Abstract
Sexual minority men living in Africa, where many countries criminalize same-sex behavior, are vulnerable to HIV and experience significant barriers to HIV care. Sexual prejudice in healthcare settings is a key contributor to these barriers. Building on social psychological models of prejudice and interpersonal contact at the clinic, we examined the associations between healthcare workers’ sexual prejudice and their comfort to provide care to MSM, and assessed the moderating role of workers’ prior interpersonal contact with MSM. A cross-sectional survey of 147 healthcare workers varying in level of training and expertise working in HIV care organizations was conducted in western Kenya. Sexual prejudice was negatively associated with comfort to provide care to MSM. Prior interpersonal contact with MSM moderated the association between sexual prejudice and comfort to provide care to MSM among nurses/counselors, such that those with low prior contact and high sexual prejudice were the most uncomfortable providing care to MSM. Interventions are needed to address sexual prejudice and encourage positive forms of interpersonal contact with MSM, especially with nurses and counselors who might have more and varied patient interactions, to improve access to the continuum of HIV prevention and care for MSM in Kenya.

Similar content being viewed by others
References
UNAIDS. Global AIDS Monitoring. Indicators for monitoring the 2016 political declaration on ending AIDS. Geneva: UNAIDS; 2019. p. 2018.
Brown T, Peerapatanapokin W. Evolving HIV epidemics: the urgent need to refocus on populations with risk. Curr Opin HIV AIDS. 2019;14(5):337–53.
Sandfort TG, Mbilizi Y, Sanders EJ, Guo X, Cummings V, Hamilton EL, Akelo V, Panchia R, Dominguez K, Stirratt MJ, Chege W. HIV incidence in a multinational cohort of men and transgender women who have sex with men in sub-Saharan Africa: Findings from HPTN 075. PloS one. 2021;16(2):e0247195.
Kimani M, van der Elst EM, Chiro O, Oduor C, Wahome E, Kazungu W, et al. PrEP interest and HIV-1 incidence among MSM and transgender women in coastal Kenya. J Int AIDS Soc. 2019;22(6):e25323.
UNAIDS. Fast Track. Ending the AIDS epidemic by 2030. UNAIDS, Geneva 2014. https://www.unaids.org/sites/default/files/media_asset/JC2686_WAD2014report_en.pdf. Accessed 20 May 2021.
United Nations. Sustainable development goals 2015. Available from: https://www.un.org/sustainabledevelopment/health/.
Bhattacharjee P, McClarty LM, Musyoki H, Anthony J, Kioko J, Kaosa S, et al. Monitoring HIV prevention programme outcomes among key populations in Kenya: findings from a national survey. PloS ONE. 2015;10(8):e0137007.
NACC. Kenya AIDS strategic framework 2014/15–2018/19. Nairobi: Government of Kenya; 2014.
Stahlman S, Beyrer C, Sullivan PS, Mayer KH, Baral SD. Engagement of gay men and other men who have sex with men (MSM) in the response to HIV: a critical step in achieving an AIDS-free generation. AIDS Behav. 2016;20(Suppl 3):330–40.
Unaids HIV. Addressing a blind spot in the response to HIV-reaching out to men and boys. Joint United Nations Programme on HIV/AIDS Geneva. 2017.
Shangani S, Naanyu V, Operario D, Genberg B. Stigma and healthcare-seeking practices of men who have sex with men in Western Kenya: a mixed-methods approach for scale validation. AIDS Patient Care STDS. 2018;32(11):477–86.
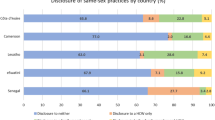
Qiao S, Zhou G, Li X. Disclosure of same-sex behaviors to health-care providers and uptake of HIV testing for men who have sex with men: a systematic review. Am J Mens Health. 2018;12(5):1197–214.
Larsson M, Ross MW, Månsson S-A, Nyoni J, Shio J, Agardh A. Being forced to become your own doctor: men who have sex with Men’s experiences of stigma in the Tanzanian healthcare system. Int J Sex Health. 2016;28(2):163–75.
Risher K, Adams D, Sithole B, Ketende S, Kennedy C, Mnisi Z, et al. Sexual stigma and discrimination as barriers to seeking appropriate healthcare among men who have sex with men in Swaziland. J Int AIDS Soc. 2013;16:18715.
Kapanda L, Jumbe V, Izugbara C, Muula AS. Healthcare providers’ attitudes towards care for men who have sex with men (MSM) in Malawi. BMC Health Serv Res. 2019;19(1):316.
Pettigrew TF. Intergroup contact theory. Annu Rev Psychol. 1998;49(1):65–85.
Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. J Pers Soc Psychol. 2006;90(5):751.
Smith SJ, Axelton AM, Saucier DA. The effects of contact on sexual prejudice: a meta-analysis. Sex Roles. 2009;61(3–4):178–91.
Chan BT, Tsai AC. Personal contact with HIV-positive persons is associated with reduced HIV-related stigma: cross-sectional analysis of general population surveys from 26 countries in sub-Saharan Africa. J Int AIDS Soc. 2017;20(1):21395.
van der Elst EM, Gichuru E, Omar A, Kanungi J, Duby Z, Midoun M, et al. Experiences of Kenyan healthcare workers providing services to men who have sex with men: qualitative findings from a sensitivity training programme. J Int AIDS Soc. 2013;16:18741.
van der Elst EM, Smith AD, Gichuru E, Wahome E, Musyoki H, Muraguri N, et al. Men who have sex with men sensitivity training reduces homoprejudice and increases knowledge among Kenyan healthcare providers in coastal Kenya. J Int AIDS Soc. 2013;16(Suppl 3):18748.
van der Elst EM, Mudza R, Onguso JM, Kiirika L, Kombo B, Jahangir N, et al. A more responsive, multi-pronged strategy is needed to strengthen HIV healthcare for men who have sex with men in a decentralized health system: qualitative insights of a case study in the Kenyan coast. J Int AIDS Soc. 2020;23(Suppl 6):e25597.
Kenya MoH. Strategy for community health 2014–2019: transforming health and accelerating the attainment of health goals. Kenya: Ministry of Health Nairobi; 2014.
Kafu C, Wachira J, Braitstein P, Wilson I, Koech B, Kamene R, et al. Provider perspectives on the role of the patient as an active participant in HIV care. Glob Public Health. 2020. https://doi.org/10.1080/17441692.2020.1830296.
Einterz RM, Kimaiyo S, Mengech HN, Khwa-Otsyula BO, Esamai F, Quigley F, et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med J Assoc Am Med Coll. 2007;82(8):812–8.
Shangani S, Naanyu V, Mwangi A, Vermandere H, Mereish E, Obala A, et al. Factors associated with HIV testing among men who have sex with men in Western Kenya: a cross-sectional study. Int J STD AIDS. 2017;28(2):179–87.
Shangani S, Harrison A, Wachira J, Naanyu V, Operario D. Cultural adaptation and validation of a measure of sexual prejudice against men who have sex with men in Western Kenya among healthcare providers in western Kenya. Glob Public Health. 2020. https://doi.org/10.1080/17441692.2020.1860248.
Sanchez NF, Rabatin J, Sanchez JP, Hubbard S, Kalet A. Medical students’ ability to care for lesbian, gay, bisexual, and transgendered patients. Fam Med-Kans City. 2006;38(1):21.
Holzemer WL, Makoae LN, Greeff M, Dlamini PS, Kohi TW, Chirwa ML, et al. Measuring HIV stigma for PLHAs and nurses over time in five African countries. Sahara J: J Soc Asp HIV/AIDS Res Alliance. 2009;6(2):76–82.
Nyblade L, Jain A, Benkirane M, Li L, Lohiniva A-L, McLean R, et al. A brief, standardized tool for measuring HIV-related stigma among health facility staff: results of field testing in China, Dominica, Egypt, Kenya, Puerto Rico and St. Christopher & Nevis. J Int AIDS Soc. 2013;16(3):18718.
Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26(1):224–7.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: The Guilford Press; 2013.
Aiken LS, West SG, Reno RR. Multiple regression: testing and interpreting interactions. Newbury Park: Sage; 1991.
Matovu JKB, Musinguzi G, Kiguli J, Nuwaha F, Mujisha G, Musinguzi J, et al. Health providers’ experiences, perceptions and readiness to provide HIV services to men who have sex with men and female sex workers in Uganda: a qualitative study. BMC Infect Dis. 2019;19(1):214.
Sekoni AO, Jolly K, Gale NK, Ifaniyi OA, Somefun EO, Agaba EI, et al. Provision of healthcare services to men who have sex with men in Nigeria: students’ attitudes following the passage of the same-sex marriage prohibition law. LGBT Health. 2016;3(4):300–7.
Herek GM, Capitanio JP. “Some of My Best Friends” intergroup contact, concealable stigma, and heterosexuals’ attitudes toward gay men and lesbians. Pers Soc Psychol Bull. 1996;22(4):412–24.
Earnshaw VA, Jin H, Wickersham JA, Kamarulzaman A, John J, Lim SH, et al. Stigma toward men who have sex with men among future healthcare providers in Malaysia: would more interpersonal contact reduce prejudice? AIDS Behav. 2016;20(1):98–106.
Acknowledgements
This research was supported by grants from NIAID (P30AI042853), NIMH (R01MH118075 and K01MH112443), NIH Fogarty International (D43-TW000237), the Nora Kahn Piore Research Fellowship, and the Brown University Global Mobility Program
Funding
This research was supported by grants from NIAID (P30AI042853), NIMH (R01MH118075 and K01MH112443), NIH Fogarty International (D43-TW000237), the Nora Kahn Piore Research Fellowship, and the Brown University Global Mobility Program.
Author information
Authors and Affiliations
Contributions
SS developed the idea, led the data collection and analysis, and wrote the manuscript. DO, BG, AH, JP, VN, and JW provided critical appraisal and helped to draft critical elements of the manuscript. All authors read, edited and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no financial conflict of interest.
Ethical Approval
Ethical approval of the study protocol was reviewed and approved by Brown University institutional review board (IRB) and Moi University institutional research and ethics committee (IREC).
Consent to Participate
Informed consent was obtained from all individual participants included in the study. Participation in the study was voluntary and participants could refuse to answer any question or stop the interview at any time.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shangani, S., Genberg, B., Harrison, A. et al. Sexual Prejudice and Comfort to Provide Services to Men Who Have Sex with Men Among HIV Healthcare Workers in Western Kenya: Role of Interpersonal Contact. AIDS Behav 26, 805–813 (2022). https://doi.org/10.1007/s10461-021-03440-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03440-4