Abstract
Purpose
We conducted a single-arm prospective phase II trial to evaluate the efficacy and safety of oral metronomic vinorelbine combined with trastuzumab (mNH) in human epidermal growth factor receptor 2-positive (HER2-positive) metastatic breast cancer (MBC) patients.
Methods
HER2-positive MBC patients received oral vinorelbine 40 mg thrice a week and trastuzumab (loading dose of 8 mg/kg, followed by 6 mg/kg every 3 weeks) until disease progression, unacceptable toxicity, or consent withdrawal. The primary endpoints were objective response rate (ORR), clinical benefit rate (CBR; CR + PR + SD for ≥ 24 weeks). The secondary endpoints were progression-free survival (PFS), tolerability, and overall survival (OS).
Results
Twenty patients with HER2-positive MBC were enrolled, with a median of 1 prior chemotherapy regimens for MBC. Median age was 61.5 years (95% Confidence Interval (CI) 48.6–63.1). Visceral involvements presented in 14 patients (70.0%). ORR was 20.0%, and CBR was 75% with 4 PR (20.0%) and 11 SD (55.0%). The median PFS (mPFS) and median OS (mOS) were 7.4 months (95% CI 3.2–11.5) and 45.8 months (95%CI: not reached), respectively. The mPFS was 17.7 months (95%CI not reached) and 5.8 months (95%CI 5.6–5.9) in mNH as first-line and ≥ second-line therapy (log rank p = 0.03), respectively. The most common grade 1 adverse events (AEs) included nausea (15%), leukopenia (15%), ALT/AST elevation (15%), diarrhea (10%), and peripheral neuropathy (10%). Grade 2 adverse events included leukopenia (5%) and neutropenia (10%). No grade 3/4 AEs were observed.
Conclusions
Oral metronomic vinorelbine combined with trastuzumab is a well-tolerated and effective anti-tumor regimen for HER2-positive MBC.
Similar content being viewed by others
Introduction
Breast cancer, accounts for 30% female cancers, is the most frequently diagnosed cancer among women worldwide [1]. Human epidermal growth factor receptor 2 (HER2) is positive in about 20–25% breast cancer patients [2]. Metastatic breast cancer is an incurable disease, in which median survival is only 2–4 years [3] and 5-year survival rate is only about 25% [4]. The purpose of treatment in advanced breast cancer patients is to improve the quality of life, and to prolong the overall survival [5]. Several studies have showed that longer duration of chemotherapy was associated with both longer progression-free disease (PFS) and longer overall survival (OS) [6], leading to the introduction of metronomic chemotherapy term. Metronomic chemotherapy (mCHT) refers to the frequent administration of cytotoxic agents at low dose less than maximum tolerated doses with no drug-free breaks that lead to continuously anti-tumor activity and gentle adverse events [7].
Conventional chemotherapy, namely ‘maximum tolerated doses’ (MTDs) chemotherapy, uses cytotoxic drugs to kill tumor cells [8]. Different from the conventional chemotherapy, metronomic chemotherapy uses the minimum biologically effective dose of chemotherapy agent without prolonged drug-free breaks [9]. The anti-tumor mechanism of metronomic chemotherapy including indirect effects on cancer cells inhibit tumor neovascularization, regulate tumor environment, and reduce the number of regulatory T cells [10].
Several studies evaluated the efficacy and safety of metronomic chemotherapy combined with targeted therapy in HER2-positive metastatic breast cancer [11]. Orlando et al. demonstrated the activity of the combination of trastuzumab plus metronomic cyclophosphamide (CTX) and methotrexate (MTX), which showed an efficacy of 18% (95% CI 5–40%) partial remission (PR), 46% (95% CI 24–68%) stable disease (SD), a median time to progression of 6 months (range 0.7 to 18.4 months), and a median duration of treatment of 5 months (range 1 to 18 months) [12]. However, studies evaluating the combination of oral metronomic vinorelbine and trastuzumab in breast cancer are limited.
Vinorelbine is an anti-tubulin chemotherapeutic drug. Preclinical studies have demonstrated that it acts synergistically with trastuzumab in several HER2-positive breast cancer cell lines [13]. Meanwhile, trastuzumab plus vinorelbine or docetaxel (HERNATA) clinical study showed that intravenous vinorelbine (30–35 mg/m2 on days 1 and 8) combined with trastuzumab has a higher anti-tumor activity than docetaxel plus trastuzumab (TTP 15.3 vs 12.4 months, OS 38.8 vs 35.7 months, respectively) [14]. A retrospective study compared intravenous taxanes plus trastuzumab to oral vinorelbine (60 mg/m2 on days 1 and 8 of a 3-week cycle) plus trastuzumab as first-line therapy in HER2-positive metastatic breast cancer patients [15]. The result showed that the mPFS and mOS were 7 months vs. 9 months (log rank, no significant), 49 months vs. 59 months (p = 0.033), respectively. The above results inspired us to conduct a phase II clinical trial to evaluate the safety and efficacy of oral metronomic vinorelbine combined with trastuzumab (mNH) in HER2-positive advanced breast cancer.
Patients and methods
Study design
This study was a single-arm, prospective phase II clinical trial conducted at National Clinical Research Center for Cancer, China. Patients were enrolled to receive oral metronomic vinorelbine 40 mg on day 1, day 3, day 5 every week and trastuzumab 6 mg/kg (loading dose 8 mg/kg) every 3 weeks. A dose-limiting toxicity (DLT) was defined as grade 3 or 4 of any hematological and biochemical toxicity during the first month of metronomic vinorelbine plus trastuzumab treatment regimen. During the mNH treatment period, patients were followed monthly and were conducted radiological evaluation every 6 weeks, treatment was continued until disease progression or intolerable toxicities.
The primary endpoints were objective response rate (ORR) and clinical benefit rate (CBR). The secondary endpoints were progression-free survival (PFS), tolerability, and overall survival (OS). PFS was defined as the time from the date of first dose administration to earliest date of disease progression or cancer-related death, whichever occurred first. CBR was defined as the percentage of patients who have achieved complete response (CR), partial response (PR), and stable disease (SD) for ≥ 24 weeks. Overall survival (OS) was defined as the time from the date of first dose administration to date of death or last visit.
Eligibility criteria
The main eligibility criteria were as follows: female; aged ≥ 18 years; histologically or cytologically proved HER2-positive metastatic breast cancer; HER2-positive status determined by immunohistochemistry 3 + or fluorescent in situ hybridization (FISH) positive on the primary tumor site or a metastatic lesion; at least one measurable lesion defined by RECIST 1.1 criteria; regardless of any neoadjuvant and/or adjuvant therapies, or previous lines of therapy, including chemotherapy, endocrine therapy, or target therapy received for metastatic disease; performance status of 0–2 according to WHO criteria; an estimated life expectancy ≥ 12 weeks; adequate bone marrow, liver, renal, and cardiac function with normal left ventricular ejection fraction defined by our institution. The ineligibility criteria included unstable brain metastasis, second primary malignancy, and dyspnea.
The study was approved by the institutional Ethical Committee of National Clinical Research Center for Cancer.
Treatment schedule
Patients received oral vinorelbine 40 mg 3 days a week (D1, D3, D5/per week) and trastuzumab at the dose of 6 mg/kg was administered intravenously every 21 days (8 mg/kg loading dose at first administration). Endocrine therapy for hormone receptor-positive patients was not admitted during treatment.
Assessment
Tumor responses were evaluated according to the international criteria proposed by the Response Evaluation Criteria in Solid Tumors (RECIST 1.1). Tumor assessments were carried out by CT scan every 6 weeks.
Adverse events were evaluated according to the Common Terminology Criteria for Adverse Effects Version 5.0 (CTCAE 5.0).
Statistical analysis
Median PFS and OS plots were drawn using the Kaplan–Meier plot, log rank test was used to compare the difference of survival rate between the two groups. Univariable and multivariable Cox proportional regression analysis was used to assess the association between various patients or tumor characteristics and progression or death. All analyses were performed with the SPSS software (version 23.0). The survival curve was drawn by Graphpad Prism software (version 8.0). All p values were two-sided.
Results
Patients
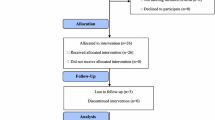
From September 2017 to August 2020, 20 patients with HER2-positive MBC from National Clinical Research Center for Cancer were enrolled. The median age was 61.5 years (range from 31 to 78). 14 patients were postmenopausal (70.0%), while 6 were premenopausal (30.0%). 14 patients presented with visceral involvement (70.0%), 6 patients presented with lymph node, bone, or chest wall metastasis (30.0%). 14 patients were hormone receptor positive (70.0%), 6 patients were hormone receptor negative (30.0%). 8 (40.0%) patients had never received chemotherapy for advanced disease, 7 (35.0%) patients had received 1 lines of chemotherapy, 4 (20.0%) patients had received 2 lines, and 1 (5.0%) patient had received 4 lines of chemotherapy. For the previous treatments, in the neoadjuvant/adjuvant treatment, 15 patients received taxanes and 5 patients received trastuzumab. In the first-line treatment, 4 received taxanes, 4 received pyrotinib, and 2 received trastuzumab. In the second-line treatment, 2 received trastuzumab and 2 received lapatinib. No taxanes were observed in patients with ≥ 2 lines of treatment.
Table 1 reports the main patient characteristics
Efficacy
Among the 20 patients who received oral metronomic vinorelbine combined with trastuzumab, 4 patients achieved partial response (20.0%), 11 patients achieved stable disease (55.0%), and 5 patients achieved progressive disease (25.0%). The duration of remission of the above 15 patients with PR or SD was more than 24 weeks. ORR was 20.0%, CBR was 75.0% (Table 2).
The median PFS (mPFS) was 7.4 months [95% Confidence Interval (CI) 3.2–11.5]. The mPFS of patients who received mNH as the first-line treatment regimen for MBC was 17.7 months (95%CI not reached), while the mPFS of patients who received mNH as ≥ second-line regimens was 5.8 months (95%CI 5.6–5.9). There was significant difference between the two groups (log rank p = 0.03) (Table 3). The longest PFS of the 20 patients was 33.5 months. Among the patients with mNH as the first-line treatment, 3 PR, 4 SD, 1 PD, ORR was 37.5% (3/8), and CBR was 87.5% (7/8). The median OS was 45.8 months (95% CI not reached) (Fig. 1).
Treatment safety
Adverse events were observed in patients during the course of study and are summarized in Table 4. Grade 1 adverse events included nausea (15%), leukopenia (15%), ALT/AST elevation (15%), diarrhea (10%), peripheral neuropathy (10%), constipation (5%), anemia (5%), cardiac toxicity (5%), increased creatine (5%), and insomnia (5%). Grade 2 adverse events included leukopenia (5%) and neutropenia (10%). No grade 3/4 adverse events were observed.
Discussion
In the present study of oral metronomic vinorelbine combined with trastuzumab (mNH) in HER2-positive MBC patients who had received a median of 2 prior treatment regimens, the median PFS was 7.4 months (95% CI 3.2–11.5), and median OS was 45.8 months (95%CI not reached), with a CBR of 75.0% (15 patients achieved PR + SD ≥ 24 weeks) and an ORR of 20%. The mPFS was 17.7 months (95%CI not reached) and 5.8 months (95%CI 5.6–5.9) in first-line therapy and ≥ second-line therapy (log rank p = 0.03). Although the sample size is limited, this study demonstrated promising efficacy of mNH regimen in HER2-positive MBC patients.
The concept of “dose intensity” is the foundation of conventional chemotherapy [16]. In the conventional chemotherapy, chemotherapeutic drugs are delivered at the highest tolerable dose in cycles with 3–4 weeks interval. However, this drug-free interval may allow cancer cells to regrow and acquire resistance. The term of metronomic chemotherapy was then introduced, which refers to low-dose chemo-drugs with shorter drug-free intervals to achieve continuous anti-tumor activity and gentle adverse events. Metronomic chemotherapy not only directly targets cancer cells but also exerts effects on tumor microenvironment [17], which is achieved by tumor angiogenesis inhibition and anti-tumor immune response activation [17]. Browder et al. suggested that metronomic chemotherapy targets tumor vascular bed and sustained apoptosis of vascular endothelial cells [10]. In the present study, patients were administered with oral vinorelbine three times a week, instead of long drug-free interval.
Orlando et al. explored the efficacy and safety of metronomic capecitabine/cyclophosphamide combined with trastuzumab (HEX) as the first-line treatment for HER2-positive patients with advanced breast cancer. The results showed that the ORR was 56.7%, CBR was 78.2%, and mPFS and mOS were 11 months and 45.9 months, respectively [4]. The results showed the anti-tumor activity of oral metronomic chemotherapy combined with targeted therapy. However, the two-drug combination chemotherapy of this scheme makes its toxic and side effects slightly serious, and adverse reactions such as grade 3 hand–foot syndrome and anemia can be observed. We explored the efficacy and safety of oral single-drug vinorelbine combined with trastuzumab (mNH) in the treatment of advanced breast cancer. Subgroup analysis showed that the ORR was 37.5%, CBR was 87.5%, and mPFS was 17.7 months. Although the effectiveness of the two regimens cannot be directly compared, the data show that mNH regimen is slightly better than HEX regimen in terms of CBR and mPFS. Most of the side effects were grade 1–2, and no grade 3 or above side effects were observed.
In a phase I study, researchers explored the safety dose-range of metronomic oral vinorelbine in advanced refractory cancer [18]. In that study, 62 patients were enrolled to receive six dose levels of oral metronomic vinorelbine from 20 to 70 mg thrice a week until disease progression, unacceptable toxicity, or withdrawal of consent. Unacceptable toxicity occurred in 2 patients at 60 mg (leukopenia grade 4 and epistaxis grade 2) and in 1 patient at 70 mg (leukopenia grade 2). Therefore, recommended dose of metronomic oral vinorelbine as a single agent was defined as 50 mg thrice a week. In another phase I trial, patients with metastatic breast cancer were enrolled to receive oral metronomic vinorelbine plus capecitabine, and the results showed that the dose-limiting toxicities of metronomic vinorelbine were 70 mg and recommended maximum tolerated doses (MTD) were 60 mg every other day [19]. In the phase I VICTOR-1 study, researchers also explored the MTD of oral metronomic vinorelbine combined with capecitabine the first time [20]. Patients with metastatic breast cancer received oral metronomic vinorelbine from 20 mg on Days 1–3–5 plus capecitabine fixed dose of 500 mg thrice a day, if no grade 3/4 toxicity was observed in the first 3 weeks, then the vinorelbine will be escalated by 10 mg/ days. The results showed that the MTD of oral metronomic vinorelbine was 40 mg thrice a week and was the recommended dose for phase II multicenter study. Our study also followed the recommended dose as 40 mg thrice a week.
HERNATA is a phase III clinical trial which compared the efficacy of vinorelbine plus trastuzumab with docetaxel plus trastuzumab in first-line treatment of HER2-positive MBC patients [14]. In the subgroup of vinorelbine plus trastuzumab of HERNATA study, patients naïve to chemotherapy for advanced disease received intravenous injection vinorelbine 30 to 35 mg/m2 on day 1 and 8 combined with trastuzumab (8 mg/kg loading dose and 6 mg/kg maintenance dose) on day 1 every 3 weeks as first-line therapy for metastatic breast cancer. The median time to progression (TTP) was 15.3 months, the median overall survival was 38.8 months. 13 (11.0%) patients got CR, 57 (48.3%) partial response, 19 (16.1%) stable disease, 6 (5.1%) progressive disease, and 23 (19.5%) not evaluable. Overall response rate (CR + PR) was 59.3%. Due to significant differences in sample size and study design, our results cannot be compared directly with the previous data. The mPFS of mNH in the first-line treatment of HER2-positive MBC in our study is 17.7 months (95%CI not reached), and the ORR of mNH in this population is 20%, which warrants further evaluation of mNH regimen in a larger sample size. Meanwhile, our primary results also indicated a possibility that metronomic chemotherapy plus trastuzumab may exert a modest and delayed anti-tumor activity, which may achieve comparable and even longer survival benefit compared with traditional intravenous chemotherapy in combination with trastuzumab.
In the present study, the mPFS of mNH reached 7.4 months (95%CI 3.2–11.5). For patients who received mNH as first-line therapy, the mPFS was 17.7 (95%CI: not reached), while the mPFS of patients who received mNH as more than 1 treatment line was 5.8 months (95%CI 5.6–5.9) (log rank p = 0.03). This result indicated that earlier administration of mNH regimen was associated with superior survival benefit compared to later exposure, which warrants further study to evaluate this regimen in earlier treatment lines for HER2-positive MBC patients.
Several studies have evaluated the efficacy of metronomic chemotherapy combined with anti-HER2 treatment. In the EORTC 75,111–10,114 phase II clinical trial, HER2-positive metastatic breast cancer patients without previous chemotherapy for metastatic disease were enrolled [21]. The trastuzumab and pertuzumab plus metronomic cyclophosphamide group prolonged the 6-month PFS rate than the dual HER2 blockade alone (73.4% vs 46.2%, p = 0.12). The mPFS of trastuzumab and pertuzumab plus metronomic cyclophosphamide regimen reached 12.7 months (95%CI 6.7–24.8), while the trastuzumab and pertuzumab alone group were 5.6 months (95%CI 3.6–16.8). The most common grade 3–4 side effects in the dual HER2 blockade plus cyclophosphamide group were hypertension (12%), diarrhea (12%), dyspnea (10%), fatigue (5%), pain (5%), and a thromboembolic event (10%). In another clinical trial, the median time to progression (mTTP) of trastuzumab combined with oral metronomic cyclophosphamide and methotrexate in HER2-positive metastatic breast cancer patients was 6 months (range from 0.7 to 18.4 months) [22]. Although different studies cannot be compared directly, our primary data showed promising mPFS in first-line HER2-positive metastatic breast cancer patients with limited toxicity, which brings a new option of metronomic regimen for HER2-positive MBC patients.
Subgroup analysis showed that there was no difference of mPFS between the hormone receptor-positive and receptor-negative group. While in the HERNATA study, hormone receptor status may be a marker for sensitivity to vinorelbine [14].
VELVET study explored the safety and efficacy of intravenous vinorelbine combined with dual anti-HER2 regimen [22]. The VELVET study results showed that the PFS of intravenous vinorelbine combined with pertuzumab and trastuzumab as first-line treatment of HER2-positive metastatic breast cancer patients was 14.3 months (95%CI 11.2–17.5). In our study, the mPFS for patients who received oral metronomic vinorelbine combined with trastuzumab as first-line therapy was 17.7 (95%CI: not reached). The above indicated that oral metronomic vinorelbine combined with anti-HER2 regimen was an efficacy treatment strategy.
In HERNATA study, grade 3 and 4 drug-related toxicities were observed included hematologic toxicities and nonhematologic toxicities [14]. However, in our study, we observed the most common side effects of metronomic vinorelbine combined with trastuzumab were grade 1 nausea (15%), leukopenia (15%), ALT/AST elevation (15%), diarrhea (10%), peripheral neuropathy (10%), constipation (5%), anemia (5%), cardiac toxicity (5%), increased creatine (5%), and insomnia (5%). Grade 2 adverse events included leukopenia (5%), neutropenia (10%). All of the advanced events were less than 3 degrees. Those side effects indicated that oral mNH combination is a very well-tolerated regimen, with modest side effects and high quality of life.
mNH regimen is economical, effective, and well tolerated. In low-income countries, it can be used as a treatment for HER2-positive breast cancer patients. At the same time, oral metronomic chemotherapy makes patients not hospitalized or reduce the length of stay (only because of targeted treatment), which provides convenience for patients in the global pandemic of diseases such as COVID-19.
However, the sample size enrolled in this clinical trial was limited. Besides, due to limited accessibility and insurance reimbursement of anti-HER2 drugs in china, no patients in this study received pertuzumab or ado-trastuzumab emtansine as previous anti-HER2 treatment. It is expected that large-scale phase III clinical trial will be carried out to verify the results of this trial.
Conclusions
To conclude, oral metronomic vinorelbine combined with trastuzumab is present with promising anti-tumor activity and is well-tolerated in previously treated HER2-positive metastatic breast cancer patients.
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30
Mukai H (2010) Treatment strategy for HER2-positive breast cancer. Int J Clin Oncol 15(4):335–340
Cazzaniga ME, Biganzoli L, Cortesi L, De Placido S, Donadio M, Fabi A, Ferro A, Generali D, Lorusso V, Milani A et al (2019) Treating advanced breast cancer with metronomic chemotherapy: what is known, what is new and what is the future? Onco Targets Ther 12:2989–2997
Orlando L, Lorusso V, Giotta F, Di Maio M, Schiavone P, Fedele P, Quaranta A, Caliolo C, Ciccarese M, Cinefra M et al (2020) Metronomic oral chemotherapy with cyclophosphamide plus capecitabine combined with trastuzumab (HEX) as first line therapy of HER-2 positive advanced breast cancer: a phase II trial of the Gruppo Oncologico Italia Meridionale (GOIM). Breast (Edinburgh, Scotland) 53:18–22
Harbeck N, Gnant M (2017) Breast cancer. Lancet (London, England) 389(10074):1134–1150
Gennari A, Stockler M, Puntoni M, Sormani M, Nanni O, Amadori D, Wilcken N, D’Amico M, DeCensi A, Bruzzi P (2011) Duration of chemotherapy for metastatic breast cancer: a systematic review and meta-analysis of randomized clinical trials. J Clin Oncol 29(16):2144–2149
Dellapasqua S, Bertolini F, Bagnardi V, Campagnoli E, Scarano E, Torrisi R, Shaked Y, Mancuso P, Goldhirsch A, Rocca A et al (2008) Metronomic cyclophosphamide and capecitabine combined with bevacizumab in advanced breast cancer. J Clin Oncol 26(30):4899–4905
Munzone E, Colleoni M (2015) Clinical overview of metronomic chemotherapy in breast cancer. Nat Rev Clin Oncol 12(11):631–644
Cazzaniga ME, Dionisio MR, Riva F (2017) Metronomic chemotherapy for advanced breast cancer patients. Cancer Lett 400:252–258
Browder T, Butterfield CE, Kräling BM, Shi B, Marshall B, O’Reilly MS, Folkman J (2000) Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Can Res 60(7):1878–1886
Banissi C, Ghiringhelli F, Chen L, Carpentier AF (2009) Treg depletion with a low-dose metronomic temozolomide regimen in a rat glioma model. Cancer Immunol Immunother CII 58(10):1627–1634
Orlando L, Cardillo A, Ghisini R, Rocca A, Balduzzi A, Torrisi R, Peruzzotti G, Goldhirsch A, Pietri E, Colleoni M (2006) Trastuzumab in combination with metronomic cyclophosphamide and methotrexate in patients with HER-2 positive metastatic breast cancer. BMC Cancer 6:225
Pegram MD, Konecny GE, O’Callaghan C, Beryt M, Pietras R, Slamon DJ (2004) Rational combinations of trastuzumab with chemotherapeutic drugs used in the treatment of breast cancer. J Natl Cancer Inst 96(10):739–749
Andersson M, Lidbrink E, Bjerre K, Wist E, Enevoldsen K, Jensen AB, Karlsson P, Tange UB, Sørensen PG, Møller S et al (2011) Phase III randomized study comparing docetaxel plus trastuzumab with vinorelbine plus trastuzumab as first-line therapy of metastatic or locally advanced human epidermal growth factor receptor 2-positive breast cancer: the HERNATA study. J Clin Oncol 29(3):264–271
Bergen E, Berghoff AS, Rudas M, Dubsky P, De Vries C, Sattlberger C, Mader RM, Zagouri F, Sparber C, Fitzal F et al (2014) Taxanes plus trastuzumab compared to oral vinorelbine plus trastuzumab in HER2-overexpressing metastatic breast cancer. Breast Care (Basel, Switzerland) 9(5):344–348
Fares JE, El Tomb P, Khalil LE, Atwani RW, Moukadem HA, Awada A, El Saghir NS (2020) Metronomic chemotherapy for patients with metastatic breast cancer: review of effectiveness and potential use during pandemics. Cancer Treat Rev 89:102066
André N, Carré M, Pasquier E (2014) Metronomics: towards personalized chemotherapy? Nat Rev Clin Oncol 11(7):413–431
Briasoulis E, Pappas P, Puozzo C, Tolis C, Fountzilas G, Dafni U, Marselos M, Pavlidis N (2009) Dose-ranging study of metronomic oral vinorelbine in patients with advanced refractory cancer. Clin Cancer Res 15(20):6454–6461
Saridaki Z, Malamos N, Kourakos P, Polyzos A, Ardavanis A, Androulakis N, Kalbakis K, Vamvakas L, Georgoulias V, Mavroudis D (2012) A phase I trial of oral metronomic vinorelbine plus capecitabine in patients with metastatic breast cancer. Cancer Chemother Pharmacol 69(1):35–42
Cazzaniga ME, Torri V, Villa F, Giuntini N, Riva F, Zeppellini A, Cortinovis D, Bidoli P (2014) Efficacy and safety of the all-oral schedule of metronomic vinorelbine and capecitabine in locally advanced or metastatic breast cancer patients: the phase I-II VICTOR-1 study. Int J Breast Cancer 2014:769790
Wildiers H, Tryfonidis K, Dal Lago L, Vuylsteke P, Curigliano G, Waters S, Brouwers B, Altintas S, Touati N, Cardoso F et al (2018) Pertuzumab and trastuzumab with or without metronomic chemotherapy for older patients with HER2-positive metastatic breast cancer (EORTC 75111–10114): an open-label, randomised, phase 2 trial from the Elderly Task Force/Breast Cancer Group. Lancet Oncol 19(3):323–336
Perez EA, López-Vega JM, Petit T, Zamagni C, Easton V, Kamber J, Restuccia E, Andersson M (2016) Safety and efficacy of vinorelbine in combination with pertuzumab and trastuzumab for first-line treatment of patients with HER2-positive locally advanced or metastatic breast cancer: VELVET Cohort 1 final results. Breast Cancer Res BCR 18(1):126
Acknowledgements
We thank the patients who participated in this study and their families. Thanks for Han yiqun in revising this paper.
Funding
There is no fund support for the research.
Author information
Authors and Affiliations
Contributions
ZJW: Assembly of data, Data analysis and interpretation, Manuscript writing, and Final approval of manuscript. JXL: Assembly of data, Manuscript writing, and Final approval of manuscript. FM: Assembly of data, Manuscript writing, and Final approval of manuscript. JYW: Assembly of data, Manuscript writing, and Final approval of manuscript. YL: Assembly of data, Manuscript writing, and Final approval of manuscript. YF: Assembly of data, Manuscript writing, and Final approval of manuscript. PY: Assembly of data, Manuscript writing, and Final approval of manuscript. PZ: Assembly of data, Manuscript writing, and Final approval of manuscript. QL: Assembly of data, Manuscript writing, and Final approval of manuscript. QL: Conception and design, Assembly of data, Data analysis and interpretation, Manuscript writing, and Final approval of manuscript. BHX: Conception and design, Assembly of data, Data analysis and interpretation, Manuscript writing, and Final approval of manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared no competing interests.
Ethical approval
The study was approved by the institutional review board of National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College. All patients provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Z., Liu, J., Ma, F. et al. Safety and efficacy study of oral metronomic vinorelbine combined with trastuzumab (mNH) in HER2-positive metastatic breast cancer: a phase II trial. Breast Cancer Res Treat 188, 441–447 (2021). https://doi.org/10.1007/s10549-021-06216-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06216-5