Abstract
Background
Location of bleeding can present a diagnostic challenge in patients without hematemesis more so than those with hematemesis.
Aim
To describe endoscopic diagnostic yields in both hematemesis and non-hematemesis gastrointestinal bleeding patient populations.
Methods
A retrospective analysis on a cohort of 343 consecutively identified gastrointestinal bleeding patients admitted to a tertiary care center emergency department with hematemesis and non-hematemesis over a 12-month period. Data obtained included presenting symptoms, diagnostic lesions, procedure types with diagnostic yields, and hours to diagnosis.
Results
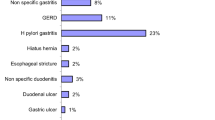
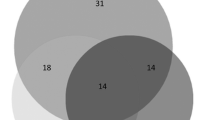
The hematemesis group (n = 105) took on average 15.6 h to reach a diagnosis versus 30.0 h in the non-hematemesis group (n = 231), (p = 0.005). In the non-hematemesis group, the first procedure was diagnostic only 53% of the time versus 71% in the hematemesis group (p = 0.02). 25% of patients in the non-hematemesis group required multiple procedures versus 10% in the hematemesis group (p = 0.004). Diagnostic yield for a primary esophagogastroduodenoscopy was 71% for the hematemesis group versus 50% for the non-hematemesis group (p = 0.01). Primary colonoscopies were diagnostic in 54% of patients and 12.5% as a secondary procedure in the non-hematemesis group. A primary video capsule endoscopy yielded a diagnosis in 79% of non-hematemesis patients (n = 14) and had a 70% overall diagnostic rate (n = 33).
Conclusion
Non-hematemesis gastrointestinal bleeding patients undergo multiple non-diagnostic tests and have longer times to diagnosis and then compared those with hematemesis. The high yield of video capsule endoscopy in the non-hematemesis group suggests a role for this device in this context and warrants further investigation.


Similar content being viewed by others
References
Eisen GM, Dominitz JA, Faigel DO, et al. An annotated algorithmic approach to upper gastrointestinal bleeding. Am J Gastroenterol. 2001;53:853–858. https://doi.org/10.1016/s0016-5107(01)70305-7.
Brackman MR, Gushchin VV, Smith L, et al. Acute lower gastroenteric bleeding retrospective analysis (the ALGEBRA study): an analysis of the triage, management and outcomes of patients with acute lower gastrointestinal bleeding. Am Surg. 2003;69:145–149.
Rockall TA, Logan RF, Devlin HB, et al. Risk assessment after acute upper gastrointestinal hemorrhage. Gut. 1996;38:316–321. https://doi.org/10.1136/gut.38.3.316.
Blatchford O, Murray WR, Blatchford MA. A risk score to predict need for upper-gastrointestinal hemorrhage. Lancet. 2000;356:1318–1321. https://doi.org/10.1016/S0140-6736(00)02816-6%5d.
Church NI, Dallal NJ, Masson J. Validity of the Rockall system after endoscopic therapy for bleeding peptic ulcer: a prospective cohort study. Gastrointest Endosc. 2006;63:606–612. https://doi.org/10.1016/j.gie.2005.06.042.
Das A, Wong RC. Prediction of outcome of acute GI hemorrhage review of risk scores and predictive models. Gastrointest Endosc. 2004;60:85–93. https://doi.org/10.1016/S0016-5107(04)01291-X.
Cappell MS, Friedel D. Initial management of acute upper gastrointestinal bleeding: from initial evaluation up to gastrointestinal endoscopy. Med Clin North Am. 2008;92:491. https://doi.org/10.1016/j.mcna.2008.01.005.
Srygley FD, Gerardo CJ, Tran T, Fisher DA. Does this patient have a severe upper gastrointestinal bleed? JAMA. 2012;307:1072–1079. https://doi.org/10.1001/jama.2012.253.
Peter DJ, Doughtery JM. Evaluation of the patient with gastrointestinal bleeding: an evidence based approach. Emerg Med Clin North Am. 1999;17:239–261. https://doi.org/10.1016/S0733-8627(05)70055-9.
Witting MD, Magder L, Heins AE, Mattu A, Granja CA, Baumgarten M. ED predictors of upper gastrointestinal tract bleeding in patients without hematemesis. Am J Emerg Med. 2006;24:280–285. https://doi.org/10.1016/j.ajem.2005.11.005.
Peura DA, Lanza FL, Gostout CJ, et al. The American College of Gastroenterology Bleeding Registry: preliminary findings. Am J Gastroenterol. 1997;92:924–928.
Ibach MB, Grier JF, Goldman DE, LaFontaine S, Gholson CF. Diagnostic considerations in evaluation of patients presenting with melena and nondiagnostic esophagogastroduodenoscopy. Dig Dis Sci. 1995;40:1459–1462. https://doi.org/10.1007/BF02285192.
Zuccaro G. Management of the adult patient with acute lower gastrointestinal bleeding. Am J Gastroenterol. 1998;93:1202–1208. https://doi.org/10.1016/S0002-9270(98)00276-7.
Chalasani N, Clark WS, Wilcox CM. Blood urea nitrogen to creatinine concentration in gastrointestinal bleeding: a reappraisal. Am J Gastroenterol. 1997;92:1796–1799.
Gunjan D, Sharma V, Rana SS, Bhasin DK. Small bowel bleeding: a comprehensive review. Gastroenterol Rep. 2014;2(4):262–275.
Gersen LB, Fidler JF, Cave DR, Leighton JA. Diagnosis and management of small bowel bleeding. Am J Gastroenterol. 2015;110:1265–1287. https://doi.org/10.1038/ajg.2015.246.
Silverstein FE, Gilbert DA, Tedesco FJ, Buenger NK, Persing J. The national ASGE survey on upper gastrointestinal bleeding. II. Clinical prognostic factors. Gastrointest Endosc. 1981;27:80–93.
Laine L, Peterson WL. Bleeding peptic ulcer. N Engl J Med. 1994;331:717–727. https://doi.org/10.1056/NEJM199409153311107.
Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1995;90:206–210.
Boonpongmanee S, Fleischer D, Pezzullo J, et al. The frequency of peptic ulcer as a cause of upper-GI bleeding is exaggerated. Gastrointest Endosc. 2004;59:788–794. https://doi.org/10.1016/S0016-5107(04)00181-6.
Enestvedt BK, Gralnek IM, Mattek N, Lieberman DA, Eisen G. An evaluation of endoscopic indications and findings related to nonvariceal upper-GI hemorrhage in a large multicenter consortium. Gastrointest Endosc. 2008;67:422. https://doi.org/10.1016/j.gie.2007.09.024.
Loperfido S, Baldo V, Piovesana E, et al. Changing trends in acute upper-GI bleeding: a population-based study. Gastrointest Endosc. 2009;70:212. https://doi.org/10.1016/j.gie.2008.10.051.
Etzel JP, Williams JL, Jiang Z, Lieberman DA, Knigge K, Faigel DO. Diagnostic yield of colonoscopy to evaluate melena after a nondiagnostic EGD. Gastrointest Endosc. 2012;75:819–826. https://doi.org/10.1016/j.gie.2011.11.041.
Angtuaco T, Reddy S, Drapkin S, et al. The utility of urgent colonoscopy in the evaluation of acute lower gastrointestinal tract bleeding: a 2-year experience from a single center. Am J Gastroenterol. 2001;96:1782–1785. https://doi.org/10.1111/j.1572-0241.2001.03871.x.
Jensen DM, Machicado GA. Diagnosis and treatment of severe hematochezia. The role of urgent colonoscopy after purge. Gastroenterology. 1988;95:1569–1574.
Laine L, Shah A. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding. Am J Gastroenterol. 2010;105:2636–2641. https://doi.org/10.1038/ajg.2010.277.
Sung JY, Tang RS, Ching JY, et al. Use of capsule endoscopy in the emergency department as a triage of patients with GI bleeding. Gastrointest Endosc. 2016;84:907–913.
Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010;71:280. https://doi.org/10.1016/j.gie.2009.09.031.
Lewis BS, Swain P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: results of a pilot study. Gastrointest Endosc. 2002;56:349. https://doi.org/10.1067/mge.2002.126906.
Scapa E, Jacob H, Lewkowicz S, et al. Initial experience of wireless-capsule endoscopy for evaluating occult gastrointestinal bleeding and suspected small bowel pathology. Am J Gastroenterol. 2002;97:2776. https://doi.org/10.1111/j.1572-0241.2002.07021.x.
Kitiyakara Taya, Selby Warwick. Non-small-bowel lesions detected by capsule endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;62:234–238. https://doi.org/10.1016/S0016-5107(05)00292-0.
Galmiche JP, Coron E, Sacher-Huvelin S. Recent developments in capsule endoscopy. Gut. 2008;57:695–703. https://doi.org/10.1136/gut.2007.127852.
Sidhu R, Sanders DS, McAlindon ME. Does capsule endoscopy recognise gastric antral vascular ectasia more frequently than conventional endoscopy? J Gastrointest Liver Dis. 2006;15:375–377.
Rubin M, Hussain SA, Shalomov A, Cortes RA, Smith MS, Kim SH. Live view video capsule endoscopy enables risk stratification of patients with acute upper GI Bleeding in the emergency room: a pilot study. Dig Dis Sci. 2011;56:786–791. https://doi.org/10.1007/s10620-010-1336-9.
Meltzer AC, Ali MA, Kresiberg RB, et al. Video capsule endoscopy in the emergency department: a prospective study of acute upper gastrointestinal hemorrhage. Ann Emerg Med. 2013;61:438–443. https://doi.org/10.1016/j.annemergmed.2012.11.008.
Gralnek IM, Ching JY, Maza I, et al. Capsule endoscopy in acute upper gastrointestinal hemorrhage: a prospective cohort study. Endoscopy. 2013;45:12–19. https://doi.org/10.1055/s-0032-1325933.
Gayer C, Chino A, Lucas C, et al. Acute lower gastrointestinal bleeding in 1112 patients admitted to an urban emergency medical center. Surgery. 2009;146:600–606. https://doi.org/10.1016/j.surg.2009.06.055.
Singh A, Marshall C, Chaudhuri B, et al. Timing of video capsule endoscopy relative to overt obscure GI bleeding: implications from a retrospective study. Gastrointest Endosc. 2013;77:640–761. https://doi.org/10.1016/j.gie.2012.11.041.
Hay JA, Lyubashevsky E, Elashoff J, Maldonado L, Weingarten SR, Ellrodt AG. Upper gastrointestinal hemorrhage clinical guideline—determining the optimal hospital length of stay. Am J Med. 1996;100:313–322. https://doi.org/10.1016/S0002-9343(97)89490-9.
Author information
Authors and Affiliations
Contributions
SJ was involved in study concept and design, acquisition of data, analysis and interpretation of data, drafting of manuscript, and statistical analysis. NM contributed to study concept and design, acquisition of data, analysis and interpretation of data, and drafting of manuscript. BG performed acquisition of data, study concept and design. LM was involved in study concept and design, data analysis and interpretation, and statistical analysis. CM, AS, GV, DC contributed to study concept and design, critical revision of the manuscript for important intellectual content. JC performed study concept and design. MA-S analyzed data. AF performed administrative and drafting of manuscript. The study was reviewed and approved by the University of Massachusetts Medical School Institutional Review Board. A HIPPA waiver was approved by the aforementioned IRB given minimal risk to patient subjects.
Corresponding author
Ethics declarations
Conflict of interest
Dr David Cave is a consultant for Olympus USA and Tokyo; he is also a contributor to UptoDate.
Additional information
Core Tip: This study is one of the first to follow the diagnostic course of consecutive patients presenting to the emergency department with GIB. Diagnosing bleeding lesions in patients presenting with hematemesis was found to be efficient with quick diagnostic times. However, those presenting with non-hematemesis bleeding have less efficient evaluations, often needing multiple non-diagnostic procedures with longer times to diagnosis.
Rights and permissions
About this article
Cite this article
Jawaid, S., Marya, N., Gondal, B. et al. Lower Endoscopic Diagnostic Yields Observed in Non-hematemesis Gastrointestinal Bleeding Patients. Dig Dis Sci 63, 3448–3456 (2018). https://doi.org/10.1007/s10620-018-5244-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5244-8