2012;57:1618–1623. https://doi.org/10.1007/s10620-012-2072-0.
Nugent FW, Roy MA. Duodenal Crohn’s disease: an analysis of 89 cases. Am J Gastroenterol. 1989;84:249–254.
Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 1: diagnosis and medical management. J Crohns Colitis. 2016;11:3–25.
Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV. Risk factors associated with progression to intestinal complications of Crohn’s disease in a population-based cohort. Gastroenterology. 2010;139:1147–1155.
Nguyen GC, Torres EA, Regueiro M, et al. Inflammatory bowel disease characteristics among African Americans, Hispanics, and non-Hispanic whites: characterization of a large North American cohort. Am J Gastroenterol. 2006;101:1012–1023.
Leong RW, Lau JY, Sung JJ. The epidemiology and phenotype of Crohn’s disease in the Chinese population. Inflamm Bowel Dis. 2004;10:646–651.
Yokota K, Saito Y, Einami K, et al. A bamboo joint-like appearance of the gastric body and cardia: possible association with Crohn’s disease. Gastrointest Endosc. 1997;46:268–272.
Rutgeerts P, Onette E, Vantrappen G, Geboes K, Broeckaert L, Talloen L. Crohn’s disease of the stomach and duodenum: a clinical study with emphasis on the value of endoscopy and endoscopic biopsies. Endoscopy. 1980;12:288–294.
Cameron DJ. Upper and lower gastrointestinal endoscopy in children and adolescents with Crohn’s disease: a prospective study. J Gastroenterol Hepatol. 1991;6:355–358.
Carbo AI, Reddy T, Gates T, Vesa T, Thomas J, Gonzalez E. The most characteristic lesions and radiologic signs of Crohn disease of the small bowel: air enteroclysis, MDCT, endoscopy, and pathology. Abdom Imaging. 2014;39:215–234.
Alcantara M, Rodriguez R, Potenciano JL, Carrobles JL, Munoz C, Gomez R. Endoscopic and bioptic findings in the upper gastrointestinal tract in patients with Crohn’s disease. Endoscopy. 1993;25:282–286.
Wright CL, Riddell RH. Histology of the stomach and duodenum in Crohn’s disease. Am J Surg Pathol.. 1998;22:383–390.
Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sandborn WJ, Loftus EJ. Surgery in a population-based cohort of Crohn’s disease from Olmsted County, Minnesota (1970–2004). Am J Gastroenterol. 2012;107:1693–1701.
Sampietro GM, Corsi F, Maconi G, et al. Prospective study of long-term results and prognostic factors after conservative surgery for small bowel Crohn’s disease. Clin Gastroenterol Hepatol. 2009;7:183–191.
Henriksen M, Jahnsen J, Lygren I, et al. Clinical course in Crohn’s disease: results of a five-year population-based follow-up study (the IBSEN study). Scand J Gastroenterol. 2007;42:602–610.
Chang C, Wong J, Tung C, Shih I, Wang H, Wei S. Intestinal stricture in Crohn’s disease. Intest Res. 2015;13:19–26.
Yamamoto T, Allan RN, Keighley MR. An audit of gastroduodenal Crohn disease: clinicopathologic features and management. Scand J Gastroenterol. 1999;34:1019–1024.
Levine A, Griffiths A, Markowitz J, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:1314–1321.
Hoekman DR, Stibbe JA, Baert FJ, et al. Long-term outcome of early combined immunosuppression versus conventional management in newly diagnosed Crohn’s disease. J Crohns Colitis. 2018;12:517–524.
Korelitz BI, Waye JD, Kreuning J, et al. Crohn’s disease in endoscopic biopsies of the gastric antrum and duodenum. Am J Gastroenterol. 1981;76:103–109.
El-Omar E, Penman I, Cruikshank G, et al. Low prevalence of Helicobacter pylori in inflammatory bowel disease: association with sulphasalazine. Gut. 1994;35:1385–1388.
Acknowledgments
The authors would like to thank the patients and staff of the Jinling Hospital for their support with screening and data collection.
Author information
Authors and Affiliations
Contributions
X-WS, JW, and F-YW are the guarantors of the article, having initiated and designed the study; X-WS, X-XJ, H-JW, and B-SY collected the data; X-WS and ZY performed the data analysis; X-WS and JW drafted the manuscript; M-FY, JL, and F-YW critically revised the manuscript; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, XW., Wei, J., Yang, Z. et al. Clinical Features and Prognosis of Crohn’s Disease with Upper Gastrointestinal Tract Phenotype in Chinese Patients. Dig Dis Sci 64, 3291–3299 (2019). https://doi.org/10.1007/s10620-019-05651-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05651-1