Abstract
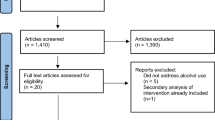
Russia has one of the highest rates of alcohol consumption and is experiencing one of the fastest-growing HIV epidemics in the world. Given these co-occurring health problems, we systematically reviewed combined alcohol and sexual risk interventions to reduce HIV among Russians. We completed comprehensive electronic searches to locate studies that (a) sampled people living in Russia, (b) used a behavioral intervention, and (c) assessed both alcohol and sexual risk behavior. These searches yielded 584 studies, of these, two were included. Compared with controls, intervention participants reported increasing their condom use (ds ranged from 0.12 to 0.85). Within-group improvements in sexual behaviors were found for both groups (ds ranged from 0.19 to 1.94); participants reported fewer sexual partners, more condom use, and reduced alcohol or drug use before sex. These findings support the need and potential benefits for alcohol and HIV interventions among Russians, and suggest directions for public policy.
Resumen
Rusia tiene una de las tasas más altas de consumo de alcohol y está experimentando uno de los más rápidos crecimientos en la epidemia de VIH en el mundo. Teniendo en cuenta estos problemas de salud coexistentes, llevamos a cabo una revisión sistemática de las intervenciones que combinan reducción de consumo de alcohol y riesgo sexual para prevenir el VIH entre los rusos. Las búsquedas electrónicas que se realizaron incluyeron aquellos estudios (a) cuyas muestras fueran de personas que vivieran en Rusia, (b) que utilizaron una intervención conductual, y (c) midieron tanto consumo de alcohol como comportamiento sexual de riesgo. En las búsquedas se obtuvieron 584 estudios, de los cuales 2 fueron incluidos. Los participantes de los grupos de intervención en comparación con los de los grupos control, informaron de un aumento del uso del condón (con ds entre 0,12 y 0,85). Se encontraron mejoras intra-grupo en los comportamientos sexuales tanto para los grupos control como para los experimentales (con ds que iban desde 0,19 hasta 1,94); los participantes informaron de menos parejas sexuales, uso del preservativo con más frecuencia, y una reducción del consumo de alcohol y de drogas antes del sexo. Estos hallazgos apoyan la necesidad y los beneficios potenciales de las intervenciones para reducir el consumo de alcohol y el VIH entre los rusos, y sugieren orientaciones para las políticas públicas.


Similar content being viewed by others
References
Grisin SA, Wallander CA. Russia HIV/AIDS crisis: confronting the present and facing the future center for strategic and international studies. 2002. http://csis.org/files/media/csis/pubs/hiv.pdf. Accessed 2 May 2013.
UNAIDS. Report on the global AIDS epidemic. 2012. http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_en.pdf. Accessed 2 May 2013.
Amirkhanian YA, Tiunov DV, Kelly JA. Risk factors for HIV and other sexually transmitted diseases among adolescents in St. Petersburg, Russia. Fam Plann Perspect. 2001;33(3):106–12.
Rhodes T, Ball A, Stimson GV, Kobyshcha Y, Fitch C, Pokrovsky V, et al. HIV infection associated with drug injecting in the newly independent states, eastern Europe: the social and economic context of epidemics. Addiction. 1999;94(9):1323–36.
Rhodes T, Simic M. Transition and the HIV risk environment. BMJ. 2005;331(7510):220–3.
Kon IS. Russia. In: West D, Green R, editors. Sociolegal control of homosexuality: a multi-nation comparison. New York: Plenum Press; 2002.
Lowndes CM, Alary M. Injection drug use, commercial sex work, and the HIV/STI epidemic in the russian federation. Sex Transm Dis. 2003;30(1):46–8.
Federal AIDS Centre. HIV infection: Informational Bulletin No. 20. 2002.
Dehne K, Khodakevich L, Hamers FF, Schwartlander B. The HIV/AIDS epidemic in eastern Europe: recent patterns and trends and their implication for policy-making. AIDS. 1999;13:741–9.
Dehne K, Pokrovsky V, Kobyshcha Y, Schwartlander B. Update on the epidemics of HIV and other sexually transmitted infections in the newly independent states of the Soviet Union. AIDS. 2000;14(suppl 3):S75–84.
UNAIDS. Country progress report of the Russian Federation on the implementation of the Declaration of Commitment on HIV/AIDS reporting period: Jan 2008–Dec 2009. Russian Federation Federal Service for Surveillance of Consumer Rights Protection and Human Well-Being. 2010. http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2010countries/russia_2010_country_progress_report_en.pdf. Accessed 15 July 2013.
World Health Organization. Russian Federation: summary country profile for HIV/AIDS treatment scale-up. 2010.
UNAIDS/WHO. AIDS epidemic update. 2011.
Wall M, Tkatchenko-Schmidt E, Renton A. Sexual behaviour in Russia: who exhibits a higher risk? Evidence from longitudinal data. Int J STD AIDS. 2006;17(11):759–63.
Zebzeeva G. HIV epidemiological situation in the Orenburg region as of 1 January 2007. Presentation to Regional Monitoring and Evaluation Workshop, 5–7 June 2007 Orenburg, Regional Centre for Preventing and Combating AIDS and Infectious Diseases Presentation to “Mapping the AIDS pandemic” meeting 30 June, Moscow; 2007.
World Health Organization. Risk factors impacting on the spread of HIV among pregnant women in the Russian federation. Geneva: WHO Press; 2007.
Burchell AN, Calzavara LM, Orekhovsky V, Ladnaya NN. Characterization of an emerging heterosexual HIV epidemic in Russia. Sex Trasm Dis. 2008;35(9):807–13.
Toussova O, Shcherbakova I, Volkova G, Niccolai L, Heimer R, Kozlov A. Potential bridges of heterosexual HIV transmission from drug users to the general population in St. Petersburg, Russia: is it easy to be a young female? J Urban Health. 2009;86(Suppl 1):121–30.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33.
Pomerleau J, McKee M, Rose R, Haerpfer CW, Rotman D, Tumanov S. Hazardous alcohol drinking in the former Soviet Union: a cross-sectional study of eight countries. Alcohol Alcohol. 2008;43(3):351–9.
World Health Organization. WHO Country Profile: The Russian Federation 2011. http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/rus.pdf. Accessed 30 Aug 30 2013.
McKee M. Alcohol in Russia. Alcohol Alcohol. 1999;34(6):824–9.
Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis. 2007;34(11):856–63.
Fortenberry JD, Orr DP, Katz BP, Brizendine EJ, Blythe MJ. Sex under the influence. A diary self-report study of substance use and sexual behavior among adolescent women. Sex Transm Dis. 1997;24(6):313–9.
Irwin TW, Morgenstern J, Parsons JT, Wainberg M, Labouvie E. Alcohol and sexual HIV risk behavior among problem drinking men who have sex with men: an event level analysis of timeline followback data. AIDS Behav. 2006;10(3):299–307.
Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141–51.
Kalichman SC, Weinhardt L, DiFonzo K, Austin J, Luke W. Sensation seeking and alcohol use as markers of sexual transmission risk behavior in HIV-positive men. Ann Behav Med. 2002;24(3):229–35.
Morojele NK, Kachieng’a MA, Mokoko E, Nkoko MA, Parry CD, Nkowane AM, et al. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med. 2006;62(1):217–27.
Rhodes T, Cusick L. Accounting for unprotected sex: stories of agency and acceptability. Soc Sci Med. 2002;55(2):211–26.
Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS—a systematic review. Alcohol Alcohol. 2010;45(2):159–66.
Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health. 2010;55(3):159–66.
Abdala N, White E, Toussova OV, Krasnoselskikh TV, Verevochkin S, Kozlov AP, et al. Comparing sexual risks and patterns of alcohol and drug use between injection drug users (IDUs) and non-IDUs who report sexual partnerships with IDUs in St. Petersburg, Russia. BMC Public Health. 2010;10:676.
Abdala N, Grau LE, Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, et al. Inebriation, drinking motivations and sexual risk taking among sexually transmitted disease clinic patients in St. Petersburg, Russia. AIDS Behav. 2013;17(3):1144–50.
National Institute on Alcohol Abuse and Alcoholism. The physicians’ guide to helping patients with alcohol problems. US Department of Health and Human Services. 1995.
Pace CA, Lioznov D, Cheng DM, Wakeman SE, Raj A, Walley AY, et al. Sexually transmitted infections among HIV-infected heavy drinkers in St Petersburg, Russia. Int J STD AIDS. 2012;23(12):853–8.
Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. Lancet. 2010;376(9739):398–400.
Rosenthal R. The “file-drawer” problem and tolerance for null results. Psychol Bull. 1979;86:638–41.
Samet J, Krupitsky E, Cheng D, Raj A, Egorova V, Levenson S, et al. Mitigating risky sexual behaviors among Russian narcology hospital patients: the PREVENT (Partnership to Reduce the Epidemic Via Engagement in Narcology Treatment) randomized controlled trial. Addiction. 2008;103(9):1474–83.
Raj A, Cheng DM, Krupitsky EM, Coleman S, Bridden C, Samet JH. Correlates of any condom use among Russian narcology patients reporting recent unprotected sex. AIDS Behav. 2009;13(2):310–7.
Walley A, Krupitsky E, Cheng D, Raj A, Edwards E, Bridden C, et al. Implications of cannabis use and heavy alcohol use on HIV drug risk behaviors in Russian heroin users. AIDS Behav. 2008;12(4):662–9.
Abdala N, Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV. Efficacy of a brief HIV prevention counseling intervention among STI clinic patients in Russia: a randomized controlled trial. AIDS Behav. 2013;17(3):1016–24.
Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV, Abdala N. Depressive symptoms and unprotected sex in St. Petersburg, Russia. J Psychosom Res. 2012;72(5):371–5.
Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV, Abdala N. Gender differences in the relationship between alcohol use and depressive symptoms in St. Petersburg, Russia. J Addict Res Ther. 2012;3(2).
Raj A, Cheng DM, Krupitsky EM, Levenson S, Egorova VY, Meli S, et al. Binge drinking and unsafe sex: a study of narcology hospital patients from St. Petersburg, Russia. Subst Abus. 2009;30(3):213–22.
Cohen J. Statistical power analysis of the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum; 1998.
Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods. 2002;7(1):105–25.
Sanchez-Meca J, Marin-Martinez F, Chacon-Moscoso S. Effect-size indices for dichotomized outcomes in meta-analysis. Psychol Methods. 2003;8(4):448–67.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Hoboken: Wiley; 2009.
Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks: Sage; 2001.
StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp2011.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Fowkes FG, Fulton PM. Critical appraisal of published research: introductory guidelines. BMJ. 1991;302(6785):1136–40.
Kamb ML, Fishbein M, Douglas JM Jr, Rhodes F, Rogers J, Bolan G, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases. JAMA. 1998;280(13):1161–7.
Ajzen I, Fishbein M. Understanding attitudes and predicting social behaviour. Englewood Cliffs: Prentice-Hall; 1980.
Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44:1175–84.
Albarracin D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005;131:856–97.
Crepaz N, Lyles CM, Wolitski RJ, Passin WF, Rama SM, Herbst JH, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20(2):143–57.
Johnson BT, Scott-Sheldon LA, Carey MP. Meta-synthesis of health behavior change meta-analyses. Am J Public Health. 2010;100(11):2193–8.
Jones BT. Changing alcohol expectancies: techniques for altering motivations for drinking. In: Cox WM, Klinger E, editors. Handbook of motivational counseling: concepts, approaches, and assessment. Hoboken: Wiley; 2004.
Johnson BT, Redding CA, DiClemente RJ, Mustanski BS, Dodge B, Sheeran P, et al. A network-individual-resource model for HIV prevention. AIDS Behav. 2010;14(Suppl 2):204–21.
Noar SM. Behavioral interventions to reduce HIV-related sexual risk behavior: review and synthesis of meta-analytic evidence. AIDS Behav. 2008;12(3):335–53.
Sorensen JL, Copeland AL. Drug abuse treatment as an HIV prevention strategy: a review. Drug Alcohol Depend. 2000;59(1):17–31.
Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, et al. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Ann Behav Med. 2008;36(3):270–9.
Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2007;44(5):594–600.
Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23.
Valentine JC, Pigott TD, Rothstein HR. How many studies do you need? A primer on statistical power for meta-analysis. J Educ Behav Stat. 2010;35(2):215–47.
Cooper HM, Rosenthal R. Statistical versus traditional procedures for summarizing research findings. Psychol Bull. 1980;87(3):442–9.
Perlman FJA. Drinking in transition: trends in alcohol consumption in Russia 1994–2004. BMC Public Health. 2010;10:691.
World Health Organization, Joint United Nations Programme on HIV/AIDS, UNICEF. Global HIV/AIDS response: epidemic update and health sector progress towards universal access. 2011. http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/20111130_ua_report_en.pdf. Accessed 2 May 2013.
Heine S, Andersson P-A. HIV and alcohol. IOGT International. 2009. http://ec.europa.eu/health/alcohol/docs/alcohol_lib23_en.pdf. Accessed 12 July 2013.
World Health Organization. AUIDT: The Alcohol Use Disorders Identification Test, guidelines for use in primary care. 2nd ed. Geneva, Switzerland: World Health Organization; 2001.
Acknowledgments
Research reported in this manuscript was supported by the National Institute of Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R01-AA021355 to Lori A. J. Scott-Sheldon. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Tania B. Huedo-Medina, PhD, for translating our abstract from English to Spanish.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lan, CW., Scott-Sheldon, L.A.J., Carey, K.B. et al. Alcohol and Sexual Risk Reduction Interventions Among People Living in Russia: A Systematic Review and Meta-analysis. AIDS Behav 18, 1835–1846 (2014). https://doi.org/10.1007/s10461-013-0615-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0615-9