Abstract
This paper reports the results of a randomized controlled trial (RCT) to assess the efficacy of Nexus, a telehealth delivered intervention that combines Couples’ HIV counseling and testing (CHTC) with home-based HIV-testing, examining the impact of the intervention on the couples’ formation and adherence to safer sexual agreements. Between 2016 and 2018, 424 couples were recruited online from the U.S and randomized to the intervention arm (a telehealth delivered CHTC session with two home HIV-testing kits) or a control arm (two home HIV-testing kits), with study assessments at baseline, 3 and 6 months. Outcomes were the formation and adherence to safer sexual agreements, dyadic discordance in sexual agreements, breakage of sexual agreements, and perceptions of PrEP. Couples in the intervention arm had significantly greater odds of reporting a safer sexual agreement (3 months OR 1.87, p-value 0.005, and 6 months OR 1.84, p-value 0.007), lower odds of reporting discordant sexual agreements at 6 months (OR 0.62, p-value 0.048), and a significantly lower odds of reporting breaking their sexual agreement (3 months OR 0.51, p-value 0.035, and 6 months OR 0.23, p-value 0.000). By 6 months, couples in the intervention arm were less likely to say PrEP was beneficial to one (RRR 0.33, P = 0.000) or both of them (RRR 0.29, P = 0.000) than being beneficial to neither of the partners. The high levels of acceptability and efficacy of the intervention demonstrate strong potential for the scale-up of this efficacious intervention that is delivered through a low-cost telehealth platform.
Similar content being viewed by others
Introduction
Male couples play a critical role in global HIV epidemics [1] and in the US epidemic [2]. Modeling work demonstrates that between one to two-thirds of HIV infections are from primary partners [3, 4], but few behavioral interventions to reduce the risks of HIV transmission within couples exist. Risks of transmission within male couples are impacted by several factors, including the HIV infection status and viral load of each partner, types of sex engaged in, use of condoms, and sexual risks for HIV acquisition with partners outside the relationship. Couples HIV testing and counseling (CHTC) promotes the incorporation of these factors into a couple-specific prevention plan. Both partners receive HIV counseling and testing together and develop a prevention plan that reflects their joint serostatus and relationship context [5]. CHTC was adapted for US male couples and is considered to be an effective approach to HIV prevention among male couples [6], and a recent randomized control trial of CHTC coupled with adherence counseling for sero-discordant male couples showed efficacy for creating gains in viral suppression for the positive partner [7]. However, similar improvements in health have not been demonstrated for male couples who are not serodiscordant, and CHTC has not been demonstrated to impact HIV prevention behaviors within couples.
Over the past decade, there has been an increase in the use of telehealth platforms to deliver HIV prevention and care, and this growth in telehealth has escalated during the recent COVID-19 pandemic [8]. Telehealth delivered counseling offers a convenient, confidential, and user-controlled opportunity to provide support and information to individuals who otherwise may not be willing or able to access services in-person. The application of telehealth to HIV prevention and care has been shown to be feasible, acceptable, and effective [9,10,11]. Recent studies have demonstrated the ability of telehealth to provide HIV care to GBMSM living with HIV, to provide home-based STI testing, and to provide access to PrEP screening and referrals [12,13,14,15,16,17,18,19]. However, no couples-based HIV telehealth prevention interventions have been reported to date.
We report the results of a randomized controlled trial (RCT) to test the efficacy of Nexus, a telehealth delivered intervention for male couples that combines CHTC with home-based HIV-testing delivered via a video-chat platform. The RCT examined the impact of the intervention on the couples’ sexual agreement making. The hypothesis was that couples exposed to the intervention would be more likely to develop and adhere to a safer sexual agreement (for example, use of condoms or PrEP, or only having condomless sex with their main partner).
Materials and Methods
Study Design
The intervention, Nexus, was evaluated through a RCT, conducted with male couples recruited from across the U.S. Ethical approval was obtained from the University of Michigan (HUM00102906) Institutional Review Board. The study was registered on ClinicalTrials.gov (NCT02335138) before initiating study recruitment. Additional details on procedures and intervention have been published previously [20]. Cohort recruitment began in April 2016 and the final follow-up visit was completed in June 2018. Participants were enrolled and equally randomized to either the Nexus intervention arm (telehealth-delivered CHTC session plus two home HIV-testing kits) or a control arm (two home HIV-testing kits with no offer of telehealth counseling). Couples were followed prospectively for 6 months, with study assessments at baseline, 3 and 6 months.
Participants
Eligible participants of each male couple were: (1) two cis-men who had been in a sexual relationship with each other for > 6 months, (2) both aged > 18 years, (3) both participants not having tested for HIV in the last six months (or for sero-discordant couples, the negative partner not tested for HIV in the last six months), (5) reporting no recent history (< 12 month) of intimate partner violence (IPV) or coercion, (6) being willing to have HIV test kits delivered by mail, (7) having access to internet within their home, (8) report anal sex with each other in the past 6 months, and (9) being either self-reported concordant HIV negative or self-reported HIV sero-discordant. IPV was measured using the GBM-IPV scale [20, 21]. Participants were ineligible if they reported severe physical (hit, slapped, kicked, punched or stabbed) or sexual (forced sex) IPV.
Recruitment and Retention
Participants were recruited from the U.S. via online advertisements placed on key social media websites. Men who clicked on an advertisement were provided a short description of study activities and taken to the study consent form. Consenting men were administered a short eligibility screener. Men who (1) did not consent or (2) did not meet the eligibility criteria or (3) did not provide an email for a main partner (defined as a “sexual relationship with a man who you feel committed to above all others”) were ineligible for study participation. Men who were eligible and provided an email address for their main partner were directed to a registration process. During registration, both men provided email addresses, cell phone numbers, and mailing addresses. Once both partners had consented, completed the screening questionnaire, proven eligible for the study, and registered on the study website, a joint email was sent to both partners asking them to complete the baseline questionnaire individually. This survey collected data on demographics, relationship characteristics, sexual history, and engagement in HIV prevention and care (see measures). Individuals were sent reminders of the follow-up surveys via their preferred method of communication (email or SMS) at two weeks, one week and three days prior to the opening of the survey window.
Randomization
Participant couples were randomized to either the intervention (a telehealth delivered CHTC session with two home HIV-testing kits) or control (two home HIV-testing kits without telehealth counseling) arm using a 1:1 treatment allocation. The treatment assignments were generated with the use of a pseudo-random-number generator.
Procedures: Nexus (Intervention)
For couples randomized to the intervention arm, an email provided details on the expected content of a CHTC session, the expectation that both partners would need to attend the session together and conduct their individual HIV tests and receive their results together in the presence of a remote counselor, and information about the length of the counseling session. Couples were instructed to log on to the study website to order HIV testing kits. Intervention arm couples were asked to select a CHTC appointment time via an electronic calendar. To facilitate an intent to treat analysis, individuals who did not complete the CHTC session or did not schedule an appointment were still able to move on to take the three-month survey and the six-month survey once the survey windows opened. Participants received $50 for each survey completed, but participation in the intervention sessions was not compensated.
Couples attended the virtual CHTC together. The CHTC session content has been described [5] and was conducted by a trained counselor via video-chat using VSee (VSee, Sunnyvale, California, USA) and lasted approximately 30–45 min. Pre-test counseling focused on the couples’ relationship, their perceived HIV risk factors, and included an in-depth discussion of their sexual agreement. Both partners individually conducted their own HIV test and read their individual results together, as instructed by the counselor. Participants were asked to show the counselor their test device, and the counselor confirmed the test results for accuracy of interpretation. Post-test counseling focused on dyadic prevention messages, and revisited the couple’s sexual agreements in light of their test results. The prevention counseling element of the CHTC session focused on talking the couple through prevention options and asking them to consider which prevention options may work best based on their relationship needs, context, and unique risk profile. These prevention messages included focus on repeat testing, PrEP initiation, and re-examining the safety of the couples’ sexual agreement. The goal of the CHTC session was to end the session with a ‘shared vision’, an HIV prevention plan that both members of the dyad agreed to, and reflected their desires and attitudes towards sex within and outside of their relationship. The goal was not to encourage all couples to be monogamous, but to facilitate a discussion with the couple in which they considered the risks for HIV within and beyond their relationship and worked with the counselor to build a prevention plan that reflected their joint sero-status and sexual agreement.
Control Arm
Couples in the control arm received an email informing them that they could order up to two home HIV-testing kits per couple, and were requested to enter their HIV test results into the study portal within 48 h of taking the test. Individuals who did not order the home HIV-testing kits or did not report their results were able to move on to take the three-month survey and the six-month survey once the survey windows opened.
Couple Dissolution
For couples who dissolved their relationship during the course of the follow-up period—post the intervention or control activities—each partner was retained in the study for the full 6 month follow up period and continued to complete survey assessments individually.
Fidelity Monitoring
Fidelity of the intervention delivery was supported using approaches recommended by the Treatment Fidelity Workgroup of the National Institutes of Health Behavior Change Consortium [22]. Specifically, the counselor received booster training throughout the follow-up period, and met with the Principal Investigator to discuss and problem-solve issues that arose during the telehealth sessions.
Measurements
The baseline survey assessed relationship characteristics, including relationship length, marital status, cohabitation status, the label they used to refer to their partner (i.e. boyfriend, husband, partner, lover, fuck-buddy, or other), HIV testing history, and the experience or perpetration of IPV [21, 23] in the past 6 months. Baseline and follow-up surveys collected information on couples’ sexual agreements and their investment in agreements [24], sexual behaviors in the three months before the survey [24, 25]. All measures other than demographic measures were repeated at 3 and 6 month follow-up surveys. At month 6, participants in both arms were asked about the ease of using the home HIV-testing kit, and reactions to the cost of the testing kit (participants were not charged for the kits in the study, but the 6-month survey informed them the retail was around $40 and asked how affordable they felt this was). Participants in the control arm received a description of telehealth CHTC and were asked their willingness to take part in the future.
Statistical Analysis
This study is a RCT of CHTC counseling intervention versus control in 424 male couples observed over 6 months: 209 couples randomized to CHTC counseling and 215 randomized to control. Outcomes of sexual agreement were assessed at 3 time points: baseline, 3 and 6 months. These four outcomes are: (1) safer agreement: the couple both report that they either maintained, switched to or adopted a safer sexual agreement, (2) discordance: the partners report discordant sexual agreements, (3) breakage: either partner reports breaking their agreement, and (4) PrEP: the individual reports that they think PrEP would be beneficial to either themselves or their partner, to both of them, or to neither of them.
Outcomes
Safer agreements were defined as either (1) monogamous with no reported outside sex partners or (2) an open agreement with either no outside sex partners reported, 100% condom use with outside partners, or (3) the partner reporting the outside sex partners are on PrEP, and for sero-discordant couples, 100% condom use with the main partner, the negative partner reports being on PrEP or the positive partner reports being virally suppressed. In addition, to be considered a safer sexual agreement, both members of the dyad had to report the same agreement, had to report having the same understanding of the agreement after a discussion of it, and neither member of the dyad could report breaking the agreement. Discordance was defined by the two members of the dyad reporting different agreements. Breakage was defined by either member of the dyad or both reporting breaking the agreement. Individual PrEP interest was defined by an individual reporting that PrEP would be beneficial for himself or for his partner, but not for both; Couple PrEP Interest was defined by an individual reporting that it would be beneficial for both of them to take PrEP, No PrEP Interest was defined by an individual reporting that it would not be beneficial for either of them to take PrEP.
The analyses followed an intention-to-treat approach. For the outcomes of agreement, discordance and breakage, the percentage of couples who achieved each of the outcomes was compared across study arms, and for the PrEP outcome, the percentage of individuals who achieved the outcome was compared across study arms, using Chi-square test for significant difference. Separate longitudinal regression models were fit for each of the outcomes using STATA version 16. Models were fit using generalized estimating equations (GEE) [26], which is an extension of regression analysis via generalized linear models to the case of repeated observations: AIC criteria were applied to determine the best model fit. The data fit the model assumptions and no further transformations were required. Collinearity between control variables was assessed, using the vif post-modeling command in STATA, which produced a value for each of the explanatory variables in the model. Inference is drawn using robust standard errors with an exchangeable working correlation assumption. For the PrEP outcome, the model included a random intercept term to account for the clustering of individuals within dyads. Models included terms for intervention group assignment, time, and the 2-way interaction between group and time. Using this approach, a statistically significant 2-way interaction between group and time indicates differences in the change of the outcomes from baseline to follow-up for the intervention group. Sensitivity analyses also controlled for ethnicity, given the failure of randomization for Latino ethnicity at baseline. For the outcome of agreement, discordance and breakage, the unit of analysis was the couple; for the PrEP outcome, the unit of analysis was the individual.
Role of Funding Source
The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Results
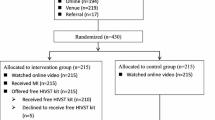
Figure 1 displays the consort diagram for the Project Nexus RCT. In total, 13,592 individuals visited the study website, 2926 consented to take the screener, and 952 (476 couples) were eligible; reasons for ineligibility are depicted in Fig. 1. Of the 476 eligible couples, 424 were randomized: in 13.5% of the 52 couples who did not progress to randomization, only one partner took the baseline survey, 1 couple reported being concordant sero-positive, and 85% did not pass contact information verification process to prove they were two individuals rather than one person. 209 couples were randomized to the intervention arm and 215 couples were randomized to the control arm. 16 sero-discordant male couples were enrolled, randomized equally to each of the arms.
Of the 209 intervention arm couples, 3.3% of couples (7 couples) declined to progress with the study, 4.7% of couples (ten couples) separated before scheduling the intervention, and 1 couple reported serious physical or sexual IPV on the baseline survey. Of the 191 couples who remained eligible, 164 (86%) completed the intervention. Of the 215 control arm couples, 3.7% of couples (8 couples) proved ineligible due to IPV reported on the baseline survey (n = 2), separation (n = 2) or declining further progress in the study (n = 4). Of the remaining 207 couples, 191 (92%) couples ordered HIV testing kits and reported their results, in 12 (6%) couples only one partner ordered a testing kit and reported their results, and in 4 (2%) couples neither partner ordered a testing kit and reported their results.
Retention rates were high in both arms. In the intervention arm 84% of couples both completed the 3- and 6-month assessments: in the control arm, 93% of couples both completed the 3-month assessment and 87% of couples both completed the 6 month assessment. For individuals, in the intervention arm retention rates were 85% at 3 months and 87% at 6 months. In the control arm, the retention rates for individuals were 96% at 3 months and 94% at 6 months. In the intervention arm, 8 couples (3.8%) reported separation in the follow-up period, and 15 couples (6.9%) in the control arm reported separating.
The sample was predominantly White; 23.0% of the control arm and 16.6% of the intervention arm identified as Latino (Table 1). The sample was highly educated, with a third having graduated college, and more than two-thirds of each arm reported being employed full time. 91.5% of control arm and 89.8% of intervention arm participants identified as gay; the mean age of participants was 30 years. In the control arm, 27.0% reported being married, compared to 29.8% in the intervention arm. A quarter of couples were currently married, and one in 6 had been together for 6–12 months, and participants largely referred to their partner with labels indicating more formal, committed relationships (i.e., boyfriend). One-quarter of men reported substance use in the past 6 months (of which 85% was marijuana use), and half reported binge drinking in the past 6 months. The sample was almost exclusively HIV sero-negative participants, with 98% of participants in each arm reporting being HIV sero-negative, and only 2% in each arm reporting being in a sero-discordant relationship.
Eighty-four per cent of participants reported having a sexual agreement with their partner and monogamy was the most commonly reported agreement (Table 2). Participants in both arms reported highly positive attitudes towards their current agreements, and more than 80% of couples reported no breakages in their agreements in the past 12 months. However, taking into account reports of outside sex partners and whether the couple both reported talking about their agreement, the data showed a different distribution of agreements. One-third of couples reported not discussing their agreement with their partner, and the prevalence of monogamy reduced to 40% when considering the reporting of outside sex partners. Small percentages of couples who said they were monogamous also reported sex with outside partners, with and without condoms or PrEP. Interestingly, 13% of couples reported they had open sexual agreements but reported no outside sex partners in the past 6 months. Five per cent of couples reported being non-monogamous with outside partners without condom and/or PrEP protection. In terms of condom use, a third of control arm couples and a quarter of intervention arm couples reported no condomless sex in the past 6 months, and majority reported condomless sex only with each other. The median number of outside sex partners in the past 6 months in both arms was one.
Table 3 shows the distribution of the 4 outcomes over time and by arm. There were no significant differences in any study outcome measures by arm at baseline. Approximately half of couples reported a safer sexual agreement at baseline (control arm 53.1%, intervention arm 47.6%); increases in having a safer sexual agreement were larger in the intervention arm than the control arm (at 6 months: control arm 57.5%, intervention arm 69.7%, p = 0.001). At baseline, approximately 14% of couples reported breaking their agreements in the prior 6 months: this reduced in both arms over time to 9.8% in the control arm and 4.0% in the intervention arm (p = 0.002). By 6 months, the percentage of couples who reported discordant agreements declined to 9.1% in the intervention arm but was at 16.7% in the control arm (p = 0.003). At baseline about half of couples in both arms reported that PrEP would not be beneficial to either of them; by 6 months the percentage of couples who reported that it would be beneficial for neither of them to take PrEP had decreased to 26% in the control arm and to 17% in the intervention arm (p = 0.001).
Tables 4 and 5 show the results of the modeling of the 4 outcomes. Couples in the intervention arm had significantly greater odds of reporting a safer sexual agreement (3 months OR 1.87, p-value 0.005, and 6 months OR 1.84, p-value 0.007), lower odds of reporting discordant sexual agreements at 6 months (OR 0.62, p-value 0.048), and a significantly lower odds of reporting breaking their sexual agreement (3 months OR 0.51, p-value 0.035, and 6 months OR 0.23, p-value 0.000). By 6 months, couples in the intervention arm were less likely to say PrEP was beneficial to one (RRR 0.33, P = 0.000) or both of them (RRR 0.29, P = 0.000) than being beneficial to neither of the partners.
The number of preliminary positive HIV test results differed substantially by arm. In the intervention arm, only one preliminary HIV positive test result was identified during a CHTC session. In the control arm, ten participants self-reported preliminary positive HIV test results, but the results were not confirmed by the study counselor looking at the test device as they were in the intervention arm. Thus, there was a differential assessment on this outcome between the two arms. Each of the participants reporting a preliminary positive result was contacted by a study staff member within 48 h and linked to care in their local area; follow-up calls documented 100% linkage to care at 30 days. There was no difference in repeat HIV testing between the two arms at 3 or 6 months.
Attitudes towards the intervention and home HIV-testing were positive (Table 6). Participants reported that the home HIV-testing kit was easy to use, the results were easy to read, and that they felt that the cost of the test ($40) would be affordable in the future. Couples in both arms reported strong agreement that testing at home had aided their ability to communicate with their partner and that it had given them a platform to discuss reducing sexual risk in their relationship. Most couples (84.8%) in the intervention arm said they would be more inclined to test with their partner in the future, and 75% of those in the control arm reported they would be willing to do the intervention in the future.
Discussion
CHTC plus home HIV-testing kits and a video-chat telehealth platform for male couples resulted in significant gains in the formation and adherence to safer sexual agreements. This is the first intervention to show efficacy for creating gains in sexual agreement safety for male couples. It was successful not only for the efficacy of the intervention, but for the very high rates of intervention uptake, with 86% of couples in the intervention arm completing all elements of the intervention. In the control arm, 92% of couples ordered kits and reported their test results. The results demonstrate the feasibility of mailing out HIV-testing kits, providing home-based HIV-testing via telehealth, and receiving high levels of return of results from male couples in the context of a large RCT. The results of the Project Nexus intervention demonstrate the potential for an intervention that provides male couples with a forum for discussing their concerns around HIV and their sexual risks in the presence of a remotely located counselor.
Previous studies have also explored interventions that focus on sexual agreements among male couples. In a pilot RCT to assess the feasibility and acceptability of an electronic health (eHealth) HIV prevention toolkit intervention to encourage sero-concordant negative male couples to establish and adhere to a sexual agreement, researchers found that a significantly higher proportion of couples who received the intervention established a safer agreement 6 months compared with those who received the education control, but this intervention did not include opportunities for HIV testing and agreements were made absent of accurate serostatus knowledge [27]. The 2GETHER intervention involved in-person group-format and in-person couples’ sessions, providing relationship and HIV prevention education to adult male couples in an effort to increase knowledge, motivation, and behavioral skills among male dyads and demonstrated preliminary efficacy in reducing sexual risk behaviors [28]. However, the 2TEGHER intervention used an in-person format, limiting accessibility for many couples. The We Prevent intervention, which is currently being tested in a pilot RCT, provides young (aged 15–19) partnered GBMSM the option of either testing for HIV alone or with their male partner, via a telehealth platform using home HIV-testing kits [29], and has the potential to reach young male couples, who are particularly under-serviced in HIV programming. The recent Stronger Together intervention used CHTC coupled with two sessions of adherence counseling to provide sero-discordant male couples with the opportunity to discuss how to manage HIV risk in their relationship and showed significant efficacy for increasing viral suppression in the positive partner [7]. Stronger Together was delivered in person, and given the success of Project Nexus, opportunities to provide efficacious dyadic interventions in online formats for male couples should be explored further.
The advertisements used in recruitment referred to a “sexual health study for male couples” or a “HIV study for male couples”. It is possible that sero-discordant couples, or the positive partner in such dyads, did not feel that they would be eligible to participate due to their serostatus. Previous studies have successfully enrolled sero-discordant male couples using social media [7], and so more attention is needed to ensure they see themselves reflected in recruitment materials.
The intervention identified one HIV preliminary positive test result, while 10 were reported in the control arm. At baseline there were no differences in HIV risk behaviors between participants in the control and intervention arms, and the differential identification of preliminary HIV positive results between arms is puzzling. It is possible that participants in the control arm over-reported their positive results, perhaps with the expectation that reporting a positive result was required for further progression in the study—however, further work is required to fully understand whether the results represent differential reporting behaviors or there were real differences in positivity rates between arms. In the future, similar trials may require participants to submit photographic evidence of their test results as a validated measure: this has been done successfully in other HIV prevention RCTs [30].
There are several limitations to the current RCT, in addition to the low enrollment of sero-discordant couples. It is possible that participants in the intervention arm over-reported the safety of their sexual agreements, having been exposed to an intervention in which they were explicitly asked to think about and discuss their agreements. Follow-up surveys did not assess whether couples knew other couples in the study, and so the degree of information sharing and contamination could not be assessed, however, this is unlikely in a national study. The RCT was only able to enroll 16 sero-discordant couples (2%), and given the noted high rates of HIV transmission in sero-discordant male couples [31], it remains a research priority to test and adapt efficacious dyadic interventions for the unique needs of sero-discordant male couples. The sample of couples was largely White and highly educated, and for Project Nexus to be fully scalable, it would need to be tested in an implementation study with a more diverse sample of male couples. The RCT was powered to detect changes in sexual agreements, but not changes in sexual behavior or repeat HIV testing and the follow-up period was relatively short. Although our results show that couples make and adhere to safer sexual agreements immediately after CHTC, it is possible that couples may drift from these agreements over time, so studies with longer follow-up periods are required to understand the long term effects of Project Nexus on sexual agreements and whether booster sessions might be needed. Studies with longer follow-up periods would also allow the impact of the intervention on engagement in HIV prevention (i.e. PrEP use and adherence and HIV testing) and sexual risk behaviors to be measured.
Conclusions
The results of the Project Nexus RCT show significant efficacy for creating short-term gains in safer sexual agreements among male couples. While further work is required to understand whether this intervention can create longer term behavioral changes, and to test the intervention with more diverse couples (in terms of sero-status and race), the results are a significant advance in HIV prevention science for male couples. Providing male couples with a forum to talk about their relationships, their sexual behaviors and their perceived risks for HIV within and outside of their relationship is a critical pathway to providing couples with the skills to work together on HIV prevention. The results demonstrate that male couples are highly accepting of dyadic telehealth delivered interventions, and further work is warranted to extend these types of interventions to other areas of HIV prevention and care for male couples.
References
Beyrer C, Baral SD, Collins C, et al. The global response to HIV in men who have sex with men. Lancet. 2016;388:198–206.
Sullivan PS, Satcher Johnson A, Pembleton ES, et al. Epidemiology of HIV in the USA: epidemic burden, inequities, contexts, and responses. Lancet. 2021;397:1095–106.
Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS One. 2012;7:e50522.
Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–62.
Sullivan PS, Stephenson R, Grazter B, et al. Adaptation of the African couples HIV testing and counseling model for men who have sex with men in the United States: an application of the ADAPT-ITT framework. Springerplus. 2014;3:249.
Centers for Disease Control and Prevention. Complete Listing of Risk Reduction Evidence-based Behavioral Interventions. Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention. 2020; published online June 23. https://www.cdc.gov/hiv/research/interventionresearch/compendium/rr/complete.html. Accessed Nov 30, 2020.
Stephenson R, Garofalo R, Sullivan PS, et al. Stronger Together: Results from a randomized controlled efficacy trial of a dyadic intervention to improve engagement in HIV care among serodiscordant male couples in three US cities. AIDS Behav. 2021. https://doi.org/10.1007/s10461-021-03199-8.
Armstrong WS, Agwu AL, Barrette E-P, et al. Innovations in human immunodeficiency virus (HIV) care delivery during the coronavirus disease 2019 (COVID-19) pandemic: policies to strengthen the ending the epidemic initiative-a policy paper of the infectious diseases Society of America and the HIV medicine association. Clin Infect Dis. 2021;72:9–14.
Bowen AM, Williams ML, Daniel CM, Clayton S. Internet based HIV prevention research targeting rural MSM: feasibility, acceptability, and preliminary efficacy. J Behav Med. 2008;31:463–77.
Chiasson MA, Hirshfield S, Rietmeijer C. HIV prevention and care in the digital age. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S94–7.
DeGuzman MA, Ross MW. Assessing the application of HIV and AIDS related education and counselling on the Internet. Patient Educ Couns. 1999;36:209–28.
Stekler JD, McMahan V, Ballinger L, et al. HIV pre-exposure prophylaxis prescribing through telehealth. J Acquir Immune Defic Syndr. 2018;77:e40–2.
Refugio ON, Kimble MM, Silva CL, Lykens JE, Bannister C, Klausner JD. Brief report: PrEPTECH: a telehealth-based initiation program for HIV pre-exposure prophylaxis in young men of color who have sex with men. A pilot study of feasibility. J Acquir Immune Defic Syndr. 2019;80:40–5.
Hoth AB, Shafer C, Dillon DB, Mayer R, Walton G, Ohl ME. Iowa TelePrEP: a public-health-partnered telehealth model for human immunodeficiency virus preexposure prophylaxis delivery in a rural state. Sex Transm Dis. 2019;46:507–12.
Dandachi D, Lee C, Morgan RO, Tavakoli-Tabasi S, Giordano TP, Rodriguez-Barradas MC. Integration of telehealth services in the healthcare system: with emphasis on the experience of patients living with HIV. J Investig Med. 2019;67:815–20.
Ohl ME, Richardson K, Rodriguez-Barradas MC, et al. Impact of availability of telehealth programs on documented HIV viral suppression: a cluster-randomized program evaluation in the veterans health administration. Open Forum Infect Dis. 2019;6:ofz206.
Sullivan S, Sullivan P, Stephenson R. Acceptability and feasibility of a telehealth intervention for sexually transmitted infection testing among male couples: protocol for a pilot study. JMIR Res Protocols. 2019;8:e14481.
Saberi P, Yuan P, John M, Sheon N, Johnson MO. A pilot study to engage and counsel HIV-positive African American youth via telehealth technology. AIDS Patient Care STDS. 2013;27:529–32.
Wootton AR, Legnitto DA, Gruber VA, et al. Telehealth and texting intervention to improve HIV care engagement, mental health and substance use outcomes in youth living with HIV: a pilot feasibility and acceptability study protocol. BMJ Open. 2019;9:e028522.
Stephenson R, Freeland R, Sullivan SP, et al. Home-based HIV testing and counseling for male couples (project nexus): a protocol for a randomized controlled trial. JMIR Res Protoc. 2017;6:e101.
Stephenson R, Finneran C. The IPV-GBM scale: a new scale to measure intimate partner violence among gay and bisexual men. PLoS ONE. 2013;8:e62592.
Bellg AJ. Treatment fidelity workgroup of the NIH behavior change consortium, Borrelli B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium. Health Psychol. 2004;23:443–51.
Finitsis DJ, Pellowski JA, Huedo-Medina TB, Fox MC, Kalichman SC. Visual analogue scale (VAS) measurement of antiretroviral adherence in people living with HIV (PLWH): a meta-analysis. J Behav Med. 2016;39:1043–55.
Neilands TB, Chakravarty D, Darbes LA, Beougher SC, Hoff CC. Development and validation of the sexual agreement investment scale. J Sex Res. 2010;47:24–37.
Sullivan PS, Peterson J, Rosenberg ES, et al. Understanding racial HIV/STI disparities in black and white men who have sex with men: a multilevel approach. PLoS One. 2014;9:e90514.
Cui J. QIC program and model selection in GEE analyses. Stand Genomic Sci. 2007;7(2):209–20.
Mitchell JW, Lee J-Y, Wu Y, Sullivan PS, Stephenson R. Feasibility and acceptability of an electronic health HIV prevention toolkit intervention with concordant HIV-negative, same-sex male couples on sexual agreement outcomes: pilot randomized controlled trial. JMIR Form Res. 2020;4:e16807.
Hosek SG, Green KR, Siberry G, et al. Integrating behavioral HIV interventions into biomedical prevention trials with youth: lessons from Chicago’s project PrEPare. J HIV AIDS Soc Serv. 2013. https://doi.org/10.1080/15381501.2013.773575.
Gamarel KE, Darbes LA, Hightow-Weidman L, Sullivan P, Stephenson R. The development and testing of a relationship skills intervention to improve HIV prevention uptake among young gay, bisexual, and other men who have sex with men and their primary partners (we prevent): protocol for a randomized controlled trial. JMIR Res Protoc. 2019;8:e10370.
Tahlil KM, Ong JJ, Rosenberg NE, et al. Verification of HIV self-testing use and results: a global systematic review. AIDS Patient Care STDS. 2020;34:147–56.
Bavinton BR, Pinto AN, Phanuphak N, et al. Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. Lancet HIV. 2018;5:e438–47.
Funding
This study funded by Foundation for the National Institutes of Health (R01HD078131).
Author information
Authors and Affiliations
Contributions
RS, PS and JM conceptualized the study. RS acquired funding for the study. RS oversaw project administration. SS and RA oversaw data curation. RS and PS conducted the formal statistical analysis with support from BJ: RS, PS and SS directly accessed and verified the data. RS and PS wrote the first draft of the paper. JM, BJ and SS provided review and editing of the paper. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stephenson, R., Sullivan, S.P., Mitchell, J.W. et al. Efficacy of a Telehealth Delivered Couples’ HIV Counseling and Testing (CHTC) Intervention to Improve Formation and Adherence to Safer Sexual Agreements Among Male Couples in the US: Results from a Randomized Control Trial. AIDS Behav 26, 2813–2824 (2022). https://doi.org/10.1007/s10461-022-03619-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03619-3