Abstract
Background and Aims
The aim of the study was to evaluate the safety of non-anesthesia provider (NAAP)-administered propofol sedation for advanced endoscopic procedures with those of anesthesia provider (AAP).
Methods
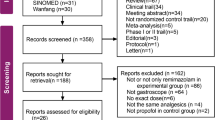
PubMed, EMBASE, Cochrane Central Register of Controlled Trials, Scopus, and Web of Science databases were searched for prospective observational trials involving advanced endoscopic procedures. From a total of 519 publications, 26 were identified to meet inclusion criteria (10 AAPs and 16 NAAPs) and were analyzed. Data were analyzed for hypoxia rate, airway intervention rates, endoscopist, and patient satisfaction scores and total propofol administered.
Results
Total number of procedures in NAAP and AAP groups was 3018 and 2374, respectively. Pooled hypoxia (oxygen saturation less than 90 %) rates were 0.133 (95 % CI 0.117–0.152) and 0.143 (95 % CI 0.128–0.159) in NAAP and AAP, respectively. Similarly, pooled airway intervention rates were 0.035 (95 % CI 0.026–0.047) and 0.133 (95 % CI 0.118–0.150), respectively. Pooled patient satisfaction rate, pooled endoscopist satisfaction rate, and mean propofol administered dose for NAAP were 7.22 (95 % CI 7.17–7.27), 6.03 (95 % CI 5.94–6.11), and 251.44 mg (95 % CI 244.39–258.49) in that order compared with 9.82 (95 % CI 9.76–9.88), 9.06 (95 % CI 8.91–9.21), and 340.32 mg (95 % CI 327.30–353.33) for AAP.
Conclusions
The safety of NAAP sedation compared favorably with AAP sedation in patients undergoing advanced endoscopic procedures. However, it came at the cost of decreased patient and endoscopist satisfaction.











Similar content being viewed by others
References
Sethi S, Wadhwa V, Thaker A, et al. Propofol versus traditional sedative agents for advanced endoscopic procedures: a meta-analysis. Dig Endosc. 2014;26:515–524.
Dumonceau J-M. Nonanesthesiologist administration of propofol: it’s all about money. Endoscopy. 2012;44:453–455.
Goudra BG, Singh PM. SEDASYS, sedation, and the unknown. J Clin Anesth. 2014;26:334–336.
Goudra BG, Singh PM, Chandrasekhara V. SEDASYS®, airway, oxygenation, and ventilation: anticipating and managing the challenges. Dig Dis Sci. 2014;59:920–927.
Clarification of the interpretative guidelines for the anaesthesia services condition of participation and revised hospital anaesthesia guidelines-state operations manual (SOM) Appendix A, S&C-10-09-Hospital. CMS publication no. 100-07.
Rex DK, Overley C, Kinser K, et al. Safety of propofol administered by registered nurses with gastroenterologist supervision in 2000 endoscopic cases. Am J Gastroenterol. 2002;97:1159–1163.
Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C. Safety of propofol for conscious sedation during endoscopic procedures in high-risk patients-a prospective, controlled study. Am J Gastroenterol. 2003;98:1751–1757.
Külling D, Rothenbühler R, Inauen W. Safety of nonanesthetist sedation with propofol for outpatient colonoscopy and esophagogastroduodenoscopy. Endoscopy. 2003;35:679–682.
Sieg A, bng-Study-Group, Beck S, et al. Safety analysis of endoscopist-directed propofol sedation: a prospective, national multicenter study of 24 441 patients in German outpatient practices. J Gastroenterol Hepatol. 2014;29:517–523.
Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C. Risk stratification and safe administration of propofol by registered nurses supervised by the gastroenterologist: a prospective observational study of more than 2000 cases. Gastrointest Endosc. 2003;57:664–671.
Sieg A. Propofol sedation in outpatient colonoscopy by trained practice nurses supervised by the gastroenterologist: a prospective evaluation of over 3000 cases. Z Gastroenterol. 2007;45:697–701.
Rex DK, Deenadayalu VP, Eid E, Imperiale TF, Walker JA, Sandhu K, et al. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009;137:1229–1237; quiz 1518–1519.
Chen SC, Rex DK. Review article: registered nurse-administered propofol sedation for endoscopy. Aliment Pharmacol Ther. 2004;19:147–155.
Rex DK. Endoscopist-directed propofol. Tech Gastrointest Endosc. 2009;11:177–180.
Cohen LB, Dubovsky AN, Aisenberg J, Miller KM. Propofol for endoscopic sedation: a protocol for safe and effective administration by the gastroenterologist. Gastrointest Endosc. 2003;58:725–732.
Vargo JJ, Cohen LB, Rex DK, Kwo PY. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc. 2009;70:1053–1059.
Poincloux L, Laquière A, Bazin J-E, et al. A randomized controlled trial of endoscopist vs. anaesthetist-administered sedation for colonoscopy. Dig Liver Dis. 2011;43:553–558.
Paspatis G, Chainaki I, Manolaraki M, et al. Efficacy of bispectral index monitoring as an adjunct to propofol deep sedation for ERCP: a randomized controlled trial. Endoscopy. 2009;41:1046–1051.
Paspatis GA, Manolaraki MM, Vardas E, Theodoropoulou A, Chlouverakis G. Deep sedation for endoscopic retrograde cholangiopancreatography: intravenous propofol alone versus intravenous propofol with oral midazolam premedication. Endoscopy. 2008;40:308–313.
Coté GA, Hovis RM, Ansstas MA, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol.. 2010;8:137–142.
Fanti L, Agostoni M, Arcidiacono PG, et al. Target-controlled infusion during monitored anesthesia care in patients undergoing EUS: propofol alone versus midazolam plus propofol. A prospective double-blind randomised controlled trial. Dig Liver Dis. 2007;39:81–86.
Mazanikov M, Udd M, Kylänpää L, et al. Patient-controlled sedation for ERCP: a randomized double-blind comparison of alfentanil and remifentanil. Endoscopy. 2012;44:487–492.
Mazanikov M, Udd M, Kylänpää L, et al. A randomized comparison of target-controlled propofol infusion and patient-controlled sedation during ERCP. Endoscopy. 2013;45:915–919.
Kongkam P, Rerknimitr R, Punyathavorn S, et al. Propofol infusion versus intermittent meperidine and midazolam injection for conscious sedation in ERCP. J Gastrointest Liver Dis. 2008;17:291–297.
Barnett SR, Berzin T, Sanaka S, Pleskow D, Sawhney M, Chuttani R. Deep sedation without intubation for ERCP is appropriate in healthier, non-obese patients. Dig Dis Sci. 2013;58:3287–3292.
Berzin TM, Sanaka S, Barnett SR, et al. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73:710–717.
Mazanikov M, Udd M, Kylänpää L, et al. Patient-controlled sedation with propofol and remifentanil for ERCP: a randomized, controlled study. Gastrointest Endosc. 2011;73:260–266.
Redondo-Cerezo E, Sánchez-Robaina A, Martínez Cara JG, et al. Gastroenterologist-guided sedation with propofol for endoscopic ultrasonography in average-risk and high-risk patients: a prospective series. Eur J Gastroenterol Hepatol. 2012;24:506–512.
Lee CK, Lee S-H, Chung I-K, et al. Balanced propofol sedation for therapeutic GI endoscopic procedures: a prospective, randomized study. Gastrointest Endosc. 2011;73:206–214.
Von Delius S, Salletmaier H, Meining A, et al. Bispectral index monitoring of midazolam and propofol sedation during endoscopic retrograde cholangiopancreatography: a randomized clinical trial (the EndoBIS study). Endoscopy. 2012;44:258–264.
Lee TH, Lee CK, Park S-H, et al. Balanced propofol sedation versus propofol monosedation in therapeutic pancreaticobiliary endoscopic procedures. Dig Dis Sci. 2012;57:2113–2121.
Khan HA, Umar M, Tul-Bushra H, Nisar G, Bilal M, Umar S. Safety of non-anaesthesiologist-administered propofol sedation in ERCP. Arab J Gastroenterol. 2014;15:32–35.
Riphaus A, Geist C, Schrader K, Martchenko K, Wehrmann T. Intermittent manually controlled versus continuous infusion of propofol for deep sedation during interventional endoscopy: a prospective randomized trial. Scand J Gastroenterol. 2012;47:1078–1085.
Dewitt J, McGreevy K, Sherman S, Imperiale TF. Nurse-administered propofol sedation compared with midazolam and meperidine for EUS: a prospective, randomized trial. Gastrointest Endosc. 2008;68:499–509.
Angsuwatcharakon P, Rerknimitr R, Ridtitid W, et al. Cocktail sedation containing propofol versus conventional sedation for ERCP: a prospective, randomized controlled study. BMC Anesthesiol. 2012;12:20.
García-Suárez C, López-Rosés L, Olivencia P, et al. Sedation with propofol controlled by endoscopists during percutaneous endoscopic gastrostomy. Rev Esp Enferm Dig. 2010;102:249–256.
Wehrmann T, Grotkamp J, Stergiou N, et al. Electroencephalogram monitoring facilitates sedation with propofol for routine ERCP: a randomized, controlled trial. Gastrointest Endosc. 2002;56:817–824.
Yusoff IF, Raymond G, Sahai AV. Endoscopist administered propofol for upper-GI EUS is safe and effective: a prospective study in 500 patients. Gastrointest Endosc. 2004;60:356–360.
Fatima H, DeWitt J, LeBlanc J, Sherman S, McGreevy K, Imperiale TF. Nurse-administered propofol sedation for upper endoscopic ultrasonography. Am J Gastroenterol. 2008;103:1649–1656.
Vargo JJ, Zuccaro G, Dumot JA, et al. Gastroenterologist-administered propofol versus meperidine and midazolam for advanced upper endoscopy: a prospective, randomized trial. Gastroenterology. 2002;123:8–16.
Riphaus A, Stergiou N, Wehrmann T. Sedation with propofol for routine ERCP in high-risk octogenarians: a randomized, controlled study. Am J Gastroenterol. 2005;100:1957–1963.
Schilling D, Rosenbaum A, Schweizer S, Richter H, Rumstadt B. Sedation with propofol for interventional endoscopy by trained nurses in high-risk octogenarians: a prospective, randomized, controlled study. Endoscopy. 2009;41:295–298.
Wehrmann T, Kokabpick S, Lembcke B, Caspary WF, Seifert H. Efficacy and safety of intravenous propofol sedation during routine ERCP: a prospective, controlled study. Gastrointest Endosc. 1999;49:677–683.
Goudra BG, Singh PM, Sinha AC. Anesthesia for ERCP: impact of anesthesiologist’s experience on outcome and cost. Anesthesiol Res Pract. 2013;2013:570518.
Goudra BG, Singh PM, Manjunath A, Reihmer J. Sedation spectrum in patients undergoing advanced gastrointestinal (GI) endoscopic procedures with propofol, presented at the annual meeting of International Society of Anesthetic Pharmacology, San Fransisco October 11th 2013.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goudra, B.G., Singh, P.M., Gouda, G. et al. Safety of Non-anesthesia Provider-Administered Propofol (NAAP) Sedation in Advanced Gastrointestinal Endoscopic Procedures: Comparative Meta-Analysis of Pooled Results. Dig Dis Sci 60, 2612–2627 (2015). https://doi.org/10.1007/s10620-015-3608-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3608-x