Abstract
Purpose
40% of triple-negative breast cancer (TNBC) do not express claudin-1, a major constituent of tight junction. Patients with these “claudin-1-low” tumors present a higher relapse incidence. A major challenge in oncology is the development of innovative therapies for such poor prognosis tumors. In this context, we study the anticancer effects of ∆2-TGZ, a compound derived from troglitazone (TGZ), on cell models of these tumors.
Methods and results
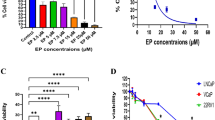
In MDA-MB-231 and Hs578T “claudin-1-low” TNBC cells, Δ2-TGZ treatment induced claudin-1 protein expression and triggered apoptosis as measured by FACS analysis (annexin V/PI co-staining). Interestingly, in the non-tumorigenic human breast epithelial cell line MCF-10A, the basal level of claudin-1 was not modified following Δ2-TGZ treatment, which did not induce apoptosis. Furthermore, claudin-1-transfected MDA-MB-231 and Hs578T cells displayed a significant increase of cleaved PARP-1 and caspase 7, caspase 3/7 activities, and TUNEL staining. RNA interference was performed in order to inhibit Δ2-TGZ-induced claudin-1 expression in both the cells. In absence of claudin-1, a decrease of cleaved PARP-1 and caspase 7 and caspase 3/7 activities were observed in MDA-MB-231 but not in Hs578T cells.
Conclusion
Claudin-1 overexpression and Δ2-TGZ treatment are associated to apoptosis in MDA-MB-231 and Hs578T “claudin-1-low” TNBC. Moreover, in MDA-MB-231 cells, claudin-1 is involved in the pro-apoptotic effect of Δ2-TGZ. Our results suggest that claudin-1 re-expression could be an interesting therapeutic strategy for “claudin-1-low” TNBC.





Similar content being viewed by others
Change history
31 July 2017
An erratum to this article has been published.
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2012) GLOBOCAN 2012 v1.0, Cancer incidence and mortality worldwide: IARC CancerBase No. 11. In: Lyon, France: International Agency for Research on Cancer; 2013
Foulkes WD, Smith IE, Reis-Filho JS (2010) Triple-negative breast cancer. N Engl J Med 363:1938–1948. doi:10.1056/NEJMra1001389
Zardavas D, Tryfonidis K, Goulioti T, Piccart M (2016) Targeted adjuvant therapy in breast cancer. Expert Rev Anticancer Ther. doi:10.1080/14737140.2016.1247698
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MC, Nielsen TO, Moorman PG, Earp HS, Millikan RC (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502. doi:10.1001/jama.295.21.2492
Lu S, Singh K, Mangray S, Tavares R, Noble L, Resnick MB, Yakirevich E (2013) Claudin expression in high-grade invasive ductal carcinoma of the breast: correlation with the molecular subtype. Mod Pathol 26:485–495. doi:10.1038/modpathol.2012.187
Tokes AM, Kulka J, Paku S, Szik A, Paska C, Novak PK, Szilak L, Kiss A, Bogi K, Schaff Z (2005) Claudin-1, -3 and -4 proteins and mRNA expression in benign and malignant breast lesions: a research study. Breast Cancer Res 7:R296–R305. doi:10.1186/bcr983
Morohashi S, Kusumi T, Sato F, Odagiri H, Chiba H, Yoshihara S, Hakamada K, Sasaki M, Kijima H (2007) Decreased expression of claudin-1 correlates with recurrence status in breast cancer. Int J Mol Med 20:139–143
Szasz AM, Tokes AM, Micsinai M, Krenacs T, Jakab C, Lukacs L, Nemeth Z, Baranyai Z, Dede K, Madaras L, Kulka J (2011) Prognostic significance of claudin expression changes in breast cancer with regional lymph node metastasis. Clin Exp Metastasis 28:55–63. doi:10.1007/s10585-010-9357-5
Ma F, Ding X, Fan Y, Ying J, Zheng S, Lu N, Xu B (2014) A CLDN1-negative phenotype predicts poor prognosis in triple-negative breast cancer. PLoS ONE 9:e112765. doi:10.1371/journal.pone.0112765
Furuse M, Sasaki H, Fujimoto K, Tsukita S (1998) A single gene product, claudin-1 or -2, reconstitutes tight junction strands and recruits occludin in fibroblasts. J Cell Biol 143:391–401
Saitou M, Fujimoto K, Doi Y, Itoh M, Fujimoto T, Furuse M, Takano H, Noda T, Tsukita S (1998) Occludin-deficient embryonic stem cells can differentiate into polarized epithelial cells bearing tight junctions. J Cell Biol 141:397–408
Zhou B, Moodie A, Blanchard AA, Leygue E, Myal Y (2015) Claudin 1 in breast cancer: new insights. J Clin Med 4:1960–1976. doi:10.3390/jcm4121952
Zhang K, Yao HP, Wang MH (2008) Activation of RON differentially regulates claudin expression and localization: role of claudin-1 in RON-mediated epithelial cell motility. Carcinogenesis 29:552–559. doi:10.1093/carcin/bgn003
Kulawiec M, Safina A, Desouki MM, Still I, Matsui S, Bakin A, Singh KK (2008) Tumorigenic transformation of human breast epithelial cells induced by mitochondrial DNA depletion. Cancer Biol Ther 7:1732–1743
Hoevel T, Macek R, Swisshelm K, Kubbies M (2004) Reexpression of the TJ protein CLDN1 induces apoptosis in breast tumor spheroids. Int J Cancer 108:374–383. doi:10.1002/ijc.11571
Akasaka H, Sato F, Morohashi S, Wu Y, Liu Y, Kondo J, Odagiri H, Hakamada K, Kijima H (2010) Anti-apoptotic effect of claudin-1 in tamoxifen-treated human breast cancer MCF-7 cells. BMC Cancer 10:548. doi:10.1186/1471-2407-10-548
Liu Y, Wang L, Lin XL, Wang J, Yu JH, Miao Y, Wang EH (2012) Anti-apoptotic effect of claudin-1 on TNF-a-induced apoptosis in human breast cancer MCF-7. Tumor Biol 33:2307–2315
Zhou B, Blanchard A, Wang N, Ma X, Han J, Schroedter I, Leygue E, Myal Y (2015) Claudin 1 promotes migration and increases sensitivity to tamoxifen and anticancer drugs in luminal-like human breast cancer cells MCF7. Cancer Invest 33:429–439. doi:10.3109/07357907.2015.1060996
Frohlich E, Wahl R (2015) Chemotherapy and chemoprevention by thiazolidinediones. Biomed Res Int 2015:845340. doi:10.1155/2015/845340
Home PD, Pocock SJ, Beck-Nielsen H, Curtis PS, Gomis R, Hanefeld M, Jones NP, Komajda M, McMurray JJ (2009) Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicentre, randomised, open-label trial. Lancet 373:2125–2135. doi:10.1016/S0140-6736(09)60953-3
Monami M, Lamanna C, Marchionni N, Mannucci E (2008) Rosiglitazone and risk of cancer: a meta-analysis of randomized clinical trials. Diabetes Care 31:1455–1460. doi:10.2337/dc07-2308
Mueller E, Smith M, Sarraf P, Kroll T, Aiyer A, Kaufman DS, Oh W, Demetri G, Figg WD, Zhou XP, Eng C, Spiegelman BM, Kantoff PW (2000) Effects of ligand activation of peroxisome proliferator-activated receptor gamma in human prostate cancer. Proc Natl Acad Sci USA 97:10990–10995. doi:10.1073/pnas.180329197
Prost S, Relouzat F, Spentchian M, Ouzegdouh Y, Saliba J, Massonnet G, Beressi JP, Verhoeyen E, Raggueneau V, Maneglier B, Castaigne S, Chomienne C, Chretien S, Rousselot P, Leboulch P (2015) Erosion of the chronic myeloid leukaemia stem cell pool by PPAR gamma agonists. Nature. doi:10.1038/nature15248
Chojkier M (2005) Troglitazone and liver injury: in search of answers. Hepatology 41:237–246. doi:10.1002/hep.20567
Salamone S, Colin C, Grillier-Vuissoz I, Kuntz S, Mazerbourg S, Flament S, Martin H, Richert L, Chapleur Y, Boisbrun M (2012) Synthesis of new troglitazone derivatives: anti-proliferative activity in breast cancer cell lines and preliminary toxicological study. Eur J Med Chem 51:206–215. doi:10.1016/j.ejmech.2012.02.044
Lecomte J, Flament S, Salamone S, Boisbrun M, Mazerbourg S, Chapleur Y, Grillier-Vuissoz I (2008) Disruption of ERalpha signalling pathway by PPARgamma agonists: evidences of PPARgamma-independent events in two hormone-dependent breast cancer cell lines. Breast Cancer Res Treat 112:437–451. doi:10.1007/s10549-007-9886-z
Colin C, Salamone S, Grillier-Vuissoz I, Boisbrun M, Kuntz S, Lecomte J, Chapleur Y, Flament S (2010) New troglitazone derivatives devoid of PPARgamma agonist activity display an increased antiproliferative effect in both hormone-dependent and hormone-independent breast cancer cell lines. Breast Cancer Res Treat 124:101–110. doi:10.1007/s10549-009-0700-y
Colin-Cassin C, Yao X, Cerella C, Chbicheb S, Kuntz S, Mazerbourg S, Boisbrun M, Chapleur Y, Diederich M, Flament S, Grillier-Vuissoz I (2015) PPARgamma-inactive Delta2-troglitazone independently triggers ER stress and apoptosis in breast cancer cells. Mol Carcinog 54:393–404. doi:10.1002/mc.22109
Di Cello F, Cope L, Li H, Jeschke J, Wang W, Baylin SB, Zahnow CA (2013) Methylation of the claudin 1 promoter is associated with loss of expression in estrogen receptor positive breast cancer. PLoS ONE 8:e68630. doi:10.1371/journal.pone.0068630
Ogasawara N, Kojima T, Go M, Ohkuni T, Koizumi J, Kamekura R, Masaki T, Murata M, Tanaka S, Fuchimoto J, Himi T, Sawada N (2010) PPARgamma agonists upregulate the barrier function of tight junctions via a PKC pathway in human nasal epithelial cells. Pharmacol Res 61(6):489–498. doi:10.1016/j.phrs.2010.03.002
Varley CL, Garthwaite MA, Cross W, Hinley J, Trejdosiewicz LK, Southgate J (2006) PPARgamma-regulated tight junction development during human urothelial cytodifferentiation. J Cell Physiol 208:407–417. doi:10.1002/jcp.20676
Kumei S, Motomura W, Yoshizaki T, Takakusaki K, Okumura T (2009) Troglitazone increases expression of E-cadherin and claudin 4 in human pancreatic cancer cells. Biochem Biophys Res Commun 380:614–619. doi:10.1016/j.bbrc.2009.01.134
Okumura T (2010) Mechanisms by which thiazolidinediones induce anti-cancer effects in cancers in digestive organs. J Gastroenterol 45:1097–1102. doi:10.1007/s00535-010-0310-9
Beeman N, Webb PG, Baumgartner HK (2012) Occludin is required for apoptosis when claudin-claudin interactions are disrupted. Cell Death Dis 3:e273. doi:10.1038/cddis.2012.14
Fortier AM, Asselin E, Cadrin M (2013) Keratin 8 and 18 loss in epithelial cancer cells increases collective cell migration and cisplatin sensitivity through claudin1 up-regulation. J Biol Chem 288:11555–11571. doi:10.1074/jbc.M112.428920
Acknowledgements
This work was supported by grants of the “Université de Lorraine,” the “Conseil Régional du Grand Est,” and the “Ligue Contre le Cancer.” Marine Geoffroy was recipient of a PhD grant of the «Ministère de l’Enseignement Supérieur et de la Recherche». We thank Christelle Thibault-Carpentier and Doulaye Dembele from the IGBMC GenomEast platform for the GEO deposit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
The original version of this article was revised: The given and family names of the authors were swapped. The corrected author group was updated in the article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2017_4378_MOESM2_ESM.pptx
Supplementary data. 1 Changes in expression level of genes related to cell adhesion and associated with cancer progression in Δ2-TGZ-treated MCF-7 cells after microarray analysis. Cells were treated for 12 h with DMSO or 25 µM of Δ2-TGZ Gene-expression microarray data were generated using GeneChip Human Gene 1.0 ST Array (containing 764,885 distinct probes including 28,869 well-annotated genes) as previously described [28]. Microarray data are available from Geo Data set (https://www.ncbi.nlm.nih.gov/geo/info/linking.html, accession number GSE99941). Supplementary material 2 (PPTX 39 kb)
10549_2017_4378_MOESM3_ESM.pptx
Supplementary data. 2 Claudin-1 and occludin co-localization in response to Δ2-TGZ in MDA-MB-231 and Hs578T cells. After treatment for 24 h with DMSO (Ctrl) or 20 µM of Δ2-TGZ, immunofluorescence staining for claudin-1 and occludin were performed in MDA-MB-231 and Hs578T cells. DRAQ5 staining was used for visualisation of the nuclei. a–b Cells were observed by confocal microscopy with magnification from ×400 for Hs578T to ×536 for MDA-MB-231 depending of digital confocal zooming combine with ×40 objective (NA 0.8). One confocal z section of cell of each condition is presented. Claudin-1 staining is upregulated and punctiform in both cell lines. Occludin staining is upregulated only in MDA-MB-231 cells and colocalized with claudin-1. Bar represents 50 µm. Supplementary material 3 (PPTX 2351 kb)
10549_2017_4378_MOESM4_ESM.pptx
Supplementary data. 3 Increase apoptosis in MDA-MB-231 cells overexpressing claudin-1 with Δ2-TGZ. MDA-MB-231 cells were transiently transfected with pcDNA3.1 or pcDNA3.1 containing a human claudin-1 expression vector (pcDNA3.1-CLDN1) and treated with 20 µM of Δ2-TGZ. After 48 h of transfection and 24 h of treatment, cells were subjected to western blot analysis. a Western blot analysis was performed with antibodies recognizing claudin-1 (CLDN1) cleaved PARP-1 and cleaved caspase 7. α-tubulin was used as loading control. b Relative protein level corresponds to claudin-1, cleaved PARP-1 (PARP) and cleaved caspase 7 band intensity value adjusted to α-tubulin for Δ2-pcDNA3.1 and Δ2-pcDNA3.1-CLDN1. The values represent the mean ± SEM 5 different experiments. Student-t test was used to determine significance difference from control cells, were *p < 0.05, **p < 0.01 and ***p < 0.001. Supplementary material 4 (PPTX 3130 kb)
Rights and permissions
About this article
Cite this article
Geoffroy, M., Kleinclauss, A., Grandemange, S. et al. Pro-apoptotic effect of Δ2-TGZ in “claudin-1-low” triple-negative breast cancer cells: involvement of claudin-1. Breast Cancer Res Treat 165, 517–527 (2017). https://doi.org/10.1007/s10549-017-4378-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4378-2