Abstract
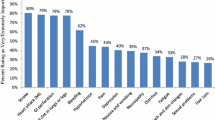
Perceptions among women with breast cancer about the relative importance of different potential chemotherapy side effects is not well understood. A survey was performed by women receiving chemotherapy for breast cancer. Grade I/II (mild to moderate) and III/IV (moderate to severe) descriptions of nine common chemotherapy side effects were assigned preference weights using the standard gamble technique. For each hypothetical side effect, patients could choose to stay in the respective side effect state or take a gamble between full health (probability p) or being dead (1 − p). For each side effect, p was varied until the patient was indifferent between these options. The survey also included questions about the importance of survival, slowing cancer growth, and quality of life. This analysis included 69 patients; mean age 54 years (range 35–84), representing all cancer stages. Standard gamble preferences were lowest (i.e., least preferred) for grade III/IV nausea/vomiting (0.621), indicating that patients would, on average, risk a 38 % chance of being dead to avoid having grade III/IV nausea/vomiting for the rest of their lives. The next least preferred side effects were grade III/IV diarrhea (0.677) and grade III/IV sensory neuropathy (0.694). Survival appeared more important than slowing cancer growth and maintaining quality of life across cancer stages. Nevertheless, patients with advanced disease placed less importance on survival (p = 0.09) and higher importance on quality of life (p = 0.05). These standard gamble utilities provide unique insights into chemotherapy toxicities from the patient perspective. Differences in the relative importance of overall survival and quality of life with treatment existed between patients with different stages of disease. These studies should be expanded as the data may also be used to calculate quality-adjusted life expectancy in cost-effectiveness evaluations of breast cancer chemotherapies.



Similar content being viewed by others
References
Jansen SJ, Stiggelbout AM, Wakker PP, Vliet Vlieland TP, Leer JW, Nooy MA, Kievit J (1998) Patients’ utilities for cancer treatments: a study of the chained procedure for the standard gamble and time tradeoff. Med Decis Mak 18(4):391–399
Chao C, Studts JL, Abell T, Hadley T, Roetzer L, Dineen S, Lorenz D, YoussefAgha A, McMasters KM (2003) Adjuvant chemotherapy for breast cancer: how presentation of recurrence risk influences decision-making. J Clin Oncol 21(23):4299–4305. doi:10.1200/jco.2003.06.025
Brazier J, Deverill M (1998) The use of health-related quality of life instruments in economic evaluation in health services research methods. A guide to best practice. BMJ Books, London
Torrance GW (1986) Measurement of health state utilities for economic appraisal. J Health Econ 5(1):1–30
Drummond MF, Iglesias CP, Cooper NJ (2008) Systematic reviews and economic evaluations conducted for the National Institute for Health and Clinical Excellence in the United Kingdom: a game of two halves? Int J Technol Assess Health Care 24(2):146–150. doi:10.1017/s0266462308080203
Cheng TF, Wang JD, Uen WC (2012) Cost-utility analysis of adjuvant goserelin (Zoladex) and adjuvant chemotherapy in premenopausal women with breast cancer. BMC Cancer 12:33. doi:10.1186/1471-2407-12-33
Melnikow J, Birch S, Slee C, McCarthy TJ, Helms LJ, Kuppermann M (2008) Tamoxifen for breast cancer risk reduction: impact of alternative approaches to quality-of-life adjustment on cost-effectiveness analysis. Med Care 46(9):946–953. doi:10.1097/MLR.0b013e318179250f
Mansel R, Locker G, Fallowfield L, Benedict A, Jones D (2007) Cost-effectiveness analysis of anastrozole vs tamoxifen in adjuvant therapy for early stage breast cancer in the United Kingdom: the 5-year completed treatment analysis of the ATAC (‘arimidex’, tamoxifen alone or in combination) trial. Br J Cancer 97(2):152–161. doi:10.1038/sj.bjc.6603804
Lloyd A, Nafees B, Narewska J, Dewilde S, Watkins J (2006) Health state utilities for metastatic breast cancer. Br J Cancer 95(6):683–690. doi:10.1038/sj.bjc.6603326
Brown RE, Hutton J, Burrell A (2001) Cost effectiveness of treatment options in advanced breast cancer in the UK. Pharmacoeconomics 19(11):1091–1102
Beusterien K, Grinspan J, Tencer T, Brufsky A, Visovsky C (2012) Patient preferences for chemotherapies used in breast cancer. Int J Women’s Health 4:279–287. doi:10.2147/ijwh.s31331
Furlong W, Feeney D, Torrance G (1990) Guide to design and development of health state utility instrumentation. Center for Health Economics Policy Analysis Working Paper Series. Hamilton (Ontario): McMaster University Paper No. 90-9
Beusterien K, Leigh N, Jackson C, Miller R, Mayo K, Revicki D (2005) Integrating preferences into health status assessment for amyotrophic lateral sclerosis: the ALS Utility Index. Amyotroph Lateral Scler Other Motor Neuron disord 6(3):169–176. doi:10.1080/14660820410021339
Fu AZ, Kattan MW (2008) Utilities should not be multiplied: evidence from the preference-based scores in the United States. Med Care 46(9):984–990. doi:10.1097/MLR.0b013e3181791a9c
Sun CC, Bodurka DC, Weaver CB, Rasu R, Wolf JK, Bevers MW, Smith JA, Wharton JT, Rubenstein EB (2005) Rankings and symptom assessments of side effects from chemotherapy: insights from experienced patients with ovarian cancer. Support Care Cancer 13(4):219–227. doi:10.1007/s00520-004-0710-6
Griffin AM, Butow PN, Coates AS, Childs AM, Ellis PM, Dunn SM, Tattersall MH (1996) On the receiving end. V: patient perceptions of the side effects of cancer chemotherapy in 1993. Ann Oncol 7(2):189–195
Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM, Tattersall MH (1983) On the receiving end–patient perception of the side-effects of cancer chemotherapy. Eur J Cancer Clin Oncol 19(2):203–208
Lindley C, McCune JS, Thomason TE, Lauder D, Sauls A, Adkins S, Sawyer WT (1999) Perception of chemotherapy side effects cancer versus noncancer patients. Cancer Pract 7(2):59–65
Chang WT, Collins ED, Kerrigan CL (2001) An internet-based utility assessment of breast hypertrophy. Plast Reconstr Surg 108(2):370–377
Acknowledgments
We would like to thank all the patients and their families for their help with this project. Funding for this study was received in the form of an unrestricted educational Grant from Eisai Pharmaceuticals.
Conflict of interest
Susan Dent—speaking honoraria (Eisai). There is no conflict of interest for the other authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuchuk, I., Bouganim, N., Beusterien, K. et al. Preference weights for chemotherapy side effects from the perspective of women with breast cancer. Breast Cancer Res Treat 142, 101–107 (2013). https://doi.org/10.1007/s10549-013-2727-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2727-3