Abstract
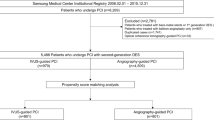
Stenting coronary artery bifurcation lesion is associated with suboptimal clinical results. Clinical improvement by intravascular ultrasound (IVUS) guided bifurcation stenting is controversial because small-side-branch (SB), low-risk patients and false bifurcations were included in previous studies that had no exact IVUS criteria for optimal stent expansion. We sought determine whether IVUS guidance is superior to angiography guidance for patients with true and complex bifurcation lesions. Between July 2006 and July 2012, 1465 patients with unstable angina and Medina 1,1,1 or 0,1,1 coronary bifurcation lesions were prospectively studied. 310 patients in the IVUS guidance (defined as stent symmetry index > 0.7, stent expansion index > 0.9, well apposition, and no Type B/C dissection) group were paired with 620 patients in the angiography group by propensity score-matching. The primary endpoint was the rate of composite major adverse cardiac events (MACE) (cardiac death, myocardial infarction (MI), or clinically-driven target vessel revascularization) at 1-year and at the end of study after indexed procedure. Use of IVUS guidance was mainly driven by stenting technique selection and identification of lesions’ specificities. IVUS criteria for optimal stent expansion were achieved in 82.9% of patients which contribute to IVUS group data assessment and the rest did not meet optimal criteria. MACE occurred in 10.0% of patients at 1-year follow-up and 15.2% at the 7-year follow-up in the IVUS group, significantly different from 15.0% (p = 0.036) and 22.4% (p = 0.01) in the angiography group, respectively. Compared to angiography guidance, IVUS guidance also resulted in a lower 7-year cardiac death rate (6.5 versus 1.3%, p = 0.002) and MI (8.4 versus 2.3%, P < 0.001). Any revascularization was also statistically lower in the IVUS group through whole study period, compared to the angiography group. Lower MACE rates were observed in IVUS guidance group in a 7-year follow-up compared with angiography guidance alone.



Similar content being viewed by others
References
Chen SL, Santoso T, Zhang JJ et al (2011) A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (double kissing crush versus provisional stenting technique for treatment of coronary bifurcation lesions) Trial. J Am Coll Cardiol 57:914–920
Chen SL, Xu B, Han YL et al (2013) Comparison of double kissing crush versus culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol 61:1482–1488
Colombo A, Bramucci E, Saccà S et al (2009) Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (coronary bifurcations: application of the crushing technique using sirolimus-eluting stents) study. Circulation 119:71–78
Chen SL, Xu B, Han YL et al (2015) Clinical outcome after DK crush versus culotte stenting of distal left main bifurcation lesions: the 3-year follow-up results of the DKCRUSH-III study. JACC Cardiovasc Interv 8:1335–1342
Chen SL, Santoso T, Zhang JJ et al (2017) Clinical outcome of double kissing crush versus provisional stenting of coronary artery bifurcation lesions: the 5-year follow-up results from a randomized and multicenter DKCRUSH-II study (randomized study on double kissing crush technique versus provisional stenting technique for coronary artery bifurcation lesions). Circ Cardiovasc Interv 10:e004497
Andell P, Karlsson S, Mohammad MA et al (2017) Intravascular ultrasound guidance is associated with better outcome in patients undergoing unprotected left main coronary artery stenting compared with angiography guidance alone. Circ Cardiovasc Interv 10:e004813
Mintz G (2014) Clinical utility of intravascular imaging and physiology in coronary artery disease. J Am Coll Cardiol 64:207–222
Kim JS, Hong MK, Ko YG et al (2011) Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: data from a Korean multicenter bifurcation registry. Am Heart J 161:180–187
Kim SH, Kim YH, Kang SJ et al (2010) Long-term outcomes of intravascular ultrasound-guided stenting in coronary bifurcation lesions. Am J Cardiol 106:612–618
Biondi-Zoccai G, Sheiban I, Romagnoli E et al (2011) Is intravascular ultrasound beneficial for percutaneous coronary intervention of bifurcation lesions? Evidence from a 4314-patient registry. Clin Res Cardiol 100:1021–1028
Chen SL, Sheiban I, Xu B et al (2014) Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complex bifurcation lesions on clinical outcomes after percutaneous coronary Intervention using drug-eluting stents). JACC Cardiovasc Interv 7:1266–1276
Tian NL, Gami SK, Ye F et al (2015) Angiographic and clinical comparisons of intravascular ultrasound- versus angiography-guided drug-eluting stent implantation for patients with chronic total occlusion lesions: 2-year results from a randomized AIR-CTO study. EuroIntervention 10:1409–1417
Medina A, Suarez de Lezo J et al (2006) A new classification of coronary bifurcation lesions. Rev Esp Cardiol 2:183
Louvard Y, Thomas M, Dzavik V et al (2008) Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv 2:175–183
Mauri L, Hsieh WH, Massaro JM et al (2007) Stent thrombosis in randomized clinical trials of drug-eluting stents. NEJM 356:1020–1029
Hahn JY, Chun WJ et al (2013) Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II registry (coronary bifurcation stenting). J Am Coll Cardiol 62:1654–1659
Costa RA, Feres F, Staico R al (2013) Vessel remodeling and plaque distribution in side branch of complex coronary bifurcation lesions: a grayscale intravascular ultrasound study. Int J Cardiovasc Imaging 29:1657–1666
Sakamoto N, Hoshino Y, Mizukami H et al (2016) Intravascular ultrasound predictors of acute side branch occlusion in coronary artery bifurcation lesions just after single stent crossover. Catheter Cardiovasc Interv 87:243–250
Sato K, Naganuma T, Costopoulos C et al (2014) Calcification analysis by intravascular ultrasound to define a predictor of left circumflex narrowing after cross-over stenting for unprotected left main bifurcation lesions. Cardiovasc Revasc Med 15:80–85
Rahman S, Leesar T, Cilingiroglu M al (2013) Impact of kissing balloon inflation on the main vessel stent volume, area, and symmetry after side-branch dilation in patients with coronary bifurcation lesions: a serial volumetric intravascular ultrasound study. JACC Cardiovasc Interv 6:923–931
Papadopoulou SL, Brugaletta S, Garcia-Garcia HM et al (2012) Assessment of atherosclerotic plaques at coronary bifurcations with multi-detector computed tomography angiography and intravascular ultrasound-virtual histology. Eur Heart J Cardiovasc Imaging 13:635–642
Shan SJ, Ye F, Liu ZZ et al (2013) Coronary bifurcation lesions treated with double kissing crush technique compared to classical crush technique: serial intravascular ultrasound analysis. Chin Med J 126:1247–1251
Chen SL, Ye F, Zhang JJet al (2013) Intravascular ultrasound-guided systematic two-stent techniques for coronary bifurcation lesions and reduced late stent thrombosis. Catheter Cardiovasc Interv 81:456–463
Patel Y, Depta JP, Novak E et al (2012) Long-term outcomes with use of intravascular ultrasound for the treatment of coronary bifurcation lesions. Am J Cardiol 109:960–965
Hong MK, Mintz GS, Lee CW et al (2006) Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J 27:1305–1310
Okumura M, Ozaki Y, Ishii J et al (2007) Restenosis and stent fracture following sirolimus-eluting stent (SES) implantation. Circ J 71:1669–1677
Kang SJ, Ahn JM, Song H et al (2011) Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ Cardiovasc Interv 4:562–569
Kim JS, Kang TS, Mintz GS et al (2013) Randomized comparison of clinical outcomes between intravascular ultrasound and angiography-guided drug-eluting stent implantation for long coronary artery stenoses. JACC Cardiovasc Interv 6:369–376
Hong SJ, Kim BK, Shin DH et al (2015) Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA 314:2155–2163
Kim BK, Shin DH, Hong MK et al (2015) Clinical impact of intravascular ultrasound-guided chronic total occlusion intervention with zotarolimus-eluting versus biolimus-eluting stent implantation: randomized study. Circ Cardiovasc Interv 8:e002592
Acknowledgements
We deeply acknowledge Dr. Bao-Xiang Duan (Chair) as the director of the independent committee. We thank Ms. Ling Lin (China, Clinical trial coordinator), Ms. Hai-Mei Xu (China), and Linda Liason (Indonesia) for their contributions to the completion of this study. We also appreciate the support through the whole study period of the Cooperative Innovational Center of Nanjing Medical University.
Disclosures
The authors certify that: (1) the paper is not under consideration elsewhere, (2) no part of the paper has been previously published, (3) all of the authors have read and approved the manuscript, and (4) none of the authors has any relevant disclosures.
Funding
The study was funded by a grant from the National Science Foundation of China (Funding No. NSFC 91639303).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Ethical approval
This study was approved by the local ethics committee of our institution.
Informed consent
Informed consent was obtained from the patient.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, L., Xu, T., Xue, XJ. et al. Intravascular ultrasound-guided drug-eluting stent implantation is associated with improved clinical outcomes in patients with unstable angina and complex coronary artery true bifurcation lesions. Int J Cardiovasc Imaging 34, 1685–1696 (2018). https://doi.org/10.1007/s10554-018-1393-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1393-2