Abstract
Background and Aim
The presence of an association between Barrett’s metaplasia and colonic neoplasia has remained controversial. The aim of the study was to test the presence of this association, using a large national database.
Methods
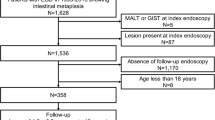
From a computerized database of surgical pathology reports, we selected 203,000 subjects who underwent colonoscopy and esophago-gastro-duodenoscopy with biopsy results available from both procedures. In a case–control study we compared the occurrence of Barrett’s metaplasia in patients with and without various types of colonic neoplasms.
Results
Barrett’s metaplasia occurred more frequently among patients with hyperplastic polyps (OR = 2.14, 95 % CI 2.02–2.27), adenomatous polyps (2.52, 2.41–2.64), advanced adenomas (2.10, 1.90–2.32), villous adenomas or adenomas with high-grade (HG) dysplasia (2.45, 2.28–2.64), and colonic adenocarcinomas (1.75, 1.39–2.22). The association between Barrett’s metaplasia and colonic neoplasm applied similarly to polyps of different size, number and location within the large bowel. These types of association could also be confirmed when analyzed separately for Barrett’s metaplasia characterized by low-grade or HG dysplasia, as well as esophageal adenocarcinoma.
Conclusions
The data support the existence of a true association between Barrett’s metaplasia and various types of colonic neoplasm. The association may be more interesting for its potential insights into the pathogenesis of the two disorders than its actual clinical implications.
Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- EGD:
-
Esophago-gastro-duodenoscopy
- HG:
-
High-grade
- OR:
-
Odds ratio
- P :
-
Probability
References
Sontag SJ, Schnell TG, Chejfec G, et al. Barrett’s oesophagus and colonic tumours. Lancet. 1985;1:946–949.
Howden CW, Hornung CA. A systematic review of the association between Barrett’s esophagus and colon neoplasms. Am J Gastroenterol. 1995;90:1814–1819.
Siersema PD, Yu S, Sahbaie P, et al. Colorectal neoplasia in veterans is associated with Barrett’s esophagus but not with proton-pump inhibitor or aspirin/NSAID use. Gastrointest Endosc. 2006;63:581–586.
Bollschweiler E, Schloesser T, Leers J, Vallböhmer D, Schäfer H, Hölscher AH. High prevalence of colonic polyps in white males with esophageal adenocarcinoma. Dis Colon Rectum. 2009;52:299–304.
de Jonge PJ, van Blankenstein M, Looman CW, Casparie MK, Meijer GA, Kuipers EJ. Risk of colorectal cancer in patients with Barrett’s esophagus: a Dutch population-based study. Am J Gastroenterol. 2010;105:77–83.
Poorman JC, Lieberman DA, Ippoliti AF, Weber LJ, Weinstein WM. The prevalence of colonic neoplasia in patients with Barrett’s esophagus: prospective assessment in patients 50–80 years old. Am J Gastroenterol. 1997;92:592–596.
Laitakari R, Laippala P, Isolauri J. Barrett’s oesophagus is not a risk factor for colonic neoplasia: a case–control study. Ann Med. 1995;27:499–502.
Lagergren J, Nyren O. No association between colon cancer and adenocarcinoma of the oesophagus in a population based cohort study in Sweden. Gut. 1999;44:819–821.
Murphy SJ, Anderson LA, Mainie I, et al. Incidence of colorectal cancer in a population-based cohort of patients with Barrett’s oesophagus. Scand J Gastroenterol. 2005;40:1449–1453 (erratum in: Scand J Gastroenterol. 2006;41:247).
Solaymani-Dodaran M, Logan RF, West J, Card T, Coupland C. Risk of extra-oesophageal malignancies and colorectal cancer in Barrett’s oesophagus and gastro-oesophageal reflux. Scand J Gastroenterol. 2004;39:680–685.
Schouten LJ, Steevens J, Huysentruyt CJ, et al. Total cancer incidence and overall mortality are not increased among patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2011;9:754–761.
Cook MB, Wild CP, Everett SM, et al. Risk of mortality and cancer incidence in Barrett’s esophagus. Cancer Epidemiol Biomarkers Prev. 2007;16:2090–2096.
Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International workshop on the histopathology of gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161–1181.
Srivastava A, Odze RD, Lauwers GY, Redston M, Antonioli DA, Glickman JN. Morphologic features are useful in distinguishing Barrett esophagus from carditis with intestinal metaplasia. Am J Surg Pathol. 2007;31:1733–1741.
Winawer SJ, Zauber AG. The advanced adenoma as the primary target of screening. Gastrointest Endosc Clin N Am. 2002;12:1–9.
Sonnenberg A, Amorosi LS, Lacey MJ, Lieberman DA. Patterns of endoscopy in the United States: analysis of data from the Centers for Medicare and Medicaid Services and the National Endoscopic Database. Gastrointest Endosc. 2008;67:489–496.
Sontag S. The Colono–Barrett relationship: a tie that will not die. Gastrointest Endosc. 2006;63:587–589.
Samanic C, Chow WH, Gridley G, Jarvholm B, Fraumeni JF Jr. Relation of body mass index to cancer risk in 362,552 Swedish men. Cancer Causes Control. 2006;17:901–909.
Corley DA, Kubo A, Levin TR, et al. Abdominal obesity and body mass index as risk factors for Barrett’s esophagus. Gastroenterology. 2007;133:34–41.
Lagergren J. Influence of obesity on the risk of esophageal disorders. Nat Rev Gastroenterol Hepatol. 2011;8:340–347.
Bernstein H, Bernstein C, Payne CM, Dvorak K. Bile acids as endogenous etiologic agents in gastrointestinal cancer. World J Gastroenterol. 2009;15:3329–3340.
McQuaid KR, Laine L, Fennerty MB, Souza R, Spechler SJ. Systematic review: the role of bile acids in the pathogenesis of gastro-oesophageal reflux disease and related neoplasia. Aliment Pharmacol Ther. 2011;34:146–165.
Thorburn CM, Friedman GD, Dickinson CJ, Vogelman JH, Orentreich N, Parsonnet J. Gastrin and colorectal cancer: a prospective study. Gastroenterology. 1998;115:275–280.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Trivers KF, Sabatino SA, Stewart SL. Trends in esophageal cancer incidence by histology, United States, 1998–2003. Int J Cancer. 2008;123:1422–1428.
American Gastroenterological Association, Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology. 2011;140:1084–1091.
Wani S, Falk G, Hall M, et al. Patients with nondysplastic Barrett’s esophagus have low risks for developing dysplasia or esophageal adenocarcinoma. Clin Gastroenterol Hepatol. 2011;9:220–227.
Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–1595.
Conflict of interest
Robert M. Genta is employed by Miraca Life Sciences, Irving, TX, USA. Amnon Sonnenberg is supported by a grant from Takeda Pharmaceuticals. No funding was obtained for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sonnenberg, A., Genta, R.M. Barrett’s Metaplasia and Colonic Neoplasms: A Significant Association in a 203,534-Patient Study. Dig Dis Sci 58, 2046–2051 (2013). https://doi.org/10.1007/s10620-013-2565-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2565-5