Abstract
Purpose
This study examined a cancer diagnosis, versus orthopedic surgery, as a teachable moment for recruiting smokers and treating nicotine dependence among patients’ relatives.
Methods
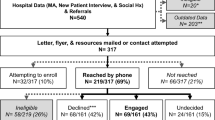
Cancer patients and, for comparison, orthopedic patients at the University of Pennsylvania Health System were approached for referrals of relatives for a smoking cessation program, which involved behavioral counseling and nicotine patches. Primary outcomes were rate of program enrollment and rate of smoking abstinence. Potential mediators of smoking cessation were explored (e.g., treatment adherence, depression, anxiety). Two hundred and thirty-four relatives (113 cancer, 121 orthopedic) were considered eligible for the cessation program and comprised the study sample.
Results
Relatives of oncology patients were significantly more likely to enroll in the smoking cessation program, vs. orthopedic relatives (75 % vs. 60 %; OR = 1.96, 95 % CI 1.07–3.61, p = .03), but they were not significantly more likely to remain in the program (61 % vs. 52 %) or quit smoking (19 % vs. 26 %; p’s > .05). Compared to orthopedic relatives, oncology relatives showed significantly lower nicotine patch adherence and significantly greater levels of negative affect and depression and anxiety symptoms during treatment (p’s < .05). Further, orthopedic relatives, compared to oncology relatives, showed a greater reduction in the perceived benefits of smoking (p = .06), which was significantly associated with abstinence (p = .02).
Conclusions
While a family member’s cancer diagnosis may serve as a teachable moment for a smoker to enroll in a smoking cessation treatment program, high levels of psychological distress and perceptions of the benefits of smoking and low levels of treatment adherence may undermine successful abstinence among this population.


Similar content being viewed by others
References
USDHS (2012) Current cigarette smoking among adults-United States, 2011. MMWR 61:889–894
USDHS (2011) Quitting smoking among adults-United States, 2001–2010. MMWR 60:1513–1519
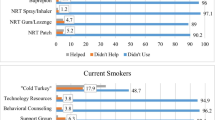
Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG (2008) Use of smoking-cessation treatments in the United States. Am J Prev Med 34:102–111
Fix BV, Hyland A, Rivard C et al (2011) Usage patterns of stop smoking medications in Australia, Canada, the United Kingdom, and the United States: findings from the 2006–2008 International Tobacco Control (ITC) four country survey. Int J Environ Res Pub Health 8:222–233
Gariti P, Levin S, Whittingham T et al (2008) Why do those who request smoking treatment fail to attend the first appointment? J Sub Ab Treat 35:62–67
Cohen DJ, Clark EC, Lawson PJ, Casucci BA, Flocke SA (2011) Identifying teachable moments for health behavior counseling in primary care. Patient Educ Couns 85:e8–e15
Katz DA, Muehlenbruch DR, Brown RL, Fiore MC, Baker TB (2004) Effectiveness of implementing the agency for healthcare research and quality smoking cessation clinical practice guideline: a randomized, controlled trial. J Natl Cancer Inst 96:594–603
McBride CM, Scholes D, Grothaus LC, Curry SJ, Ludman E, Albright J (1999) Evaluation of a minimal self-help smoking cessation intervention following cervical cancer screening. Prev Med 29:133–138
Winickoff JP, Healey EA, Regan S et al (2010) Using the postpartum hospital stay to address mothers’ and fathers’ smoking: the NEWS study. Pediatrics 125:518–525
Warner DO, Klesges RC, Dale LC et al (2011) Clinician-delivered intervention to facilitate tobacco quitline use by surgical patients. Anesthesiology 114:847–855
McBride CM, Ostroff JS (2003) Teachable moments for promoting smoking cessation: the context of cancer care and survivorship. Cancer Control 10:325–333
McBride CM, Pirie PL, Curry SJ (1992) Postpartum relapse to smoking: a prospective study. Health Educ Res 7:381–390
Cox LS, Clark MM, Jett JR et al (2003) Change in smoking status after spiral chest computed tomography scan screening. Cancer 98:2495–2501
Schnoll RA, Malstrom M, James C et al (2002) Correlates of tobacco use among smokers and recent quitters diagnosed with cancer. Patient Educ Couns 46:137–145
Fiore MC, Jaén CR, Baker TB, et al. (2008) Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service
Schnoll RA, Patterson F, Wileyto P et al (2010) Efficacy of extended duration transdermal nicotine therapy: a randomized trial. Ann Intern Med 152:144–151
Heatherton TF, Kozlowski L, Frecker RC, Fagerstrom K (1991) The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict 86:1119–1127
Radloff L (1977) The CES-D scale: a new self-report depression scale for research in the general population. App Psychol Measure 1:385–401
Lerman C, Audrain J, Orleans CT et al (1996) Investigation of mechanisms linking depressed mood to nicotine dependence. Addict Beh 21:9–19
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA (1983) Manual for the state-trait anxiety inventory. Consulting Psychologists Press, Palo Alto
Tselebis A, Papaleftheris E, Balis E, Theotoka I, Ilias I (2003) Smoking related to anxiety and depression in Greek medical staff. Psychol Rep 92:529–532
Watson D, Clark LA, Tellegen A (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 54:1063–1070
Ameringer KJ, Leventhal AM (2010) Applying the tripartite model of anxiety and depression to cigarette smoking: an integrative review. Nicotine Tob Res 12:1183–1194
Brandon TH, Baker TB (1991) The Smoking Consequences Questionnaire: the subjective expected utility of smoking in college students. Psychol Assess 3:484–491
Velicer WF, DiClemente CC, Prochaska JO, Brandenburg N (1985) Decisional balance measure for assessing and predicting smoking status. J Pers Soc Psychol 48:1279–1289
Schnoll RA, Cappella J, Lerman C et al (2011) A novel recruitment message to increase enrollment into a smoking cessation treatment program: preliminary results from a randomized trial. Health Comm 10:1–8
Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE (2003) Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res 5:13–25
SRNT (2002) Biochemical verification of tobacco use and cessation. Nicotine Tob Res 4:149–159
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51:1173–1182
Dahm JL, Cook E, Baugh K et al (2009) Predictors of enrollment in a smoking cessation clinical trial after eligibility screening. J Natl Med Assoc 101:450–455
Patterson F, Wileyto EP, Segal J, Kurz J, Glanz K, Hanlon A (2010) Intention to quit smoking: role of personal and family member cancer diagnosis. Health Educ Res 25:792–802
Carpenter MJ, Jardin BF, Burris JL et al (2013) Clinical strategies to enhance the efficacy of nicotine replacement therapy for smoking cessation: A review of the literature. Drugs. doi:10.1007/s40265-013-0038-y
Flocke SA, Antognoli E, Step MM, Marsh S, Parran T, Mason MJ (2012) A teachable moment communication process for smoking cessation talk: description of a group randomized clinician-focused intervention. BMC Health Serv Res 12:109
Poghosyan H, Kennedy SL, Cooley ME (2012) The impact of computed tomography screening for lung cancer on smoking behaviors: a teachable moment? Cancer Nurs 35:446–475
van der Aalst CM, van Klaveren RJ, van den Bergh KA, Willemsen MC, de Koning HJ (2011) The impact of a lung cancer computed tomography screening result on smoking abstinence. Eur Respir J 37:1466–1473
Schnoll RA, Leone FT, Hitsman B (2013) Symptoms of depression and smoking behaviors following treatment with transdermal nicotine patch. J Addict Dis 32:46–52
Shiffman S, Sweeney CT, Ferguson SG, Sembower MA, Gitchell JG (2008) Relationship between adherence to daily nicotine patch use and treatment efficacy: secondary analysis of a 10-week randomized, double-blind, placebo-controlled clinical trial simulating over-the-counter use in adult smokers. Clin Ther 30:1852–1858
Prochaska JO, Velicer WF, Rossi JS et al (1994) Stages of change and decisional balance for 12 problem behaviors. Health Psychol 13:39–46
MacPherson L, Tull MT, Matusiewicz AK et al (2010) Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. J Consult Clin Psychol 78:55–61
Prochaska JO, Prochaska JO, Velicer WF, Fava JL, Rossi JS, Tsoh JY (2001) Evaluating a population-based recruitment approach and a stage-based expert system intervention for smoking cessation. Addict Behav 26:583–602
Mooney M, Babb D, Jensen J, Hatsukami D (2005) Interventions to increase use of nicotine gum: a randomized, controlled, single-blind trial. Nicotine Tob Res 7:565–579
Patterson F, Jepson C, Strasser AA et al (2009) Varenicline improves mood and cognition during smoking abstinence. Biol Psychiatry 65:144–149
Acknowledgments
This research was supported by grant CA126969 from National Cancer Institute. The authors thank Dr. Caryn Lerman for assistance with the trial and manuscript. The authors also thank Elisa Martinez, Paul D’Avanzo, Krystle Jackson, and Lynne Kohler who helped with the trial.
Conflict of interest
Dr. Schnoll has served as a consultant to GlaxoSmithKline, which manufactures the nicotine patch. However, GSK did not provide medication or financial support for this study. Dr. Schnoll also receives medication and placebo from Pfizer for other clinical trials, but Pfizer was not involved in the present study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinicaltrials.gov: NCT00956943.
Rights and permissions
About this article
Cite this article
Schnoll, R.A., Wileyto, E.P., Leone, F.T. et al. Is a cancer diagnosis a teachable moment for the patient’s relative who smokes?. Cancer Causes Control 24, 1339–1346 (2013). https://doi.org/10.1007/s10552-013-0212-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-013-0212-2