Abstract
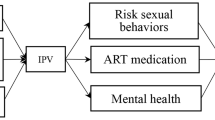
HIV disclosure is crucial for HIV prevention and control, but may also lead to discrimination, insult, and even violence against people living with HIV and AIDS (PLWHAs). In this study, we examined HIV disclosure, its influencing factors, and its association with intimate partner violence (IPV) among 1153 PLWHAs through the sexual route in Jinan, Shandong Province, China. Our results showed that 76.4% (881/1153) PLWHAs had disclosed someone about their HIV infection, the HIV disclosure rates among family members, friends, spouses, and current fixed partners of PLWHAs were 43.5% (501/1153), 47.9% (552/1153), 56.8% (129/227), and 43.2% (336/777), respectively. HIV disclosure was affected by socio-demographics, disease characteristics, and psycho-social factors and varied among family members, close friends, spouses, and current fixed sexual partners. Age ≤ 33 years (aOR 1.79, 95% CI 1.27–2.53), heterosexual infection route (aOR 1.52, 95% CI 1.06–2.17), HIV diagnosis time > 36 months (aOR 1.84, 95% CI 1.30–2.59), with other chronic diseases (aOR 1.87, 95% CI 1.34–2.61), lower self-stigma (aOR 4.03–4.36, 95% CI 1.98–8.74), higher social support (aOR 1.71–1.73, 95% CI 1.03–2.83), no depression (aOR 1.54, 95% CI 1.12–2.11), and no suicidal ideation (aOR 1.79, 95% CI 1.28–2.50) were all independently associated with increased likelihood of HIV disclosure. HIV disclosure was associated with an increased risk of IPV among current fixed sexual partners (aOR 1.87, 95% CI 1.38–2.54) and spouses (aOR 2.54, 95% CI 1.41–4.56). Our findings suggest that the HIV disclosure rate of PLWHAs is still low and is affected by multiple factors. There is an urgent need to design targeted and comprehensive interventions to improve HIV disclosure. IPV prevention should also be incorporated into the intervention system of HIV disclosure to ensure adequate and continuous support for PLWHAs.
Similar content being viewed by others
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
UNAIDS. Global HIV & AIDS statistics—2022 fact sheet. https://www.unaids.org/en/resources/fact-sheet (2012). accessed 1 Sept 2022.
Joint United Nations Programme on HIV/AIDS (UNAIDS). Fast-track: ending the AIDS epidemic by 2030. Geneva: UNAIDS; 2014.
National Health Commission of China. Low prevalence level! China reports 1.14 million existing HIV infections. https://www.cn-healthcare.com/article/20211201/content-563287.html (2021). accessed 1 Dec 2021.
NCAIDS. Progress in AIDS Prevention and Treatment in China. http://ncaids.chinacdc.cn/xxgx/yqxx/201811/t20181123_197488.htm (2018). accessed 19 Sept 2022.
World Health Organization. Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services. https://apps.who.int/iris/handle/10665/251655 (2016). accessed 1 Sept 2019.
Dalal S, Johnson C, Fonner V, et al. Improving HIV test uptake and case finding with assisted partner notification services. AIDS. 2017;31(13):1867–76.
Vermandere H, Aguilera-Mijares S, Martínez-Vargas L, et al. Developing HIV assisted partner notification services tailored to Mexican key populations: a qualitative approach. BMC Public Health. 2021;21(1):555.
Sharma M, Smith JA, Farquhar C, et al. Assisted partner notification services are cost-effective for decreasing HIV burden in western Kenya. AIDS. 2018;32(2):233–41.
O’Connell AA, Reed SJ, Serovich JA. The efficacy of serostatus disclosure for HIV transmission risk reduction. AIDS Behav. 2015;19(2):283–90.
Ostermann J, Pence B, Whetten K, et al. HIV serostatus disclosure in the treatment cascade: evidence from Northern Tanzania. AIDS Care. 2015;27(sup1):59–64.
Xiao Z, Li X, Qiao S, et al. Using communication privacy management theory to examine HIV disclosure to sexual partners/spouses among PLHIV in Guangxi. AIDS Care. 2015;27(sup1):73–82.
Lyimo RA, Stutterheim SE, Hospers HJ, et al. Stigma, disclosure, coping, and medication adherence among people living with HIV/AIDS in Northern Tanzania. AIDS Patient Care STDS. 2014;28(2):98–105.
Tesfaye T, Darega J, Belachew T, et al. HIV positive sero-status disclosure and its determinants among people living with HIV /AIDS following ART clinic in Jimma University Specialized Hospital, Southwest Ethiopia: a facility-based cross-sectional study. Arch Public Health. 2018;76:1.
Xu MJ, Zhao Y, Shao Y, et al. HIV serostatus disclosure to family members and its predictors among adolescents living with HIV receiving ART. Chin J AIDS STD. 2020;26(8):849–51.
Yang YM, Xiao CC, Wang W, et al. HIV disclosure to family members and its associated factors among people with HIV/AIDS. Chin J AIDS STD. 2017;23(08):706–9.
Lee S, Yamazaki M, Harris DR, et al. Social support and human immunodeficiency virus-status disclosure to friends and family: implications for human immunodeficiency virus-positive youth. J Adolesc Health. 2015;57(1):73–80.
Wohl AR, Galvan FH, Myers HF, et al. Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS Behav. 2011;15(6):1098–110.
Salami AK, Fadeyi A, Ogunmodede JA, Desalu OO. Status disclosure among people living with HIV/AIDS in Ilorin, Nigeria. West Afr J Med. 2011;30(5):359–63.
Zang C, He X, Liu H. Selective disclosure of HIV status in egocentric support networks of people living with HIV/AIDS. AIDS Behav. 2015;19(1):72–80.
Longinetti E, Santacatterina M, El-Khatib Z. Gender perspective of risk factors associated with disclosure of HIV status, a cross-sectional study in Soweto, South Africa. PLoS ONE. 2014;9(4): e95440.
Sun M, Chen WT, Yang JP, et al. Concerns of parental HIV disclosure in China. Clin Nurs Res. 2021;30(6):830–9.
Yang Y, Wang W, Kelifa MO, et al. HIV disclosure patterns and psychosocial correlates among people living with HIV in Nanjing, China: a latent class analysis. AIDS Res Hum Retroviruses. 2020;36(3):220–6.
Chi Y, Huang D, Lindgren T, et al. The association between HIV disclosure, spousal testing and unprotected vaginal intercourse within marriage among HIV positive married MSM in China. AIDS Care. 2022;34(1):127–34.
Adeoye-Agboola DI, Evans H, Hewson D, et al. Factors influencing HIV disclosure among people living with HIV/AIDS in Nigeria: a systematic review using narrative synthesis and meta-analysis. Public Health. 2016;136:13–28.
Abler L, Sikkema KJ, Watt MH, Hansen NB, Wilson PA, Kochman A. Depression and HIV serostatus disclosure to sexual partners among newly HIV-diagnosed men who have sex with men. AIDS Patient Care STDS. 2015;29(10):550–8.
Sulstarova B, Poglia Mileti F, Mellini L, et al. HIV disclosure and nondisclosure among migrant women from sub-Saharan Africa living in Switzerland. AIDS Care. 2015;27(4):451–7.
Colombini M, James C, Ndwiga C, et al. The risks of partner violence following HIV status disclosure, and health service responses: narratives of women attending reproductive health services in Kenya. J Int AIDS Soc. 2016;19(1):20766.
Kidman R, Violari A. Dating violence against HIV-infected youth in South Africa: associations with sexual risk behavior, medication adherence, and mental health. J Acquir Immune Defic Syndr. 2018;77(1):64–71.
Stangl AL, Singh D, Windle M, et al. A systematic review of selected human rights programs to improve HIV-related outcomes from 2003 to 2015: what do we know? BMC Infect Dis. 2019;19(1):209.
Wang N, Huang B, Ruan Y, et al. Association between stigma towards HIV and MSM and intimate partner violence among newly HIV-diagnosed Chinese men who have sex with men. BMC Public Health. 2020;20(1):204.
Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: a review. Am J Public Health. 2011;101(6):1011–23.
Ko NY, Lee HC, Hsu ST, et al. Differences in HIV disclosure by modes of transmission in Taiwanese families. AIDS Care. 2007;19(6):791–8.
Mak WW, Cheung RY. Self-stigma among concealable minorities in Hong Kong: conceptualization and unified measurement. Am J Orthopsychiatry. 2010;80(2):267–81.
Shi Y. Assessment of effect of perceived social support on school readiness, mental wellbeing, and self-esteem: mediating role of psychological resilience. Front Psychol. 2022;13: 911841.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–92.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Li XY, Fei LP, Zhang YD, et al. Reliability and validity of the Chinese version of Beck Scate for Suicide Ideation (BSI-CV) among university students. Chin Ment Health J. 2011;25(11):862–6.
Yu Y, Xiao S, Liu KQ. Dating violence among gay men in China. J Interpers Violence. 2013;28(12):2491–504.
Cui Y, Zhou YJ, Li XM, et al. Status and impacts of parental HIV disclosure to children. Chin J AIDS STD. 2019;25(6):588–91.
Omunakwe HE, Okoye H, Efobi C, Onodingene M, Chinenye S, Nwauche CA. Disclosure amongst adult HIV patients on antiretroviral therapy in Port Harcourt, Nigeria. Int J STD AIDS. 2015;26(10):729–32.
He SF, Wang J, Chen J, et al. HIV status disclosure to sexual partners and its related factors among HIV-positive college students reported from 2016 to 2019 in Beijing. Chin J AIDS STD. 2021;27(8):817–21.
Lan GH, Liang NX, Zhou YJ, et al. Influencing factors of HIV positive serostatus disclosure to the regular female sexual partners by HIV infected men who have sex with men in Guangxi. Chin J AIDS STD. 2020;26(9):949–53.
Huang ZC, Mao X, Zhang W, Hu, et al. Resistance factors influencing HIV serostatus disclosure to spouses among married men who have sex with men (MSM) in Shenyang. Chin J AIDS STD. 2018;24(3):250–3.
Haberlen SA, Nakigozi G, Gray RH, et al. Antiretroviral therapy availability and HIV disclosure to spouse in Rakai, Uganda: a longitudinal population-based study. J Acquir Immune Defic Syndr. 2015;69(2):241–7.
Madiba S, Ralebona E, Lowane M. Perceived stigma as a contextual barrier to early uptake of HIV testing, treatment initiation, and disclosure; the case of patients admitted with AIDS-related illness in a rural hospital in South Africa. Healthcare (Basel). 2021;9(8):962.
Maman S, van Rooyen H, Groves AK. HIV status disclosure to families for social support in South Africa. AIDS Care. 2014;26(2):226–32.
Zhang K, Zhao J, Li X, et al. Perceived facilitators and barriers regarding partner notification in people living with HIV in Hunan, China: a qualitative study from the patient perspective. J Assoc Nurses AIDS Care. 2019;30(6):658–67.
Pei JH, Pei YX, Ma T, et al. Prevalence of suicidal ideation, suicide attempt, and suicide plan among HIV/AIDS: a systematic review and meta-analysis. J Affect Disord. 2021;292:295–304.
Ren Y, Yan Y, Chen JD. Qualitative research on the psychology of malicious transmission of HIV/AIDS patients. Chin J Modern Nurs. 2017;23(2):212–5.
Maman S, Groves AK, McNaughton Reyes HL, Moodley D. Diagnosis and disclosure of HIV Status: implications for women’s risk of physical partner violence in the postpartum period. J Acquir Immune Defic Syndr. 2016;72(5):546–51.
Stark L, Seff I, Weber AM, et al. Perpetration of intimate partner violence and mental health outcomes: sex- and gender-disaggregated associations among adolescents and young adults in Nigeria. J Glob Health. 2020;10(1): 010708.
Ho IK, Dinh KT, Smith SA. Intimate partner violence and physical health outcomes among Southeast Asian American women. J Health Psychol. 2017;22(4):515–25.
Dunkle KL, Decker MR. Gender-based violence and HIV: reviewing the evidence for links and causal pathways in the general population and high-risk groups. Am J Reprod Immunol. 2013;69(Suppl 1):20–6.
Siemieniuk RA, Krentz HB, Miller P, et al. The clinical implications of high rates of intimate partner violence against HIV-positive women. J Acquir Immune Defic Syndr. 2013;64(1):32–8.
Centers for Disease Control and Prevention (CDC). Advancing HIV prevention: new strategies for a changing epidemic–United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(15):329–32.
Webber DW. Self-incrimination, partner notification, and the criminal law: negatives for the CDC’s “prevention for positives” initiative. AIDS Public Policy J. 2004;19(1–2):54–66.
Mao X, Leuba SI, Hu Q, et al. Use of multiple recreational drugs is associated with new HIV infections among men who have sex with men in China: a multicenter cross-sectional survey. BMC Public Health. 2021;21(1):354.
He L, Pan X, Wang N, et al. New types of drug use and risks of drug use among men who have sex with men: a cross-sectional study in Hangzhou, China. BMC Infect Dis. 2018;18(1):182.
Lei Y, Wang H, Xiao X, et al. Status and influencing factors of rush poppers use and HIV infection among men who have sex with men in Changsha. Chin J Prev Med. 2016;50(2):148–52.
Stoicescu C, Ameilia R, Irwanto, et al. Syndemic and synergistic effects of intimate partner violence, crystal methamphetamine, and depression on HIV sexual risk behaviors among women who inject drugs in Indonesia. J Urban Health. 2019;96(3):477–96.
Gabbidon K, Chenneville T, Peless T, Sheared-Evans S. Self-disclosure of HIV status among youth living with HIV: a global systematic review. AIDS Behav. 2020;24(1):114–41.
Parker R, Aggleton P, Attawell K, et al. HIV/AIDS-related stigma and discrimination: A conceptual framework and an agenda for action. Horizons report. 2010.
Thapa S, Hannes K, Cargo M, et al. Building a conceptual framework to study the effect of HIV stigma-reduction intervention strategies on HIV test uptake: a scoping review. J Assoc Nurses AIDS Care. 2017;28(4):545–60.
Frye V, Paige MQ, Gordon S, et al. Developing a community-level anti-HIV/AIDS stigma and homophobia intervention in New York city: the project change model. Eval Program Plann. 2017;63:45–53.
Acknowledgements
We extend our gratitude to all PLWHAs who completed the survey. We further thank the HIV specialist nurses and doctors at the Center for Disease Control and Prevention (CDC) of the Central District of Jinan City,China for their effort in recruiting respondents to complete the surveys.
Funding
This study was supported by the Special Funding Project for High-level Innovation Teams and Outstanding Scholars Plan of Guangxi Colleges and University: Research on Emergencies in Guangxi (Department of Education of Guangxi Province, China, Grant No. GuijiaoRenCai[2020]6), the Scientific research project of Hunan Education Department (19B517), and the Guangxi Philosophy and Social Science Foundation Project (22FSH012).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by YY, KQ, FX, HC, YS, JL, ZC, KY, QH, and ZW. Data analysis was performed by YY, KQ, FX, and all authors contributed to the interpretation of data. The first draft of the article was written by YY, KQ, FX, and all authors commented on previous versions of the article. All authors read and approved the final article.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Guangxi Normal University (GXNU [2020] 2002). Informed consent was obtained from all individual participants included in this study.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, Y., Qin, K., Xiao, F. et al. HIV Disclosure Among Sexually Infected People Living with HIV and AIDS in China: Prevalence, Influencing Factors, and Negative Outcomes. AIDS Behav 27, 2411–2429 (2023). https://doi.org/10.1007/s10461-022-03968-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03968-z