Abstract
Purpose
Tumors of the inner quadrants of the breast are associated with poorer survival than those of the upper-outer quadrant. It is unknown whether racial differences in breast cancer outcomes are modified by breast quadrant, in addition to comparisons among Asian subgroups.
Methods
Using the Surveillance, Epidemiology, and End Results database, we analyzed data among women diagnosed with non-metastatic invasive breast cancer between 1990 and 2014. We performed Cox proportional hazards regression models to assess the associations of race with breast cancer-specific survival and overall survival, stratified by breast quadrants. The models were adjusted for age, year of the diagnosis, tumor size, grade, histological type, tumor laterality, lymph node, estrogen receptor, progesterone receptor, and treatments.
Results
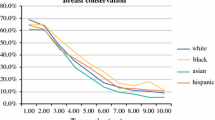
Among 454,154 patients (73.0% White, 10.0% Black, 7.8% Asian/PI, and 9.2% Hispanic), 54.3% had tumors diagnosed in the upper-outer quadrant of the breast. Asian/PI women were more likely than White to have tumors diagnosed in the nipple/central portion of the breast and were less likely to have diagnosed in the upper-outer quadrant (P < 0.001), despite a similar distribution of breast quadrant between Black, Hispanic, and White women. Compared with White women, the multivariable-adjusted hazard ratios of breast cancer-specific mortality were 1.41 (95% CI 1.37–1.44) in Black women, 0.82 (95% CI 0.79–0.85) in Asian women, and 1.05 (95% CI 1.02–1.09) in Hispanic women. Among Asian subgroups, Japanese American women had a lower risk of breast cancer-specific mortality (HR = 0.68, 95% CI 0.62–0.74) compared with White women. Overall survival was similar to breast cancer-specific survival in each race group. The race-associated risks did not vary significantly by breast quadrants for breast cancer-specific mortality and all-cause mortality.
Conclusions
Differences in breast cancer survival by race could not be attributed to tumor locations. Understanding the cultural, biological, and lifestyle factors that vary between White, African American, and ethnic subgroups of Asian American women may help explain these survival differences.


Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the first author on reasonable request.
Abbreviations
- BCS:
-
Breast-conserving surgery
- BCSM:
-
Breast cancer-specific mortality
- BCSS:
-
Breast cancer-specific survival
- CI:
-
Confidence interval
- ER:
-
Estrogen receptor
- HR:
-
Hazard ratio
- NOS:
-
Not otherwise specified
- OS:
-
Overall survival
- PI:
-
Pacific Islander
- PR:
-
Progesterone receptor
- SEER:
-
Surveillance, Epidemiology, and End Results
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin. 69:7–34
Smith RA, Andrews KS, Brooks D et al (2017) Cancer screening in the United States, 2017: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 67:100–121
DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A (2016) Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin. 66:31–42
Lohrisch C, Jackson J, Jones A, Mates D, Olivotto IA (2000) Relationship between tumor location and relapse in 6,781 women with early invasive breast cancer. J Clin Oncol 18:2828–2835
Zucali R, Mariani L, Marubini E et al (1998) Early breast cancer: evaluation of the prognostic role of the site of the primary tumor. J Clin Oncol 16:1363–1366
Gaffney DK, Tsodikov A, Wiggins CL (2003) Diminished survival in patients with inner versus outer quadrant breast cancers. J Clin Oncol 21:467–472
Siotos C, McColl M, Psoter K et al (2018) Tumor site and breast cancer prognosis. Clinical Breast Cancer 18:e1045–e1052
Perkins CI, Hotes J, Kohler BA, Howe HL (2004) Association between breast cancer laterality and tumor location, United States, 1994–1998. Cancer Causes Control: CCC 15:637–645
Lee AH (2005) Why is carcinoma of the breast more frequent in the upper outer quadrant? A case series based on needle core biopsy diagnoses. Breast (Edinburgh, Scotland) 14:151–152
Bao J, Yu KD, Jiang YZ, Shao ZM, Di GH (2014) The effect of laterality and primary tumor site on cancer-specific mortality in breast cancer: a SEER population-based study. PLoS ONE 9:e94815
Colleoni M, Zahrieh D, Gelber RD et al (2005) Site of primary tumor has a prognostic role in operable breast cancer: the international breast cancer study group experience. J Clin Oncol 23:1390–1400
Sohn VY, Arthurs ZM, Sebesta JA, Brown TA (2008) Primary tumor location impacts breast cancer survival. Am J Surg 195:641–644
Giess CS, Keating DM, Osborne MP, Ng YY, Rosenblatt R (1998) Retroareolar breast carcinoma: clinical, imaging, and histopathologic features. Radiology 207:669–673
Nicholson BT, Harvey JA, Cohen MA (2009) Nipple-areolar complex: normal anatomy and benign and malignant processes. Radiographics 29:509–523
Turner-Warwick RT (1959) The lymphatics of the breast. Br J Surg 46:574–582
Savaridas SL, Spratt JD, Cox J (2015) Incidence and potential significance of internal mammary lymphadenopathy on computed tomography in patients with a diagnosis of primary breast cancer. Breast Cancer: Basic Clin Res 9:59–65
Gou ZC, Liu XY, Xiao Y, Zhao S, Jiang YZ, Shao ZM (2018) Decreased survival in patients with carcinoma of axillary tail versus upper outer quadrant breast cancers: a SEER population-based study. Cancer Manage Res 10:1133–1141
Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA (2015) Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA 313:165–173
National Cancer Institute. Surveillance, Epidemiology, and End Results program. SEER incidence data, 1973-2015.
National Cancer Institute. Surveillance, Epidemiology, and End Results program. Quadrants of the Breast.
Park JJ, Humble S, Sommers BD, Colditz GA, Epstein AM, Koh HK (2018) Health Insurance for Asian Americans, Native Hawaiians, and Pacific Islanders Under the Affordable Care Act. JAMA Intern Med 178:1128–1129
Gomez SL, Von Behren J, McKinley M et al (2017) Breast cancer in Asian Americans in California, 1988–2013: increasing incidence trends and recent data on breast cancer subtypes. Breast Cancer Res Treat 164:139–147
VanderWeele TJ (2009) On the distinction between interaction and effect modification. Epidemiology (Cambridge, Mass.). 20:863–871
Shahar KH, Buchholz TA, Delpassand E et al (2005) Lower and central tumor location correlates with lymphoscintigraphy drainage to the internal mammary lymph nodes in breast carcinoma. Cancer 103:1323–1329
Warner ET, Tamimi RM, Hughes ME et al (2015) Racial and ethnic differences in breast cancer survival: mediating effect of tumor characteristics and sociodemographic and treatment factors. J Clin Oncol 33:2254–2261
Sakamoto G, Sugano H (1991) Pathology of breast cancer: present and prospect in Japan. Breast Cancer Res Treat 18(Suppl 1):S81–S83
Stemmermann GN (1991) The pathology of breast cancer in Japanese women compared to other ethnic groups: a review. Breast Cancer Res Treat 18(Suppl 1):S67–S72
Shoemaker ML, White MC, Wu M, Weir HK, Romieu I (2018) Differences in breast cancer incidence among young women aged 20-49 years by stage and tumor characteristics, age, race, and ethnicity, 2004-2013. Breast Cancer Res Treat 169:595–606
Lamb EP, Pritchard FE, Nouer SS et al (2018) Understanding disparities in breast cancer care in Memphis. Tennessee Am Surg 84:620–627
Parkes A, Warneke CL, Clifton K et al (2018) Prognostic factors in patients with metastatic breast cancer with bone-only metastases. Oncologist 23:1282–1288
DeSantis CE, Siegel RL, Sauer AG et al (2016) Cancer statistics for African Americans, 2016: progress and opportunities in reducing racial disparities. CA Cancer J Clin. 66:290–308
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer 109:1721–1728
Akinyemiju T, Moore JX, Altekruse SF (2015) Breast cancer survival in African-American women by hormone receptor subtypes. Breast Cancer Res Treat 153:211–218
Newman LA, Griffith KA, Jatoi I, Simon MS, Crowe JP, Colditz GA (2006) Meta-analysis of survival in African American and white American patients with breast cancer: ethnicity compared with socioeconomic status. J Clin Oncol 24:1342–1349
Kwan ML, John EM, Caan BJ et al (2014) Obesity and mortality after breast cancer by race/ethnicity: The California Breast Cancer Survivorship Consortium. Am J Epidemiol 179:95–111
Nahleh Z, Otoukesh S, Mirshahidi HR et al (2018) Disparities in breast cancer: a multi-institutional comparative analysis focusing on American Hispanics. Cancer Med 7:2710–2717
Liu N, Johnson KJ, Ma CX (2018) Male breast cancer: an updated surveillance, epidemiology, and end results data analysis. Clin Breast Cancer 18:e997–e1002
Haji-Jama S, Gorey KM, Luginaah IN, Balagurusamy MK, Hamm C (2013) Health insurance mediation of the Mexican American non-Hispanic white disparity on early breast cancer diagnosis. SpringerPlus 2:285
Wheeler SB, Reeder-Hayes KE, Carey LA (2013) Disparities in breast cancer treatment and outcomes: biological, social, and health system determinants and opportunities for research. Oncologist 18:986–993
Stevenson JKR, Cheung MC, Earle CC et al (2018) Chinese and South Asian ethnicity, immigration status, and clinical cancer outcomes in the Ontario Cancer System. Cancer 124:1473–1482
Gomez SL, Glaser SL (2006) Misclassification of race/ethnicity in a population-based cancer registry (United States). Cancer Causes Control: CCC 17:771–781
Swallen KC, Glaser SL, Stewart SL, West DW, Jenkins CN, McPhee SJ (1998) Accuracy of racial classification of Vietnamese patients in a population-based cancer registry. Ethn Dis 8:218–227
Duggan MA, Anderson WF, Altekruse S, Penberthy L, Sherman ME (2016) The Surveillance, Epidemiology, and End Results (SEER) Program and Pathology: toward strengthening the critical relationship. Am J Surg Pathol 40:e94–e102
Sogaard M, Thomsen RW, Bossen KS, Sorensen HT, Norgaard M (2013) The impact of comorbidity on cancer survival: a review. Clin Epidemiol 5:3–29
Funding
Dr. Han was supported by foundations from Barnes-Jewish Hospital and Breast Cancer Research Foundation (award ID: BCRF-17-028). Dr. Colditz is supported by the Breast Cancer Research Foundation. Drs. Moore, Langston, Fuzzell, Khan, and Lewis were supported by the Washington University School of Medicine, Public Health Sciences Division Postdoctoral Training in Cancer Prevention and Control, and a training grant from the National Cancer Institute of the National Institutes of Health under award number T32CA190194. YL is supported by an American Cancer Society—Denim Days Research Scholar Grant (RSG-18-116-01-CPHPS) and the National Cancer Institute (R01CA215418). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
As this study is based on a publicly available database without identifying patient information, informed consent was not needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Han, Y., Moore, J.X., Langston, M. et al. Do breast quadrants explain racial disparities in breast cancer outcomes?. Cancer Causes Control 30, 1171–1182 (2019). https://doi.org/10.1007/s10552-019-01222-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01222-x