Abstract
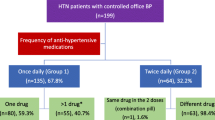
The aim of our study was to evaluate whether captopril administered at night, can shift the circadian blood pressure (BP) from a nondipper to a dipper pattern in adequately controlled hypertensive patients, who continued their antihypertensive therapy. In a prospective, randomized, double blind, placebo-controlled designed study, we enrolled 121 treated, adequately controlled nondipping hypertensive patients. All patients were randomly assigned to 12.5 mg captopril or placebo treatment administered at night. In case of nondippers, the dosage of captopril or placebo was doubled after two weeks of treatment, while for dippers antihypertensive regimens were not changed. After another two weeks, all patients underwent ambulatory BP monitoring. Our results show that at the end of the active treatment period, the prevalence of a dipping diurnal BP pattern in the captopril group (70%) was significantly higher than that in the placebo group (9.8%, P < 0.001). Nighttime BP, night/day BP ratio, nighttime BP load and 24-h systolic BP were significantly lower after 4 weeks nighttime captopril treatment compared to baseline. In conclusion, the present study demonstrates for the first time that captopril administered at night can restore the diurnal BP rhythm and decrease the elevated night/day BP ratio in appropriately controlled, nondipper hypertensive patients. These results were mainly due to the decrease of nighttime BP.
Similar content being viewed by others
References
Gueyffier F, Boutitie F, Boissel JP, et al. Effect of antihypertensive drug treatment on cardiovascular outcomes in women and men. A meta-analysis of individual patient data from randomized, controlled trials. The INDANA Investigators. Ann Intern Med 1997;126:761–767.
Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: Results of prospectively-designed overviews of randomised trials. Lancet 2003;362:1527–1535.
Psaty BM, Smith NL, Siscovick DS, et al. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA 1997;277:739–745.
Cobanian AV, Bakris GL, Black HR, et al. and the National High Blood Pressure Education Program Coordinate Committee. Seventh report of the joint national committee on prevention, detection, evalution, and treatment of high blood pressure. Hypertension 2003;42:1206–1250.
O’Brien E, Sheridan J, O’Malley K. Dippers and non-dippers. Lancet 1988;13:397.
Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension 1994;24:793–801.
Hoshide S, Kario K, Hoshide Y, et al. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens 2003;16:434–438.
Ohkubo T, Hozawa A, Yamaguchi J, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: The Ohasama study. J Hypertens 2002;20:2183–2189.
Cuspidi C, Michev I, Meani S, et al. Reduced nocturnal fall in blood pressure, assessed by two ambulatory blood pressure monitorings and cardiac alterations in early phases of untreated essential hypertension. J Hum Hypertens 2003;17:245–251.
Zweiker R, Eber B, Schumacher M, Toplak H, Klein W. “Non-dipping” related to cardiovascular events in essential hypertensive patients. Acta Med Austriaca 1994;21:86–89.
Yamamoto Y, Akiguchi I, Oiwa K, Hayashi M, Kimura J. Adverse effect of nighttime blood pressure on the outcome of lacunar infarct patients. Stroke 1998;29:570–576.
Ko GT, Chan HC. Restoration of nocturnal dip in blood pressure is associated with improvement in left ventricular ejection fraction. A 1-year clinical study comparing the effects of amlodipine and nifedipine retard on ambulatory blood pressure and left ventricular systolic function in Chinese hypertensive type 2 diabetic patients. Intern J Cardiology 2003;89:159–166.
Svensson P, de Faire U, Sleight P, Yusuf S, Ostergren J. Comparative effects of ramipril on ambulatory and office blood pressures: A HOPE Substudy. Hypertension 2001;38:e28–e32.
Hermida RC, Calvo C, Ayala DE, et al. Administration time-dependent effects of valsartan on ambulatory blood pressure in hypertensive subjects. Hypertension 2003;42:283–290.
Qiu YG, Yao XY, Tao QM, et al. Circadian blood pressure profile and its influencing factors in treated essential hypertensive patients. Zhonghua Liu Xing Bing Xue Za Zhi 2004;25:710–714.
Verdecchia P. Prognostic value of ambulatory blood pressure: Current evidence and clinical implications. Hypertension 2000;35:844–851.
Qiu YG, Chen JZ, Zhu JH, Yao XY. Differential effects of morning or evening dosing of amlodipine on circadian blood pressure and heart rate. Cardiovascular Drugs and Therapy 2003;17:335–341.
Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA 1999;282:539–546.
Uzu T, Kimura G. Diuretics shift circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation 1999;100:1635–1638.
Lemmer B. Differential effects of antihypertensive drugs on circadian rhythm in blood pressure from the chronobiological point of view. Blood Press Monitor 1996;1:161–169.
Palatini P, Mos L, Motolese M, et al. Effect of evening versus morning benazepril on 24-hour blood pressure: A comparative study with continuous intraarterial monitoring. Int J Clin Pharmacol Ther Toxicol 1993;31:295–300.
White WB, Mansoor GA, Pickering TG, et al. Differential effects of morning and evening dosing of nisoldipine ER on circadian blood pressure and heart rate. Am J Hypertens 1999;12:806–814.
Scheer FA, Van Montfrans GA, van Someren EJ, Mairuhu G, Buijs RM. Daily nighttime melatonin reduces blood pressure in male patients with essential hypertension. Hypertension 2004;43:192–197.
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000;342:145–153.
Svensson P, de Faire U, Sleight P, Yusuf S, Ostergren J. Comparative effects of ramipril on ambulatory and office blood pressures: A HOPE Substudy. Hypertension 2001;38:e28–e32.
White WB, Dey HM, and Schulman P. Assessment of the daily blood pressure load as a determinant of cardiac function in patients with mild-to-moderate hypertension. Am Heart J 1989;118:782–795.
Sorof JM, Cardwell G, Franco K, Portman RJ. Ambulatory blood pressure and left ventricular mass index in hypertensive children. Hypertension 2002;39:903–908.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 1990;322:1561–1566.
Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F. Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension 2000;35:580–586.
Pfeffer M. Clinical implications of left ventricular hypertrophy in systemic hypertension. Cardiovasc Rev Rep Jan 1991;53–60.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qiu, YG., Zhu, JH., Tao, QM. et al. Captopril Administered at Night Restores the Diurnal Blood Pessure Rhythm in Adequately Controlled, Nondipping Hypertensives. Cardiovasc Drugs Ther 19, 189–195 (2005). https://doi.org/10.1007/s10557-005-1376-0
Issue Date:
DOI: https://doi.org/10.1007/s10557-005-1376-0