Abstract
HIV transmission in Ukraine is driven in part by unsafe injection drug use and sexual risk behaviors among people who inject drugs. We performed a random-intercept latent transition analysis on responses to 9 binary injection drug use and sexual behavior items from 1195 people who inject drugs with negative HIV status enrolled in a clustered randomized clinical trial of a social network intervention in Odessa, Donetsk, and Nikolayev, Ukraine. We identified 5 baseline classes: “Social injection/equipment-sharing” (11.7%), “Social injection” (25.9%), “High-risk collective preparation/splitting” (17.0%), “Collective preparation/splitting” (11.3%), and “Dealer-facilitated injection” (34.1%). After 12 months, intervention participants were more likely to transition to the “Collective preparation/splitting” class, which featured the fewest risk behaviors. Transitioning from the “Collective preparation/splitting” to the “Social injection/equipment-sharing” class was associated with HIV acquisition for control participants. Research to illuminate the stability of these patterns and how they may benefit from uniquely tailored programming to reduce unsafe behaviors is needed.
Similar content being viewed by others
Introduction
There are an estimated 16 million people who inject drugs (PWID) across 179 countries and territories worldwide [1]. Injection drug use (IDU) behaviors can facilitate exposure to blood-borne infections through the sharing of unsterile injection drug equipment [2, 3]. In 2013, over 10 million disability-adjusted life years were attributable to IDU via exposure to HIV and hepatitis-B and C viruses [4]. Condomless sex between PWID exacerbates the spread of these infections in this population, while condomless sex between PWID and people who do not inject drugs contributes to the spread of these infections to non-injecting populations [5, 6].
Intertwining IDU and sexual behaviors such as these undergird risk for HIV in Ukraine, a former Soviet republic in Eastern Europe with a PWID-population of roughly 350,000 [7]. Ukraine has the second-highest HIV incidence rate (39.0/100,000 in 2019) among the 53 countries comprising the WHO European Region [8]. War with neighboring Russia, which has the highest HIV incidence rate in the WHO European Region, undermines HIV prevention efforts, further exacerbating HIV transmission risk [9]. Ukraine’s HIV epidemic, initially driven by unsafe injection behaviors, is now driven by condomless heterosexual sex [10, 11], though this is believed to involve sex predominantly between PWID and those who do not inject drugs [12].
Social network interventions have been effective in reducing unsafe IDU and sexual risk behaviors among PWID in Ukraine and elsewhere [3, 13,14,15,16,17,18,19,20,21,22,23]. One intervention recently tested in Ukraine trained PWID to influence the injection and sexual practices of their injection network members [24]. While this trial found reduced hazard for HIV acquisition among intervention participants, HIV incidence was high in both groups, indicating the intervention was successful in reducing risk behavior among some but not all those exposed to it [24]. However, further investigation to assess risk behavior-reduction was not conducted and merits investigation.
Various IDU behaviors (e.g., injection with used needles; injection with collectively prepared solution or solution that was split with other PWID) increase HIV transmission risk, and PWID engage in distinct sets of these behaviors [25,26,27]. Prior studies in the United States (US) and Middle East have found three to four patterns of IDU behaviors (or IDU and sexual risk behaviors) among local PWID populations, with various equipment-sharing, social injection, and sexual behaviors emerging in distinct clusters [25,26,27]. Further, one US trial that tested an intervention found it to be effective in reducing risk in only one out of four emergent IDU patterns [25]. Likewise, distinct patterns of IDU and sexual risk behaviors that are differentially amenable to change in response to intervention may exist among PWID in the Ukraine trial.
This possibility warrants investigation but necessitates an alternative to traditional regression approaches, which provide effect estimates averaged over all participants, masking heterogeneity in risk behaviors that is of interest here. Latent transition analysis (LTA) can serve this purpose. LTA is a longitudinal extension of latent class analysis, a person-centered analytic approach that categorizes individuals into subgroups, or classes, using an unknown, or latent, grouping variable determined by responses to a set of indicators [28]. LTA allows for examination of how membership in the identified classes changes over time [29, 30]. The primary purpose of the present study was to re-analyze data from the previously described Ukraine trial to understand how the intervention differentially impacted distinct subgroups of participants. Specifically, we aimed to identify patterns of IDU behaviors and condomless sex, assess the extent to which these patterns changed over time in response to intervention, and compare HIV seroprevalence across groups post-intervention. Given that prior, similar research revealed three to four behavioral patterns [25] and that our study includes a larger sample and larger number of examined risk behaviors, we expected at least five behavioral patterns to emerge.
Though it is possible that the epidemiologic context of IDU and HIV in Ukraine has changed in the nearly 10 years since data collection ended for the Ukraine trial, the pertinence of understanding intervention efficacy on risk behavior-reduction to inform future HIV prevention efforts has not. Moreover, evaluating such data from multiple analytic and other perspectives (the lack of which remains a shortcoming in the broader intervention literature) is critical given how labor- and resource-intensive implementing intervention trials is. Furthermore, findings here may be relevant not only for the present Ukrainian context, but for broader Eastern European and other nearby contexts as well.
Methods
Data Source, Participants, and Procedures
Data for this secondary analysis come from a clustered randomized clinical trial of a social network intervention among PWID in Odessa, Donetsk, and Nikolayev, Ukraine (NCT01159704, ClinicalTrial.gov). Detailed methods have been described elsewhere [24]. Briefly, index participants were recruited from the streets of the aforementioned cities by outreach workers from non-governmental organizations. Eligibility criteria included being ≥ 16 years, self-reported drug injection in the past 30 days (verified by signs of recent venipuncture), willingness to participate in interviews and HIV testing, ability to provide informed consent, and willingness to recruit two members of one’s injection network for participation in the study. Network members recruited by index participants also had to meet these eligibility criteria. Recruitment occurred between July 2010 and November 2012, and informed consent was obtained from all participants.
Participants in the control and intervention arms received Ukraine’s standard of care HIV testing and counseling (an updated version of the Counseling and Education model developed during the National Institute on Drug Abuse’s cooperative agreement). Index participants in the intervention arm also received the social network intervention based on SHIELD (Self-Help in Eliminating Life-Threatening Diseases), in which they attended five small-group sessions over two weeks to be trained as peer leaders to influence their injection network members’ injection drug and sexual behaviors [21, 31, 32]. All participants were interviewed and HIV tested at baseline (prior to randomization), 6 months, and 12 months. Data from only those who tested negative for HIV at baseline were examined (N = 1200). As this was a secondary analysis of de-identified data, this study was not characterized as human subjects research and therefore not subject to full review by the San Diego State University institutional review board.
Measures
Latent Class Indicators
At each timepoint, ten yes/no items assessed lifetime engagement in selected IDU behaviors, and those who responded affirmatively were asked to indicate the number of times they had engaged in each IDU behavior in the past 30 days, which served as the basis for the latent class indicators. These behaviors included injecting with a syringe that was filled by one’s drug dealer; injecting with collectively prepared drug solution; injecting with drug solution drawn from a common container; splitting drug solution with others; injecting with used needles/syringes; preparing drug solution with a used cooker, used cotton, or used rinse water (each separately assessed); injecting with solution obtained from a preloaded syringe; and injecting with found needles/syringes. Recall period for each indicator was 30 days. Injecting with found needles and injecting with solution obtained from a preloaded syringe were excluded due to low endorsement. The remaining eight IDU behaviors were dichotomized by collapsing all responses > 0 and coding them 1, for engagement in a given behavior in the past 30 days, and 0, for non-engagement. Regarding sexual behaviors, participants who reported no vaginal or anal sex, and participants who reported using condoms for all vaginal and/or anal sex episodes, were coded 0, as having engaged in no condomless sex in the previous 30 days. Participants who reported any condomless sex in the previous 30 days were coded 1. Combined with the IDU behaviors, this totaled nine dichotomous latent class indicators. We included condomless sex with the IDU indicators because the intervention targeted both sets of behaviors, each of which carries high risk for transmitting HIV, particularly among PWID [10,11,12].
Other Variables
Exposure to the intervention was the main predictor of interest of class transitions. HIV seroprevalence was calculated as the proportion of participants who had tested positive for HIV after 12 months (versus HIV-negative or unknown status). Baseline sociodemographic variables included age (continuous and dichotomized at median), education (high school or less versus post-high school), nationality (Ukrainian, Russian, or other; for regression, dichotomized as Ukrainian versus non-Ukrainian due to small values), relationship status (partnered versus single), sexual orientation (heterosexual versus not), employment status (unemployed versus not), site (Odesa [reference because largest proportion of sample came from there], Donetsk, and Mykolaiv), and injection frequency (daily versus not).
Analysis
Descriptive statistics were calculated for sociodemographic characteristics, latent class indicators, and HIV seroprevalence, after which a random intercept-latent transition analysis (RI-LTA) was performed. The random intercept for each indicator, which varied across individuals but remained constant over time, accounted for time being nested within individuals [33, 34].
Latent Class Enumeration
RI-LTA with full maximum likelihood estimation and robust standard errors was performed on models with two through seven latent classes and a first-order autoregressive component to examine the clustering and transition of IDU and sexual risk behaviors pre- (baseline, visit 1) and post-intervention (12 months, visit 3). Transitions to and from the midpoint (6 months, visit 2) were not examined, as the primary interest was comparing change pre- and post-intervention. Bayesian Information Criterion (BIC), entropy statistic of class delineation, model characteristics (e.g., baseline class prevalence, lowest average latent class probability of latent class membership), parsimony, substantive composition of classes, and scientific interpretation were used for model selection [28, 33, 34]. A full maximum likelihood estimator was used to handle missing data [35, 36].
Latent Class Transitions
Measurement invariance over time was tested using the Satorra-Bentler chi-squared difference test. Indicators that varied over time were freely estimated one-by-one, and the overall model was re-estimated. After fixing the latent classes of the final model to prevent major shifts in class structure via auxiliary modeling procedures [37], a variable representing the intervention was added to determine its effect (via odds ratio) on class transitions. The same procedure was followed to determine the association (also via odds ratio) between class transition and HIV acquisition (using the HIV seroprevalence variable) while controlling for the intervention effect. We were interested in the extent to which transitioning to a given class was associated with testing positive for HIV at 12 months.
Distal Outcome
Using a modified version of the manual Bolck, Croon, and Hagenaars method [37], weights accounting for measurement error taken from the original RI-LTA were incorporated into a model that included HIV seroprevalence as a distal outcome. Modeling HIV seroprevalence as a distal outcome within the RI-LTA framework would reveal both the proportion of participants who had newly tested positive for HIV and the differences in HIV seroprevalence across (with a Wald test) and between (with z-tests) classes as of final class membership (i.e., within each class) at 12 months. Descriptive statistics were calculated in Stata version 15 [38], and RI-LTA was performed in Mplus version 8.6 [39].
Results
Sample Characteristics
Five network participants did not belong to any index participant’s network and were excluded, leaving 1,195 for analysis. Comparable proportions of participants were recruited in each site. Median age was 30 years, and three in four participants were men and were Ukrainian. Over three quarters had high school education or less, and over 40% were unemployed. Less than 2% were sexual minorities, and roughly one in three were partnered. Over 40% injected drugs daily (Table 1). After 12 months, 260 participants (21.8%) across both arms had tested positive for HIV; 837 (70.0%) tested negative, and 98 (8.2%) were unknown.
At baseline and 12 months, roughly two thirds of participants had used a dealer-filled syringe, over 60% had injected collectively prepared solution, over one third had drawn solution from a common container, nearly three fourths had split solution with others, one in nine had injected with a used needle/syringe, and roughly one in four had prepared solution with a used cooker. The remaining indicators demonstrated more variability: preparing solution with used cotton, 16.7% at baseline and 28.3% at 12 months; preparing solution with used rinse water, 13.6% at baseline and 22.3% at 12 months; and having condomless sex, 41.9% at baseline and 29.5% at 12 months (Table 2). Missingness of the indicators was 5.5% at 12 months, associated with non-Ukrainian nationality, and equally distributed across arms.
Model Selection
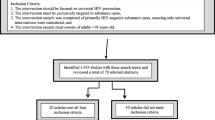
Because the BIC began increasing with the seven-class model, eight- and nine-class models were not examined. Comparison of fit indices indicated the six-class model as the best-fitting, as it had the lowest BIC, though this BIC was only slightly lower than that of the five-class model. Overall entropy was adequate for all models. However, timepoint-specific entropy and lowest average latent class probability for most likely latent class membership were adequate for all models except the six-class model. Baseline class sizes were acceptable across all models (Table 3). Five- and six-class models featured a class with a moderate probability of IDU with used needles/syringes. As IDU with used needles carries one of the highest probabilities for HIV transmission [40], documenting such a class was of great importance. The additional class in the six-class model was not substantively distinct from classes in the five-class model to warrant its selection. Taken together, we selected the more parsimonious five-class model (Fig. 1).
Measurement invariance testing indicated that having injected with used rinse water (χ2[5] = 30.05, p < 0.001), with collectively prepared solution (χ2[5] = 18.84, p < 0.001), with solution drawn from a common container (χ2[5] = 162.86, p < 0.001), and having had condomless sex (χ2[5] = 33.84, p < 0.001) varied over time. Freely estimating these indicators did not resolve the issue or improve fit. However, freeing them in select classes did improve fit over the fully invariant model, but only slightly (17,661.67 versus 17,683.26). Judging this marginal improvement to be not worth the added complexity of adding more parameters to the model to be estimated, we proceeded with the fully invariant model but performed a sensitivity analysis with the partially invariant model.
Class Enumeration
Class 1, “Social injection/equipment-sharing” (baseline prevalence: 11.7%), featured moderate to high probabilities (0.67–1.00) of 7/8 IDU behaviors and a low probability (0.16) of condomless sex. Class 2, “Social injection” (25.9%), featured moderate to high probabilities (0.43–0.91) of 5/8, mostly non-equipment-sharing behaviors and a moderate probability (0.43) of condomless sex. Class 3, “High-risk collective preparation/splitting” (17.0%), featured moderate to high probabilities (0.40–1.00) of 4/8 IDU behaviors, including injecting with used needles/syringes (0.40; highest across classes), and a moderate probability of condomless sex (0.57; highest across classes). Class 4, “Collective preparation/splitting” (11.3%), featured high probabilities (0.94–0.99) of 2/8 IDU behaviors. Class 5, “Dealer-facilitated injection” (34.1%), featured moderate to high probabilities (0.39–0.78) of 2/9 IDU behaviors and a moderate probability (0.38) of condomless sex (Fig. 1).
Participants in the “Dealer-facilitated injection” class were the reference for all baseline comparisons. Participants in the “Social injection/equipment-sharing” class were more likely to be unemployed and inject daily. Those in the “Social injection” class were more likely to reside in Odesa (than either of the other sites), be non-Ukrainian, have post-high school education, be partnered, and inject daily. Participants in the “High-risk collective preparation/splitting” class were more likely to reside in Donetsk (compared to Odesa), be non-Ukrainian, have post-high school education, and inject daily. Those in the “Collective preparation/splitting” class were less likely to reside in Donetsk (compared to Odesa) or be female and more likely to be ≤ 30 years, have post-high school education, and be unemployed (Table 4).
Patterns of Stability and Change
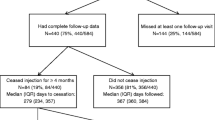
Transition patterns were similar across arms, with increasing prevalence of the “Social injection/equipment-sharing,” “High-risk collective preparation/splitting,” and “Dealer-facilitated injection” classes, and decreasing prevalence of the other classes (Fig. 2). Participants in both the control and intervention arms who started out in the “Social injection/equipment-sharing” class at baseline had comparable probabilities of remaining (0.98 and 0.96, respectively). Though participants in both groups had a low probability of transitioning to any of the other classes, they significantly differed in their probability of transitioning to the “Collective preparation/splitting” class (0.01 and 0.04, respectively). Specifically, the odds of transitioning to the “Collective preparation/splitting” class relative to staying in the “Social injection/equipment-sharing” class were 3.44 times higher for participants in the intervention group compared to those in the control group (OR 3.44, 95% CI 1.29, 9.18).
Latent class transitions of injection drug use and sexual risk behaviors among people who inject drugs in Ukraine (N = 1195). Class prevalence at baseline and 12 months is shown in each column, stratified by control and intervention group. Probabilities of transitioning from the “Social injection/equipment-sharing,” “Social injection,” “High-risk collective preparation/splitting,” and “Dealer-facilitated injection” classes to the “Collective preparation/splitting” class are displayed between columns, as these probabilities significantly differed (p < 0.05) between control and intervention groups
Participants in both control and intervention groups who started out in the “Social injection” class had comparable probabilities of remaining (0.24 and 0.23, respectively) and of transitioning to three of the other four classes. Differences between the control and intervention group were observed in transitioning to the “Collective preparation/splitting” class (0.05 versus 0.17). Specifically, the odds of transitioning to the “Collective preparation/splitting” class relative to staying in the “Social injection” class were 3.33 times higher for participants in the intervention group compared to those in the control group (OR 3.33, 95% CI 1.06, 10.48).
Participants in both the control and intervention groups who started out in the “High-risk collective preparation/splitting” class had comparable probabilities of remaining (0.77 and 0.71, respectively) and of transitioning to three of the other four classes. Differences between the control and intervention group were observed in transitioning to the “Collective preparation/splitting” class, though these probabilities were < 0.01 for both groups. Nonetheless, the odds of transitioning to the “Collective preparation/splitting” class relative to staying in the “High-risk collective preparation/splitting” class were 4.98 times higher for participants in the intervention group compared to those in the control group (OR 4.98, 95% CI 1.48, 16.78).
Participants in both the control and intervention groups who started out in the “Dealer-facilitate injection” class had comparable probabilities of remaining (0.75 and 0.77, respectively) and of transitioning to three of the other four classes. Differences between the control and intervention group were observed in transitioning to the “Collective preparation/splitting” class (0.01 and 0.02, respectively). Specifically, the odds of transitioning to the “Collective preparation/splitting” class relative to staying in the “Dealer-facilitated injection” class were 3.69 times higher for participants in the intervention group relative to those in the control group (OR 3.69, 95% CI 1.20, 11.33).
Participants in both the control and intervention groups who started out in the “Collective preparation/splitting” class had comparable probabilities of transitioning to the other four classes. Differences were observed between the control and intervention groups in remaining in the “Collective preparation/splitting” class (0.06 and 0.20, respectively). The odds of transitioning to the “Social injection/equipment-sharing,” “Social injection,” “High-risk collective preparation/splitting,” and “Dealer-facilitated injection” classes relative to remaining in the “Collective preparation/splitting” class were all lower (OR range: 0.20–0.30; not shown in Fig. 2) for participants in the intervention group compared to those in the control group (Table 5).
HIV Seroprevalence
Overall, controlling for the intervention effect, no class transition was significantly associated with HIV acquisition. Stratified by group, transitioning from the “Collective preparation/splitting” to the “Social injection/equipment-sharing” class was associated with HIV acquisition in the control group (OR 11.56, 95% CI 2.44, 54.72; not displayed). No class transitions were associated with HIV acquisition in the intervention group. At 12 months, HIV seroprevalence in the “High-risk collective preparation/splitting” class was 30.9%, followed by the “Social injection/equipment-sharing” (25.9%), “Social injection” (25.5%), “Collective preparation/splitting” (20.9%), and “Dealer-facilitated injection” classes (16.9%; Wald statistic = 16.61[4], p < 0.01). Statistically significant differences emerged between the “Social injection/equipment-sharing” and “Dealer-facilitated injection” classes (p < 0.01), and the “High-risk collective preparation/splitting” and “Dealer-facilitated injection” classes (p < 0.001).
Sensitivity Analyses
A sensitivity analysis was performed using the partially invariant model, which revealed slight changes in a few parameter estimates compared to those in the main analysis. The odds of transitioning from the “Social injection” to the “Collective preparation/splitting” class (OR 2.90, 95% CI 0.99, 8.46) and of remaining in the “Collective preparation/splitting” class relative to transitioning to the “Social injection” class (OR 0.35, 95% CI 0.12, 1.01) lost but remained close to statistical significance. Additionally, transitioning from the “Collective preparation/splitting” to the “High-risk collective preparation/splitting” class (aOR 7.44, 95% CI 1.30, 42.56) was also associated with HIV acquisition in the control group. All other estimates were comparable to those in the main analysis, leaving inferences unchanged.
Another sensitivity analysis used data from only those participants who completed both baseline and 12-month visits (N = 1131). Excluded participants (n = 64) were more likely to be non-Ukrainian (OR 2.19, 95% CI 1.31, 3.68). The same five-class latent transition model was indicated, with a class structure and item probabilities comparable to those of the main analysis. Likewise, statistical inferences of the remaining findings were comparable to those of the main analysis, with the exception of a few associations between demographic characteristics and baseline class membership (indicated in Table 4).
Discussion
We examined IDU and sexual risk behaviors reported by PWID enrolled in a social network intervention in Odesa, Donetsk, and Mykolaiv, Ukraine. We used RI-LTA to identify five subgroups of PWID engaging in distinct patterns, or classes, of IDU and sexual risk behaviors: “Social injection/equipment-sharing,” “Social injection,” “High-risk collective preparation/splitting,” “Collective preparation/splitting,” and “Dealer-facilitated injection.” Each class featured unsafe injection behavior and/or condomless sex to some degree, though the number and nature of these behaviors varied. Equipment-sharing distinguished the two social injection classes, while condomless sex and injection with used needles/syringes distinguished the collective preparation/splitting classes.
The largest class, “Dealer-facilitated injection,” may reflect the ubiquitous use of locally produced opiates commonly purchased at open-air markets in pre-loaded syringes or from dealers who load the syringe upon purchase in Ukraine [41,42,43,44]. PWID who exclusively utilize this method of IDU would be unlikely to endorse other IDU behaviors because they would not be involved in the production of the drug solution or the preparation of the syringe, which may also indicate that this subset of PWID would be less aware of whether risk-reduction practices were used when preparing the solution and syringe [41, 42]. It is perhaps understandable, then, why this particular behavior has been resistant to intervention efforts, which typically target those who use rather than deal drugs [43]. The smallest class, “Collective preparation/splitting,” featured the smallest number of moderate- to high-probability risk behaviors of all the classes with two: preparing and splitting drug solution with others. Younger participants tended to fall into this class, suggesting younger age could have correlated with more caution with regard to injection drug use practices, possibly due to less experience with injection drug use, or perhaps due to having grown up with more exposure to HIV-prevention messaging.
All risk behaviors except injecting with used needles/syringes and condomless sex were featured in the “Social injection/equipment-sharing” class. Because they are among the most statistically likely to transmit HIV [40], these behaviors have long been prominently featured in public health messaging to populations affected by HIV [45, 46]. Risk associated with the other behaviors featured in this class may receive less attention in intervention efforts, or this particular subgroup of PWID may consider such risks negligible or acceptable relative to those posed by injecting with used needles/syringes and condomless sex. The “Social injection” class differed by its relative lack of equipment-sharing and the substantially higher probability of condomless sex, and was somewhat similar to the “High-risk collective preparation/splitting” class, which had the highest probabilities of condomless sex and drug injection with used needles/syringes. Condomless sex and needle-sharing between injecting sex partners is common [1, 47, 48], amplifying risk for HIV transmission [40]. The “Social injection” class may represent a subset of individuals who inject drugs within the context of intimate relationships but do not share needles/syringes [49, 50], or a subset of individuals who have non-injecting sex partners [51]. However, we cannot make either of these conclusions based on the available data. Condomless sex between injecting and non-injecting partners has indeed become prevalent in Ukraine, contributing to the shift in the country’s HIV epidemic from concentrated to more generalized [5]. Absent among the observed patterns was a class where the probability of endorsing all behaviors was moderate or lower (i.e., a “low risk” class), in contrast to prior research [25,26,27], as each observed class featured a high probability of endorsing at least one IDU risk behavior. This may reflect the severity of the IDU epidemic in Ukraine, but may also reflect the number and diversity of IDU behaviors examined in the present study, which was greater and broader than what has been investigated previously [25,26,27].
Direct comparison of our findings with those from similar studies is not straightforward, as the number and variety of potential injection drug use and sexual risk behaviors to be included in such an analysis will result in different inclusion and categorization decisions by researchers [25,26,27]. However, some similarities and differences are evident. A peer education intervention trial conducted in five urban US cities (Baltimore, Chicago, Los Angeles, New York City, Seattle) revealed four classes, one of which found cooker-, cotton-, and rinse water-sharing to cluster together (similar to our “Social injection/equipment-sharing” class), and two of which found cooker-, cotton-, rinse water-, and needle-sharing to cluster together (different from our findings, as the only class with a moderate or higher probability of needle/syringe-sharing, the “High-risk collective preparation/splitting” class, did not feature any other equipment-sharing) [25]. Two other studies, one in another urban US city (Houston), and one in Kermanshah, Iran (a provincial capital), each found three classes, with condomless sex, needle-sharing, and other drug preparation/equipment-sharing clustering together in two out of three classes in both studies (similar to our “High-risk collective preparation/splitting” class, with the exception of non-needle equipment-sharing, the probabilities of which were all < 0.10 in our class) [26, 27]. A number of methodological factors (e.g., sample size, indicators assessed, indicator categorizations) could have certainly been responsible for the differences in class number and composition observed between these prior studies and ours; however, societal and contextual factors (e.g., drug market, economy) could have played a role as well.
Using a standard set of IDU and sexual behavior indicators and similar analytic approaches in other contexts with large PWID populations is warranted, especially in countries nearby and more comparable to Ukraine, such as those in Eastern Europe, Central Asia, and the Caucasus region that have large populations of PWID who are likewise disproportionately affected by HIV [52, 53]. Several of the behaviors characterizing the classes we identified—including syringe/needle-sharing and other equipment-sharing, sexual behaviors, and social injection—have in fact been reported in several such countries (e.g., Russia, Georgia, Tajikistan, among others), though some behaviors may be less commonly ascertained in surveys than others [54,55,56]. Future efforts to assess a wider range or standard set of specific injection behaviors and apply person-centered analytic approaches would allow for the identification of distinct patterns of risk behavior among PWID populations in these regions, facilitating comparison of patterns across contexts, identification of subgroups of PWID most at-risk for transmission of HIV and other blood-borne infections, and establishment of clearer intervention targets.
In addition to identifying five behavioral classes, our use of RI-LTA allowed us to examine the extent to which a social network intervention affected class transitions over time, revealing intervention effects for transitioning to and remaining in the “Collective preparation/splitting” class. Additionally, after 12 months, classes featuring the highest number of HIV-risk behaviors had higher HIV seroprevalence, while classes featuring the lowest number of HIV-risk behaviors (including the “Collective preparation/splitting” class) had lower seroprevalence. Moreover, transitioning to the “Social injection/equipment-sharing” class was associated with HIV acquisition for control participants.
Transition probabilities from higher-risk classes to the “Collective preparation/splitting” class were all higher for intervention participants relative to control participants, each of which translated to a significant intervention effect. Likewise, transition probabilities from the “Collective preparation/splitting” class to each higher-risk class were all lower for intervention participants relative to control participants; i.e., intervention participants had a higher probability of remaining in the “Collective preparation/splitting” class relative to control participants. These probabilities also translated to a significant intervention effect, the strongest of which was observed in intervention participants’ lower likelihood of transitioning to the “High-risk collective preparation/splitting class.”
These findings recall the aforementioned peer education intervention trial conducted in five US urban cities, wherein intervention participants in the trial’s low risk class (low probabilities of all behaviors) were more likely to remain in the low risk class relative to control participants (similar to what we found with our “Collective preparation/splitting” class), while intervention participants in the high risk class were more likely to transition to the low risk class relative to control participants (comparable to our finding of intervention participants in all higher risk classes being more likely to transition to the “Collective preparation/splitting” class relative to control participants) [25]. As certain PWID subgroups are differentially amenable to social network/peer-based interventions, greater understanding of this differential amenability and adjusting interventions to better target PWID most vulnerable to contracting HIV are needed.
Our observed intervention effects are not an indication that the “Collective preparation/splitting” class is a low-risk class, as the behaviors it features do carry risk for transmission of HIV and other blood-borne infections [57, 58]. However, this finding does indicate that, among a minority of participants and depending on the class from which participants transitioned, the intervention appeared to be effective in reducing equipment-sharing, injection with solution drawn from a common container, injection with dealer-filled syringes, and condomless sex. The greatest percentage of intervention participants transitioning to the “Collective preparation/splitting” class came from the “Social injection” class (second-largest at baseline), with 17%. Class composition may have factored into the intervention’s stronger impact on the “Social injection” class, as this was the only class where membership was associated with being more likely to be partnered and to reside in Odesa. Understanding why this particular pattern of behaviors was more strongly impacted by the intervention is an area for future research. Though no other significant effects of the intervention were detected, the difference in class prevalence increases in the “High-risk collective preparation/splitting” class between control and intervention arms was notable, suggesting the intervention may have been marginally effective in curbing the behaviors featured in this class, which included condomless sex and injection with used needles/syringes. In other words, for some, the intervention was perhaps more effective at preventing transitions to higher-risk classes rather than reducing risk outright; this type of intervention may therefore be more appropriate to implement in populations demonstrating low to moderate behavioral risk profiles than severe ones. Moreover, the drop in overall endorsement of condomless sex at 12 months may indicate that sexual behavior was more effectively targeted by the intervention, though this drop may reflect missing data.
That transitioning to the “Social injection/equipment-sharing” class was associated with HIV acquisition for control participants is notable but unsurprising. Four of the behaviors featured in this class involved sharing equipment used to inject drugs—a consistent predictor of HIV transmission in PWID networks [3]—while the sheer number of risk behaviors provides more opportunities to be exposed to HIV. Low statistical power may have prevented the detection of associations between HIV acquisition and other class transitions; however, the sensitivity analysis did reveal an association with transitioning to the “High-risk collective preparation/splitting class,” which is also unsurprising given the moderate probability of sharing used needles/syringes and having condomless sex in this class. Despite the intervention effect and HIV seroprevalence differences across classes post-intervention, HIV seroprevalence was high in each class after 12 months, similar to the main outcome findings of the trial published previously, wherein HIV incidence was high in both arms but remained statistically significantly lower in the intervention group [24]. The effectiveness of social network interventions among PWID in Ukraine may be constrained by community (e.g., police mistreatment; stigma), institutional/policy (e.g., limited access to opioid substitution therapy), and other barriers (e.g., war), warranting multilevel but more structurally-focused interventions [9, 59,60,61].
There are several limitations to this study. Some missingness due to loss to follow-up was evident at 12 months but was equally distributed across arms, and a full maximum likelihood estimator was used to handle missing data, an approach shown to be comparable to multiple imputation [35, 36]. Moreover, a sensitivity analysis excluding those lost to follow-up revealed findings that were comparable to the main analysis. Second, the sample consisted of index participants in three Ukrainian sites who were recruited by outreach workers, and index participants subsequently recruited members of their own injection network (and only two) to join the study. Had the study been conducted in other urban areas (or in rural areas in addition to urban areas), had participants recruited their entire injection networks (or more than two members), or had the sample been more demographically diverse (e.g., more sexual minorities), findings may have differed. This study may nonetheless be relevant to other comparable contexts, such as other countries in Eastern Europe, Central Asia, and the Caucasus region. Third, most class sizes remained roughly the same across arms over time, suggesting negligible intervention impact. Nevertheless, several significant differences were in fact detected, however minimal, indicating measurable intervention impact for some participants and subgroups.
Lastly, as this was a secondary analysis of data collected between 2010 and 2012, it is conceivable that our findings may not reflect the current HIV and IDU epidemiologic context of Ukraine. However, research conducted since 2012 shows that HIV transmission risk behaviors (e.g., social injection, equipment-sharing, condomless sex) remain common among PWID in Ukraine [62,63,64,65] and that PWID continue to comprise the largest key population disproportionately affected by HIV there [65], with recent data (2017–2019) showing HIV prevalence among PWID to be 22–23% [65], with large gaps at each HIV care continuum stage [59, 65]. While this research suggests the HIV and IDU epidemiologic context may have remained comparable subsequent to our study, it was all conducted prior to the COVID-19 pandemic and the current Russian invasion.
COVID-19 has already led to reduced HIV surveillance and testing [66] and disrupted harm reduction programs [67, 68], and poses particular health risks for PWID that may compromise immunity for those living with HIV and thus more easily facilitate transmission of HIV [69, 70]. Additionally, like the impact of Russia’s annexation of Crimea [71,72,73], disruption in or stoppage of HIV services and drug treatment for PWID, increased HIV prevalence in other areas of Ukraine and surrounding countries due to displacement of people living with HIV, and a consequent exacerbation of HIV-related disparities faced by PWID can be expected. Indeed, the current situation in Ukraine is already characterized by many of these conditions, while under-resourced and overwhelmed health systems in border regions remain ill-equipped to provide HIV care and treatment services to PWID and others living with HIV [69, 70, 74,75,76]. The extent to which these events will shape injection drug use and sexual behavior patterns among PWID in Ukraine and affect the broader HIV and IDU epidemiologic context is not yet known.
Conclusions
Distinct patterns of injection drug use and sexual risk behaviors characterize how people inject drugs in Ukraine, representing differential risk for HIV transmission and differential amenability to change in response to intervention. Scholarship to illuminate the stability of these patterns and the ways in which each may benefit from uniquely tailored programming to reduce risk is needed. Thoughtful, nuanced research and intervention development is particularly relevant given the stark realities facing Ukraine that will substantially upend HIV prevention efforts. Strategic targeting of IDU and sexual behavior patterns like those identified here could be an efficient, cost-effective, and impactful way forward in reducing HIV transmission in Ukraine and comparable contexts. As such endeavors may not be feasible for some time, more pressing matters, such as unfettered access to HIV treatment, should be prioritized.
Data Availability
The data are not publicly available to protect confidentiality. Requests to access the data should be send to the second author (R Booth).
Code Availability
Code may be made available by contacting the first author (JM Wiginton).
References
Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–207.
Degenhardt L, Mathers B, Vickerman P, Rhodes T, Latkin C, Hickman M. Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet. 2010;376(9737):285–301.
De P, Cox J, Boivin JF, Platt RW, Jolly AM. The importance of social networks in their association to drug equipment sharing among injection drug users: a review. Addiction. 2007;102(11):1730–9.
Degenhardt L, Charlson F, Stanaway J, Larney S, Alexander LT, Hickman M, et al. Estimating the burden of disease attributable to injecting drug use as a risk factor for HIV, hepatitis C, and hepatitis B: findings from the Global Burden of Disease Study 2013. Lancet Infect Dis. 2016;16(12):1385–98.
Des Jarlais DC, Feelemyer JP, Modi SN, Arasteh K, Mathers BM, Degenhardt L, et al. Transitions from injection-drug-use-concentrated to self-sustaining heterosexual HIV epidemics: patterns in the international data. PLoS ONE. 2012;7(3): e31227.
Rachlis B, Brouwer KC, Mills EJ, Hayes M, Kerr T, Hogg RS. Migration and transmission of blood-borne infections among injection drug users: understanding the epidemiologic bridge. Drug Alcohol Depend. 2007;90(2–3):107–19.
UNAIDS Joint United Nations Programme on HIV/AIDS. UNAIDS Data 2017. Geneva, Switzerland: UNAIDS. https://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf
European Centre for Disease Prevention and Control & World Health Organization Regional Office for Europe. HIV/AIDS surveillance in Europe 2020 (2019 data). 2020. Solna, Sweden & Copenhagen, Denmark: ECDC & WHO-Europe. https://www.ecdc.europa.eu/sites/default/files/documents/hiv-surveillance-report-2020.pdf
Holt E. Conflict in Ukraine and a ticking bomb of HIV. Lancet HIV. 2018;5(6):e273–4.
World Health Organization Regional Office for Europe. Good practices in Europe: HIV prevention for people who inject drugs implemented by the International HIV/AIDS Alliance in Ukraine. 2014. Copenhagen, Denmark: WHO Regional Office for Europe. https://www.euro.who.int/__data/assets/pdf_file/0003/254352/FINAL-Ukraine-Good-Practice-July-2014-with-covers.pdf
Burruano L, Kruglov Y. HIV/AIDS epidemic in Eastern Europe: recent developments in the Russian Federation and Ukraine among women. Gend Med. 2009;6(1):277–89.
Vitek CR, Čakalo JI, Kruglov YV, Dumchev KV, Salyuk TO, Božičević I, et al. Slowing of the HIV epidemic in Ukraine: evidence from case reporting and key population surveys, 2005–2012. PLoS ONE. 2014;9(9): e103657.
Latkin CA. Outreach in natural settings: the use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Rep. 1998;113(Suppl 1):151–9.
Theall KP, Sterk CE, Elifson KW, Kidder D. Factors associated with positive HIV serostatus among women who use drugs: continued evidence for expanding factors of influence. Public Health Rep. 2003;118(5):415–24.
Tobin KE, Kuramoto SJ, Davey-Rothwell MA, Latkin CA. The STEP into Action study: a peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction. 2011;106(2):366–75.
Neaigus A, Gyarmathy VA, Miller M, Frajzyngier VM, Friedman SR, Des Jarlais DC. Transitions to injecting drug use among noninjecting heroin users: social network influence and individual susceptibility. J Acquir Immune Defic Syndr. 2006;41(4):493–503.
Ghosh D, Krishnan A, Gibson B, Brown SE, Latkin CA, Altice FL. Social network strategies to address HIV prevention and treatment continuum of care among at-risk and HIV-infected substance users: a systematic scoping review. AIDS Behav. 2017;21(4):1183–207.
Booth RE, Lehman WE, Latkin CA, Dvoryak S, Brewster JT, Royer MS, et al. Individual and network interventions with injection drug users in 5 Ukraine cities. Am J Public Health. 2011;101(2):336–43.
Booth RE, Lehman WEK, Latkin CA, Brewster JT, Sinitsyna L, Dvoryak S. Use of a peer leader intervention model to reduce needle-related risk behaviors among drug injectors in Ukraine. J Drug Iss. 2009;39(3):607–25.
Latkin CA, Donnell D, Metzger D, Sherman S, Aramrattna A, Davis-Vogel A, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc Sci Med. 2009;68(4):740–8.
Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol. 2003;22(4):332–9.
Hoffman IF, Latkin CA, Kukhareva PV, Malov SV, Batluk JV, Shaboltas AV, et al. A peer-educator network HIV prevention intervention among injection drug users: results of a randomized controlled trial in St. Petersburg, Russia. AIDS Behav. 2013;17(7):2510–20.
Mihailovic A, Tobin K, Latkin C. The influence of a peer-based HIV prevention intervention on conversation about HIV prevention among people who inject drugs in Baltimore, Maryland. AIDS Behav. 2015;19(10):1792–800.
Booth RE, Davis JM, Dvoryak S, Brewster JT, Lisovska O, Strathdee SA, et al. HIV incidence among people who inject drugs (PWIDs) in Ukraine: results from a clustered randomised trial. Lancet HIV. 2016;3(10):e482–9.
Mackesy-Amiti ME, Finnegan L, Ouellet LJ, Golub ET, Hagan H, Hudson SM, et al. Peer-education intervention to reduce injection risk behaviors benefits high-risk young injection drug users: a latent transition analysis of the CIDUS 3/DUIT study. AIDS Behav. 2013;17(6):2075–83.
Sharifi H, Mirzazadeh A, Noroozi A, Marshall BD, Farhoudian A, Higgs P, et al. Patterns of HIV risks and related factors among people who inject drugs in Kermanshah, Iran: a latent class analysis. J Psychoactive Drugs. 2017;49(1):69–73.
Noor SW, Ross MW, Lai D, Risser JM. Use of latent class analysis approach to describe drug and sexual HIV risk patterns among injection drug users in Houston, Texas. AIDS Behav. 2014;18(Suppl 3):276–83.
Nylund-Gibson K, Choi AY. Ten frequently asked questions about latent class analysis. Trans Issues Psychol Sci. 2018;4(4):440–61.
Lanza ST, Patrick ME, Maggs JL. Latent transition analysis: benefits of a latent variable approach to modeling transitions in substance use. J Drug Issues. 2010;40(1):93–120.
Nylund KL. Latent transition analysis: modeling extensions and an application to peer victimization [dissertation]. University of California-Los Angeles; 2007. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.310.4138&rep=rep1&type=pdf
Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc Sci Med. 2003;56(3):465–76.
Latkin CA, Hua W, Davey MA. Factors associated with peer HIV prevention outreach in drug-using communities. AIDS Educ Prev. 2004;16(6):499–508.
Muthen B. Mplus web talk No. 2: using Mplus to do latent transition analysis and random intercept latent transition analysis. 2021. https://www.statmodel.com/Webtalk2.shtml
Muthén B, Asparouhov T. Latent transition analysis with random intercepts (RI-LTA). Psychol Methods 2020 11/23.
Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Methods. 2001;6(4):330–51.
Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–77.
Asparouhov T, Muthen B. Auxiliary variables in mixture modeling: using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. 2021; Webnote 21, Version 11. https://www.statmodel.com/examples/webnotes/webnote21.pdf
StatCorp LLC. Stata statistical software, release 15. 2017. College Station, TX: StataCorp LLC.
Muthen B, Muthen L. Mplus User's Guide (8th ed.). 1998–2018;8. Los Angeles, CA: Muthen & Muthen.
Patel P, Borkowf CB, Brooks JT, Lasry A, Lansky A, Mermin J. Estimating per-act HIV transmission risk: a systematic review. AIDS. 2014;28(10):1509–19.
Booth RE, Kennedy J, Brewster T, Semerik O. Drug injectors and dealers in Odessa, Ukraine. J Psychoactive Drugs. 2003;35(4):419–26.
Booth RE, Kwiatkowski CF, Brewster JT, Sinitsyna L, Dvoryak S. Predictors of HIV sero-status among drug injectors at three Ukraine sites. AIDS. 2006;20(17):2217–23.
Makarenko I, Ompad DC, Sazonova Y, Saliuk T, DeHovitz J, Gensburg L. Trends in injection risk behaviors among people who inject drugs and the impact of harm reduction programs in Ukraine, 2007–2013. J Urban Health. 2017;94(1):104–14.
Mazhnaya A, Kiriazova T, Chernova O, Tobin K, Owczarzak J. “Now it is mostly done through stashes, to do it in person one has to trust you”: Understanding the retail injection drug market in Dnipro. Ukraine Int J Drug Policy. 2021;87: 102988.
Dejong W, Wolf RC, Austin SB. U.S. Federally funded television public service announcements (PSAs) to prevent HIV/AIDS: a content analysis. J Health Commun. 2001;6(3):249–63.
Sinding SW. Does “CNN” (condoms, needles and negotiation) work better than “ABC” (abstinence, being faithful and condom use) in attacking the AIDS epidemic? Int Fam Plan Perspect. 2005;31(1):38–40.
Azim T, Bontell I, Strathdee SA. Women, drugs and HIV. Int J Drug Policy. 2015;26:S16-21.
Simmons J, Rajan S, McMahon JM. Retrospective accounts of injection initiation in intimate partnerships. Int J Drug Policy. 2012;23(4):303–11.
Bryant J, Brener L, Hull P, Treloar C. Needle sharing in regular sexual relationships: an examination of serodiscordance, drug using practices, and the gendered character of injecting. Drug Alcohol Depend. 2010;107(2–3):182–7.
Rance J, Rhodes T, Fraser S, Bryant J, Treloar C. Practices of partnership: negotiated safety among couples who inject drugs. Health (London). 2018;22(1):3–19.
Deryabina AP, Patnaik P, El-Sadr WM. Underreported injection drug use and its potential contribution to reported increase in sexual transmission of HIV in Kazakhstan and Kyrgyzstan. Harm Reduct J. 2019;16(1):1-018-0274–2.
Davlidova S, Haley-Johnson Z, Nyhan K, Farooq A, Vermund SH, Ali S. Prevalence of HIV, HCV and HBV in Central Asia and the Caucasus: a systematic review. Int J Infect Dis. 2021;104:510–25.
Jolley E, Rhodes T, Platt L, Hope V, Latypov A, Donoghoe M, et al. HIV among people who inject drugs in Central and Eastern Europe and Central Asia: a systematic review with implications for policy. BMJ Open. 2012;2(5):e001465. https://doi.org/10.1136/bmjopen-2012-001465.
Uusküla A, Raag M, Folch C, Prasad L, Karnite A, van Veen MG, et al. Self-reported testing, HIV status and associated risk behaviours among people who inject drugs in Europe: important differences between East and West. AIDS. 2014;28(11):1657–64.
Tran LT, Peacock A, Colledge S, Memedovic S, Grebely J, Leung J, et al. Injecting risk behaviours amongst people who inject drugs: a global multi-stage systematic review and meta-analysis. Int J Drug Policy. 2020;84: 102866.
Otiashvili D, Latypov A, Kirtadze I, Ibragimov U, Zule W. Drug preparation, injection, and sharing practices in Tajikistan: a qualitative study in Kulob and Khorog. Subst Abuse Treat Prev Policy. 2016;11(1):21.
Dumchev KV, Soldyshev R, Qian HZ, Zezyulin OO, Chandler SD, Slobodyanyuk P, et al. HIV and hepatitis C virus infections among hanka injection drug users in central Ukraine: a cross-sectional survey. Harm Reduct J. 2009;23(6):23-7517-6–23.
Kruse GR, Barbour R, Heimer R, Shaboltas AV, Toussova OV, Hoffman IF, et al. Drug choice, spatial distribution, HIV risk, and HIV prevalence among injection drug users in St. Petersburg, Russia. Harm Reduct J. 2009;6:22-7517-6–22.
Sazonova Y, Kulchynska R, Sereda Y, Azarskova M, Novak Y, Saliuk T, et al. HIV treatment cascade among people who inject drugs in Ukraine. PLoS ONE. 2020;15(12): e0244572.
Bojko MJ, Mazhnaya A, Makarenko I, Marcus R, Dvoriak S, Islam Z, et al. “Bureaucracy & beliefs”: assessing the barriers to accessing opioid substitution therapy by people who inject drugs in Ukraine. Drugs (Abingdon Engl). 2015;22(3):255–62.
Lee JO, Yoon Y, Idrisov B, Kiriazova T, Makarenko O, Sereda Y, et al. Violence, HIV risks, and polysubstance use among HIV-positive people who inject drugs in Ukraine. AIDS Behav. 2021;25(7):2120–30.
Corsi KF, Dvoryak S, Garver-Apgar C, Davis JM, Brewster JT, Lisovska O, et al. Gender differences between predictors of HIV status among PWID in Ukraine. Drug Alcohol Depend. 2014;1(138):103–8.
Mazhnaya A, Tobin KE, Owczarzak J. Association between injection in public places and HIV/HCV risk behavior among people who use drugs in Ukraine. Drug Alcohol Depend. 2018;1(189):125–30.
Owczarzak J, Nguyen TQ, Mazhnaya A, Phillips SD, Filippova O, Alpatova P, et al. Outcome evaluation of a “common factors” approach to develop culturally tailored HIV prevention interventions for people who inject drugs. Drug Alcohol Depend. 2019;1(199):18–26.
Kuzin I, Martzynovska V, Antonenko Z. HIV infection in Ukraine. Public Health Center of the Ministry of Health of Ukraine. 2020; Newsletter No. 51.
Kazatchkine M. We cannot let war in Ukraine derail HIV, TB and COVID-19 treatment in eastern Europe. https://www.unaids.org/en/resources/presscentre/featurestories/2022/march/20220309_michel-kazatchkine 2022.
Meteliuk A, Galvez de Leon, Samy J, Madden LM, Pykalo I, Fomenko T, Filippovych M, et al. Rapid transitional response to the COVID-19 pandemic by opioid agonist treatment programs in Ukraine. J Subst Abuse Treat. 2021;121:108164.
Dumchev K, Kiriazova T, Chernova O. Impact of the COVID-19 epidemic on drug markets, substance use patterns, and delivery of harm reduction and treatment services in Ukraine. 2021. https://uiphp.org.ua/media/k2/attachments/2021-02-01_Ukraine_Covid.pdf.
Essar MY, Matiashova L, Tsagkaris C, Vladychuk V, Head M. Infectious diseases amidst a humanitarian crisis in Ukraine: a rising concern. Ann Med Surg (Lond). 2022;3(78): 103950.
Vasylyeva TI, Smyrnov P, Strathdee S, Friedman SR. Challenges posed by COVID-19 to people who inject drugs and lessons from other outbreaks. J Int AIDS Soc. 2020;23(7): e25583.
Filippovych S. Impact of armed conflicts and warfare on opioid substitution treatment in Ukraine: responding to emergency needs. Int J Drug Policy. 2015;26(1):3–5.
Kazatchkine M. Russia’s ban on methadone for drug users in Crimea will worsen the HIV/AIDS epidemic and risk public health. BMJ. 2014;8(348): g3118.
Vasylyeva TI, Liulchuk M, Friedman SR, Sazonova I, Faria NR, Katzourakis A, et al. Molecular epidemiology reveals the role of war in the spread of HIV in Ukraine. Proc Natl Acad Sci USA. 2018;115(5):1051–6.
Altice FL, Bromberg DJ, Dvoriak S, Meteliuk A, Pykalo I, Islam Z, et al. Extending a lifeline to people with HIV and opioid use disorder during the war in Ukraine. Lancet Public Health. 2022;7(5):e482–4.
Kai J, Parczewski M, van de Vijver D. The war refugees from Ukraine: an HIV epidemic is fleeing as well. AIDS. 2022;36(12):1745–6.
Kazatchkine M. Ukrainian war: an economic crisis in Eastern Europe and Central Asia will lead to a health crisis. BMJ. 2022;24(376): o793.
Acknowledgements
The current manuscript was developed through support of NIDA R01 (R01DA042666; PI: Pitpitan). JMW received support from T32DA023356. The original trial was supported by NIDA grant R01DA026739.
Funding
The current manuscript was developed through support of NIDA R01 (R01DA042666; PI: Pitpitan). JMW received support from T32DA023356. The original trial was supported by NIDA grant R01DA026739.
Author information
Authors and Affiliations
Contributions
JMW: conceptualization, formal analysis, methodology, visualization, writing (original draft), writing (review & editing); RB: original funding acquisition, original investigation, writing (review & editing); LRS, LAE, CES, TLP: writing (review & editing); EVP: conceptualization, funding acquisition, project administration, supervision, writing (review & editing).
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Ethical Approval
As this was a secondary analysis of de-identified data, this study was not characterized as human subjects research and therefore not subject to full review by San Diego State University Institutional Review Board (IRB). The original trial was approved by the by the University of Colorado-Denver IRB and by the Ukrainian Institute on Public Health Policy IRB. The original trial was registered with ClinicalTrial.gov, NCT01159704.
Consent to Participate
This was a secondary data of de-identified data. In the original trail, participants provided informed consent to participate.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wiginton, J.M., Booth, R., Eaton, L.A. et al. Injection Drug Use and Sexual Risk Behaviors Among People who Inject Drugs in Ukraine: A Random-Intercept Latent Transition Analysis. AIDS Behav 27, 3012–3026 (2023). https://doi.org/10.1007/s10461-023-04024-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04024-0