Abstract
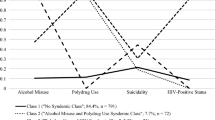
The number of HIV cases attributed to heterosexual contact and the proportion of women among HIV positive individuals has increased worldwide. Russia is a country with the highest rates of newly diagnosed HIV infections in the region, and the infection spreads beyond traditional risk groups. While young women are affected disproportionately, knowledge of HIV risk behaviors in women in the general population remains limited. The objectives of this study were to identify patterns of behaviors that place women of childbearing age at high risk for HIV transmission and determine whether socio-demographic characteristics and alcohol use are predictive of the risk pattern. A total of 708 non-pregnant women, aged between 18 and 44 years, who were at risk for an alcohol-exposed pregnancy were enrolled in two regions in Russia. Participants completed a structured interview focused on HIV risk behaviors, including risky sexual behavior and alcohol and drug use. Latent class analysis was utilized to examine associations between HIV risk and other demographic and alcohol use characteristics and to identify patterns of risk among women. Three classes were identified. 34.93% of participants were at high risk, combining their risk behaviors, e.g., having multiple sexual partners, with high partner’s risk associated with partner’s drug use (class I). Despite reporting self-perceived risk for HIV/STI, this class of participants was unlikely to utilize adequate protection (i.e., condom use). The second high risk class included 13.19% of participants who combined their risky sexual behaviors, i.e., multiple sexual partners and having STDs, with partner’s risk that included partner’s imprisonment and partner’s sex with other women (class II). Participants in this class were likely to utilize protection/condoms. Finally, 51.88% of participants were at lower risk, which was associated primarily with their partners’ risk, and these participants utilized protection (class III). The odds of being in class I compared with class III were 3.3 (95% CI [1.06, 10.38]) times higher for those women who had Alcohol Use Disorders Identification Test scores ≥ 8 than those who had lower scores, and were 3.9 (95% CI [1.69, 8.97]) times higher for those who used alcohol before sex than those who did not. In addition, women who drank more days per week were 1.36 times more likely to be in class II than in class III. The study informs prevention by identifying specific population groups and targets for interventions. Alcohol use is a significant predictor and an overarching factor of HIV risk in women. Since at-risk drinking is common among young Russian women, alcohol risk reduction should be an essential component of HIV prevention efforts.
Similar content being viewed by others
References
UNAIDS. Global report: UNAIDS report on the global AIDS epidemic. http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf (2013).
Rhodes T, Simic M. Transition and the HIV risk environment. BMJ. 2005;331(7510):220–3.
Noor SW, Ross MW, Lai D, Risser JM. Use of latent class analysis approach to describe drug and sexual HIV risk patterns among injection drug users in Houston, Texas. AIDS Behav. 2014;18(Suppl 3):276–83.
Chan PA, Rose J, Maher J, et al. A latent class analysis of risk factors for acquiring HIV among men who have sex with men: implications for implementing pre-exposure prophylaxis programs. AIDS Patient Care STDs. 2015;29(11):597–605.
Wang Q-Q, Chen X-S, Yin Y-P, et al. HIV/STD pattern and its associated risk factors among male STD clinic attendees in China: a foci for HIV intervention. BMC Public Health. 2011;11(1):1–8.
Konda KA, Celentano DD, Kegeles S, Coates TJ, Caceres CF. Latent class analysis of sexual risk patterns among esquineros (street corner men) a group of heterosexually identified, socially marginalized men in urban coastal Peru. AIDS Behav. 2011;15(4):862–8.
European Centre for Disease Prevention and Control (ECDC) WHOWROfE. HIV/AIDS surveillance in Europe 2014. Stockholm: ECDC; 2015. http://ecdc.europa.eu/en/publications/Publications/hiv-aids-surveillance-in-Europe-2014.pdf.
WHO UA. AIDS epidemic update: December. Geneva, Switzerland. http://www.who.int/hiv/mediacentre/2006_EpiUpdate_en.pdf (2006).
Ministry of Health and Social Development of the Russian Federation UNCsF. Children, women and HIV infection in the Russian Federation: analytic review [in Russian]. Moscow: Ministry of Health and Social Development of the Russian Federation, United Nations Children’s Fund; 2004.
UNDP. HIV/AIDS in Eastern Europe and the Commonwealth of Independent States: reversing the epidemic: facts and policy options. Bratislava: UNDP; 2004.
Federal AIDS Center. BИЧ-инфeкция Инфopмaциoнный бюллeтeнь № 39 [HIV Infection Informational Bulletin No. 39]. http://hivrussia.ru/files/bul_39.pdf (2014). Accessed 26 Sep 2016.
Niccolai LM, Shcherbakova IS, Toussova OV, Kozlov AP, Heimer R. The potential for bridging of HIV transmission in the Russian Federation: sex risk behaviors and HIV prevalence among drug users (DUs) and their non-DU sex partners. J Urban Health. 2009;86(Suppl 1):131–43.
UNAIDS. UNAIDS annual report 2008: towards universal access. http://www.unaids.org/sites/default/files/media_asset/jc1736_2008_annual_report_en_1.pdf (2008).
UNAIDS. Global report: UNAIDS report on the global AIDS epidemic. http://www.unaids.org/sites/default/files/media_asset/20121120_UNAIDS_Global_Report_2012_with_annexes_en_1.pdf (2012).
UNAIDS. Progress report on the global response to the HIV/AIDS Epidemic. http://data.unaids.org/topics/ungass2003/ungass_report_2003_en.pdf (2003).
Higgins JA, Hoffman S, Dworkin SL. Rethinking gender, heterosexual men, and women’s vulnerability to HIV/AIDS: time to shift the paradigm. Am J Public Health. 2010;100(3):435–45.
Amirkhanian YA, Kelly JA, Kuznetsova AV, DiFranceisco WJ, Musatov VB, Pirogov DG. People with HIV in HAART-era Russia: transmission risk behavior prevalence, antiretroviral medication-taking, and psychosocial distress. AIDS Behav. 2011;15(4):767–77.
Kelly JA, Amirkhanian YA, McAuliffe TL, et al. HIV risk characteristics and prevention needs in a community sample of bisexual men in St. Petersburg, Russia. AIDS Care. 2002;14(1):63–76.
Benotsch EG, Somlai AM, Pinkerton SD, et al. Drug use and sexual risk behaviours among female Russian IDUs who exchange sex for money or drugs. Int J STD AIDS. 2004;15(5):343–7.
Balachova T, Shaboltas A, Nasledov A, et al. Alcohol and HIV risk among Russian women of childbearing age. AIDS Behav. 2016;21(7):1857–67.
Bedoya CA, Mimiaga MJ, Beauchamp G, Donnell D, Mayer KH, Safren SA. Predictors of HIV transmission risk behavior and seroconversion among Latino men who have sex with men in project EXPLORE. AIDS Behav. 2012;16(3):608–17.
Schwarcz S, Scheer S, McFarland W, et al. Prevalence of HIV infection and predictors of high-transmission sexual risk behaviors among men who have sex with men. Am J Public Health. 2007;97(6):1067–75.
Colfax G, Coates TJ, Husnik MJ, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of san francisco men who have sex with men. J Urban Health. 2005;82(Suppl 1):i62–70.
Colfax GN, Mansergh G, Guzman R, et al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. J Acquir Immune Defic Syndr. 2001;28(4):373–9.
Noor SWB, Ross MW, Lai D, Risser JM. Use of latent class analysis approach to describe drug and sexual HIV risk patterns among injection drug users in Houston, Texas. AIDS Behav. 2014;18(3):276–83.
Green TC, Kershaw T, Lin H, et al. Patterns of drug use and abuse among aging adults with and without HIV: a latent class analysis of a US Veteran cohort. Drug Alcohol Depend. 2010;110(3):208–20.
Monga N, Rehm J, Fischer B, et al. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007;88(1):1–8.
James S, McField ES, Montgomery SB. Risk factor profiles among intravenous drug using young adults: a latent class analysis (LCA) approach. Addict Behav. 2013;38(3):1804–11.
Trenz RC, Scherer M, Duncan A, Harrell PT, Moleko AG, Latimer WW. Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug Alcohol Depend. 2013;132(3):441–8.
Harrell PT, Mancha BE, Petras H, Trenz RC, Latimer WW. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 2012;122(3):220–7.
McCutcheon AL. Latent class analysis. Newbury Park, CA: Sage Publications; 1987.
Balachova T, Bonner BL, Chaffin M, et al. Brief FASD prevention intervention: physicians’ skills demonstrated in a clinical trial in Russia. Addict Sci Clin Pract. 2013;8(1):1.
Sukhanova LP. Cтaтиcтикa poдoвcпoмoжeния кaк фaктop oбecпeчeния кaчecтвa aкyшepcкoй и пepинaтaльнoй пoмoщи в Poccии. [Statistics of obstetric aid as a factor of providing quality of obstetric and perinatal care in Russia]. http://vestnik.mednet.ru/content/view/47/30 (2008).
National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide (updated 2005 edition). Washington, DC: U.S. Government Printing Office; 2005.
Babor TF, Higgins-Biddle JC, Saunders JB. M.G. M. AUDIT: the alcohol use disorders identification test: guidelines for use in primary care. 2nd ed. World Health Organization: Geneva; 2001.
Balachova T, Bonner B, Chaffin M, et al. Women’s alcohol consumption and risk for alcohol-exposed pregnancies in Russia. Addiction (Abingdon, England). 2012;107(1):109–17.
Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–91.
Vermunt JK, Magidson J. Latent GOLD choice user’s guide. Belmont, MA: Statistical Innovations Inc; 2003.
Lynskey MT, Agrawal A, Bucholz KK, et al. Subtypes of illicit drug users: a latent class analysis of data from an Australian twin sample. Twin Res Human Genet. 2012;9(4):523–30.
Carlson RG, Wang J, Falck RS, Siegal HA. Drug use practices among MDMA/ecstasy users in Ohio: a latent class analysis. Drug Alcohol Depend. 2005;79(2):167–79.
Watson C-A, Weng CX, French T, et al. Substance abuse treatment utilization, HIV risk behaviors, and recruitment among suburban injection drug users in Long Island, New York. AIDS Behav. 2014;18(3):305–15.
Muthén LK, Muthén BO. Mplus user’s guide. 7th ed. Los Angeles, CA: Muthén & Muthén; 1998.
Akaike H. Information theory and an extension of the maximum likelihood principle. In: Parzen E, Tanabe K, Kitagawa G, editors. Selected papers of Hirotugu Akaike. New York: Springer; 1998. p. 199–213.
Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–4.
Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Stat Med. 2004;23(9):1455–97.
Federal State Statistics Service. Дeнeжныe дoxoды и пoтpeбитeльcкиe pacxoды в pacчeтe нa дyшy нaceлeния в 2008 гoдy [Monetary income and consumer spending per capita in 2008]. http://www.gks.ru/ (2008).
Federal State Statistics Service. Federal State Statistics Service. http://www.gks.ru/ (2012). Accessed 30 May 2017.
Federal State Statistics Service. Federal state statistics service. http://www.gks.ru/free_doc/new_site/population/bednost/tabl/2-03.htm (2013). Accessed 30 May 2017.
Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004;82(6):454–61.
Moreno R, Nababan HY, Ota E, et al. Structural and community-level interventions for increasing condom use to prevent the transmission of HIV and other sexually transmitted infections. Cochrane Database of Systematic Reviews. 2014;29(7):CD003363.
Townsend L, Mathews C, Zembe Y. A systematic review of behavioral interventions to prevent HIV infection and transmission among heterosexual, adult men in low- and middle-income countries. Prev Sci. 2013;14(1):88–105.
Finer LB, Darroch JE, Singh S. Sexual partnership patterns as a behavioral risk factor for sexually transmitted diseases. Fam Plann Perspect. 1999;31(5):228–36.
Salina DD, Ram D, Jason LA. Perceptions of women’s HIV risk and partner HIV risk behaviors in substance using women with criminal justice involvement. ContempBehav Health Care. 2015;1:33–9.
Helleringer S, Kohler H-P. Sexual network structure and the spread of HIV in Africa: evidence from Likoma Island, Malawi. AIDS. 2007;21(17):2323–32.
Halperin DT, Epstein H. Concurrent sexual partnerships help to explain Africa’s high HIV prevalence: implications for prevention. Lancet. 2004;364(9428):4–6.
Arasteh K, Jarlais DCD, Perlis TE. Alcohol and HIV sexual risk behaviors among injection drug users. Drug Alcohol Depend. 2008;95(1–2):54–61.
Rees V, Saitz R, Horton NJ, Samet J. Association of alcohol consumption with HIV sex- and drug-risk behaviors among drug users. J Subst Abuse Treat. 2001;21(3):129–34.
Stein MD, Charuvastra A, Anderson B, Sobota M, Friedmann PD. Alcohol and HIV risk taking among intravenous drug users. Addict Behav. 2002;27(5):727–36.
Stein MD, Hanna L, Natarajan R, et al. Alcohol use patterns predict high-risk HIV behaviors among active injection drug users. J Subst Abuse Treat. 2000;18(4):359–63.
Montgomery ET, van der Straten A, Stadler J, et al. Male partner influence on women’s HIV prevention trial participation and use of pre-exposure prophylaxis: the importance of “understanding”. AIDS Behav. 2015;19(5):784–93.
Acknowledgements
Sources of support: Research Grant R01AA016234 from the National Institutes of Health/National Institute on Alcohol Abuse and Alcoholism (NIAAA) and Fogarty International Center (Brain Disorders in the Developing World: Research Across the Lifespan) to T. Balachova at OUHSC; and the U.S.-Russia Collaborative HIV/AIDS Research Initiative, the National Institutes of Health (NIH), USA and the Russian Foundation for Basic Research (RFBR), Russia, Administrative Supplement 3R01AA016234-05S1 and Research Grant R21AA022596 from NIAAA to T. Balachova at OUHSC and Research Grant 12-06-91444 from RFBR to A. Shaboltas at SPSU. The authors would like to thank Theresa Exner, PhD, of Columbia University, for her invaluable consultation on the study procedures and development of the study survey measure. The authors wish to acknowledge the contributions of Karen Beckman, MD, and Kathy Kyler, MS, of OUHSC, Sangeeta Agrawal, MS, of Gallup Consulting, and Nicholas Knowlton, MS, of NSK Statistical Solutions. Many thanks also go to Mary Asal, Ekaterina Burina, Elena Kosih, and other graduate students from St. Petersburg State University, Nizhny Novgorod State Pedagogical University, and the University of Oklahoma Health Sciences Center for their assistance with the study. Special thanks go to the participants who volunteered to participate in the study.
Funding
Tatiana Balachova, Som Bohora, Mark Chaffin, Alla Shaboltas, Barbara Bonner, Galina Isurina, Larissa Tsvetkova, Larissa Skitnevskaya, and Elena Volkova, had NIH Grants funding. Alla Shaboltas and Julia Batluk had RFBR Grant funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Contributions
All authors have made substantual contribution to the study design, data gathering, analysis, and/or interpretation of data and have contributed to the intellectual content and preparation of the manuscript. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, NIAAA, FIC, or RFBR.
Conflict of interest
The authors declare that they have no other conflicts of interest.
Ethical Approval
The study approval was obtained from the Institutional Review Boards (IRBs) of both participating universities, the St. Petersburg State University and the University of Oklahoma Health Sciences Center. All procedures performed in the study were in accordance with the ethical standards of the IRBs and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bohora, S., Chaffin, M., Shaboltas, A. et al. Latent Class Analysis of HIV Risk Behaviors Among Russian Women at Risk for Alcohol-Exposed Pregnancies. AIDS Behav 21 (Suppl 2), 243–252 (2017). https://doi.org/10.1007/s10461-017-1929-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1929-9