Abstract
Introduction
Triple negative breast cancer (TNBC) is an aggressive cancer subtype and lack of effective targeted therapies. It has been recently reported that Interleukin 17 (IL-17), a family of cytokines secreted in tumor microenvironment, affects tumor progression through a variety of molecular pathways. Its role in TNBC is so far still poorly explored.
Materials and methods
We employed immunohistochemistry to evaluate the distribution of IL-17+ cells in TNBC with no special type features (TNBC-NST), their association with tumor microangiogenesis, as well as their impact on prognosis of the patients.
Results
In comparison to medullary carcinoma with triple-negative molecular features (TNBC-MC), we found a significant increase in IL-17+ cell infiltrates in intratumoral stroma and extratumoral stroma of TNBC-NST. Similarly, stromal cells with co-expression of CD4 and IL-17 were noted in intratumoral and extratumoral stroma in both TNBC-NST and TNBC-MC. In addition, intratumoral IL-17+ cells were positively associated with tumor cell expression of vascular endothelial growth factor A (VEGFA) and with intratumoral tumor microvascular density (MVD). Multivariate analysis identified that intratumoral IL-17+ cells (P = 0.018), MVD (P = 0.039), and TNM stage (P = 0.002) were independent prognostic factors for predicting poor PFS.
Conclusion
The study indicates that IL-17 is overexpressed in intratumoral stromal cells of TNBC-NST. The overexpression of IL-17 might engage in active tumor microangiogenesis through its signal transduction pathways resulting in increased tumor secretion of VEGFA, and then promote tumor progression. IL-17 might serve as a potential new target for individualized therapy to TNBC-NST patients by development of specific antibodies. Additional study is deemed to further explore the role of IL-17+ stromal cells in breast cancer.




Similar content being viewed by others
References
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454 (7203):436–444. https://doi.org/10.1038/nature07205
Rosenberg SA, Spiess P, Lafreniere R (1986) A new approach to the adoptive immunotherapy of cancer with tumor-infiltrating lymphocytes. Science 233 (4770):1318–1321. https://doi.org/10.1126/science.3489291
Harrington LE, Hatton RD, Mangan PR, Turner H, Murphy TL, Murphy KM, Weaver CT (2005) Interleukin 17-producing CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat Immunol 6 (11):1123–1132. https://doi.org/10.1038/ni1254
Park H, Li Z, Yang XO, Chang SH, Nurieva R, Wang YH, Wang Y, Hood L, Zhu Z, Tian Q, Dong C (2005) A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat Immunol 6 (11):1133–1141. https://doi.org/10.1038/ni1261
He S, Fei M, Wu Y, Zheng D, Wan D, Wang L, Li D (2011) Distribution and clinical significance of Th17 cells in the tumor microenvironment and peripheral blood of pancreatic cancer patients. Int J Mol Sci 12 (11):7424–7437. https://doi.org/10.3390/ijms12117424
Su X, Ye J, Hsueh EC, Zhang Y, Hoft DF, Peng G (2010) Tumor microenvironments direct the recruitment and expansion of human Th17 cells. J Immunol 184 (3):1630–1641. https://doi.org/10.4049/jimmunol.0902813
Yang L, Qi Y, Hu J, Tang L, Zhao S, Shan B (2012) Expression of Th17 cells in breast cancer tissue and its association with clinical parameters. Cell Biochem Biophys 62 (1):153–159. https://doi.org/10.1007/s12013-011-9276-3
Jain P, Javdan M, Feger FK, Chiu PY, Sison C, Damle RN, Bhuiya TA, Sen F, Abruzzo LV, Burger JA, Rosenwald A, Allen SL, Kolitz JE, Rai KR, Chiorazzi N, Sherry B (2012) Th17 and non-Th17 interleukin-17-expressing cells in chronic lymphocytic leukemia: delineation, distribution, and clinical relevance. Haematologica 97 (4):599–607. https://doi.org/10.3324/haematol.2011.047316
Punt S, Fleuren GJ, Kritikou E, Lubberts E, Trimbos JB, Jordanova ES, Gorter A (2015) Angels and demons: Th17 cells represent a beneficial response, while neutrophil IL-17 is associated with poor prognosis in squamous cervical cancer. Oncoimmunology 4 (1):e984539. https://doi.org/10.4161/2162402X.2014.984539
Tesmer LA, Lundy SK, Sarkar S, Fox DA (2008) Th17 cells in human disease. Immunol Rev 223:87–113. https://doi.org/10.1111/j.1600-065X.2008.00628.x
Wang B, Li L, Liao Y, Li J, Yu X, Zhang Y, Xu J, Rao H, Chen S, Zhang L, Zheng L (2013) Mast cells expressing interleukin 17 in the muscularis propria predict a favorable prognosis in esophageal squamous cell carcinoma. Cancer Immunol Immunother 62 (10):1575–1585. https://doi.org/10.1007/s00262-013-1460-4
Yang B, Kang H, Fung A, Zhao H, Wang T, Ma D (2014) The role of interleukin 17 in tumour proliferation, angiogenesis, and metastasis. Mediat Inflamm 2014:623759. https://doi.org/10.1155/2014/623759
Ye J, Livergood RS, Peng G (2013) The role and regulation of human Th17 cells in tumor immunity. Am J Pathol 182 (1):10–20. https://doi.org/10.1016/j.ajpath.2012.08.041
Murugaiyan G, Saha B (2009) Protumor vs antitumor functions of IL-17. J Immunol 183 (7):4169–4175. https://doi.org/10.4049/jimmunol.0901017
Liu J, Duan Y, Cheng X, Chen X, Xie W, Long H, Lin Z, Zhu B (2011) IL-17 is associated with poor prognosis and promotes angiogenesis via stimulating VEGF production of cancer cells in colorectal carcinoma. Biochem Biophys Res Commun 407 (2):348–354. https://doi.org/10.1016/j.bbrc.2011.03.021
Du JW, Xu KY, Fang LY, Qi XL (2012) Interleukin-17, produced by lymphocytes, promotes tumor growth and angiogenesis in a mouse model of breast cancer. Mol Med Rep 6 (5):1099–1102. https://doi.org/10.3892/mmr.2012.1036
Bianchini G, Balko JM, Mayer IA, Sanders ME, Gianni L (2016) Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol 13 (11):674–690. https://doi.org/10.1038/nrclinonc.2016.66
Irvin WJ Jr, Carey LA (2008) What is triple-negative breast cancer? Eur J Cancer 44 (18):2799–2805. https://doi.org/10.1016/j.ejca.2008.09.034
Ribatti D, Nico B, Ruggieri S, Tamma R, Simone G, Mangia A (2016) Angiogenesis and antiangiogenesis in triple-negative breast cancer. Transl Oncol 9 (5):453–457. https://doi.org/10.1016/j.tranon.2016.07.002
Demaria S, Volm MD, Shapiro RL, Yee HT, Oratz R, Formenti SC, Muggia F, Symmans WF (2001) Development of tumor-infiltrating lymphocytes in breast cancer after neoadjuvant paclitaxel chemotherapy. Clin Cancer Res 7 (10):3025–3030
Stephenson TJ (2000) Diagnostic surgical pathology, 3rd edn. Lippincott Williams & Wilkins, Philadelphia. https://doi.org/10.1136/jcp.53.10.804
Wu Y, Kyle-Cezar F, Woolf RT, Naceur-Lombardelli C, Owen J, Biswas D, Lorenc A, Vantourout P, Gazinska P, Grigoriadis A, Tutt A, Hayday A (2019) An innate-like Vdelta1 (+) gammadelta T cell compartment in the human breast is associated with remission in triple-negative breast cancer. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aax9364
Yang M, Bao W, Zhang X, Kang Y, Haffty B, Zhang L (2017) Short-term and long-term clinical outcomes of uncommon types of invasive breast cancer. Histopathology 71 (6):874–886. https://doi.org/10.1111/his.13328
Lim KH, Telisinghe PU, Abdullah MS, Ramasamy R (2010) Possible significance of differences in proportions of cytotoxic T cells and B-lineage cells in the tumour-infiltrating lymphocytes of typical and atypical medullary carcinomas of the breast. Cancer Immun 10:3
Ridolfi RL, Rosen PP, Port A, Kinne D, Mike V (1977) Medullary carcinoma of the breast: a clinicopathologic study with 10 year follow-up. Cancer 40 (4):1365–1385. https://doi.org/10.1002/1097-0142(197710)40:4%3c1365:aid-cncr2820400402%3e3.0.co;2-n
Guo X, Fan Y, Lang R, Gu F, Chen L, Cui L, Pringle GA, Zhang X, Fu L (2008) Tumor infiltrating lymphocytes differ in invasive micropapillary carcinoma and medullary carcinoma of breast. Mod Pathol 21 (9):1101–1107. https://doi.org/10.1038/modpathol.2008.72
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S, International TWG (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26 (2):259–271. https://doi.org/10.1093/annonc/mdu450
Weidner N (1995) Current pathologic methods for measuring intratumoral microvessel density within breast carcinoma and other solid tumors. Breast Cancer Res Treat 36 (2):169–180. https://doi.org/10.1007/bf00666038
Chen JG, Xia JC, Liang XT, Pan K, Wang W, Lv L, Zhao JJ, Wang QJ, Li YQ, Chen SP, He J, Huang LX, Ke ML, Chen YB, Ma HQ, Zeng ZW, Zhou ZW, Chang AE, Li Q (2011) Intratumoral expression of IL-17 and its prognostic role in gastric adenocarcinoma patients. Int J Biol Sci 7 (1):53–60. https://doi.org/10.7150/ijbs.7.53
Benevides L, da Fonseca DM, Donate PB, Tiezzi DG, De Carvalho DD, de Andrade JM, Martins GA, Silva JS (2015) IL17 Promotes mammary tumor progression by changing the behavior of tumor cells and eliciting tumorigenic neutrophils recruitment. Cancer Res 75 (18):3788–3799. https://doi.org/10.1158/0008-5472.CAN-15-0054
Laprevotte E, Cochaud S, dusManoir S, Lapierre M, Dejou C, Philippe M, Giustiniani J, Frewer KA, Sanders AJ, Jiang WG, Michaud HA, Colombo PE, Bensussan A, Alberici G, Bastid J, Eliaou JF, Bonnefoy N (2017) The IL-17B-IL-17 receptor B pathway promotes resistance to paclitaxel in breast tumors through activation of the ERK1/2 pathway. Oncotarget 8 (69), 113360–113372. https://doi.org/10.18632/oncotarget.23008
Mohammed RA, Ellis IO, Mahmmod AM, Hawkes EC, Green AR, Rakha EA, Martin SG (2011) Lymphatic and blood vessels in basal and triple-negative breast cancers: characteristics and prognostic significance. Mod Pathol 24 (6):774–785. https://doi.org/10.1038/modpathol.2011.4
Linderholm BK, Hellborg H, Johansson U, Elmberger G, Skoog L, Lehtio J, Lewensohn R (2009) Significantly higher levels of vascular endothelial growth factor (VEGF) and shorter survival times for patients with primary operable triple-negative breast cancer. Ann Oncol 20 (10):1639–1646. https://doi.org/10.1093/annonc/mdp062
Fabre JAS, Giustinniani J, Garbar C, Merrouche Y, Antonicelli F, Bensussan A (2018) The interleukin-17 family of cytokines in breast cancer. Int J Mol Sci. https://doi.org/10.3390/ijms19123880
Funding
We thank the grant support from National Natural Science Foundation of China (Grant No. 81772840) to Xiao-Jing Guo.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Xiao-Long Qian, Peng Xu, Yi-Qian Zhang, Yuan-Ming Song, Ya-Qing Li, Wei-Dong Li, Cheng-Ying Jiang, Bei-Bei Shen , Xin-Min Zhang, Li-Na Zhang, Li Fu, and Xiao-Jing Guo declares that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2020_5540_MOESM4_ESM.tif
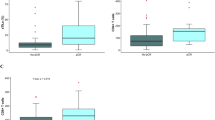
Fig. S1 Distribution of IL-17+ and CD4+ cells in different parts of stroma of TNBC-NST and TNBC-MC (Local amplifications). a Intratumoral IL-17+ cells in TNBC-NST; b Intratumoral CD4+ cells in TNBC-NST; c Peritumoral IL-17+ cells in TNBC-NST; d Peritumoral CD4+ cells in TNBC-NST; e Extratumoral IL-17+ cells in TNBC-NST; f Extratumoral CD4+ cells in TNBC-NST; g Intratumoral IL-17+ cells in TNBC-MC; h Intratumoral CD4+ cells in TNBC-MC; i Peritumoral IL-17+ cells in TNBC-MC; j Peritumoral CD4+ cells in TNBC-MC; k Extratumoral IL-17+ cells in TNBC-MC; l Extratumoral CD4+ cells in TNBC-MC. Supplementary file4 (TIF 5244 kb)
10549_2020_5540_MOESM5_ESM.tif
Fig. S2 The effect of IL-17+ cell appearance on the prognosis of TNBC-NST. a The effect of IL-17+ cell appearance on progression-free survival (PFS); b The effect of IL-17+ cell appearance on overall survival (OS). Supplementary file5 (TIF 1211 kb)
Rights and permissions
About this article
Cite this article
Qian, XL., Xu, P., Zhang, YQ. et al. Increased number of intratumoral IL-17+ cells, a harbinger of the adverse prognosis of triple-negative breast cancer. Breast Cancer Res Treat 180, 311–319 (2020). https://doi.org/10.1007/s10549-020-05540-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05540-6