Abstract
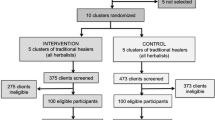
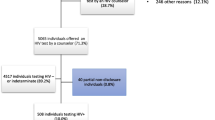
Home-based HIV testing and counseling (HBTC) has the potential to increase access to HIV testing. However, the extent to which HBTC programs successfully link HIV-positive individuals into clinical care remains unclear. To determine factors associated with early enrollment in HIV clinical care, adult residents (aged ≥13 years) in the Health and Demographic Surveillance System in Kisumu, Kenya were offered HBTC. All HIV-positive residents were referred to nearby HIV clinical care centers. Two to four months after HBTC, peer educators conducted home visits to consenting HIV-positive residents. Overall, 9,895 (82 %) of 12,035 residents accepted HBTC; 1,087 (11 %) were HIV-positive; and 737 (68 %) received home visits. Of those receiving home visits, 42 % reported HIV care attendance. Factors associated with care attendance included: having disclosed, living with someone attending HIV care, and wanting to seek care after diagnosis. Residents who reported their current health as excellent or who doubted their HBTC result were less likely to report care attendance. While findings indicate that HBTC was well-received in this setting, less than half of HIV-positive individuals reported current care attendance. Identification of effective strategies to increase early enrollment and retention in HIV clinical care is critical and will require coordination between testing and treatment program staff and systems.


Similar content being viewed by others
References
Kenya National Bureau of Statistics (KNBS), ICF Macro: Kenya demographic and health survey 2008–09. Available at http://www.measuredhs.com/pubs/pdf/fr229/fr229.pdf (2010). Accessed 2 Feb 2012.
Crum NF, Riffenburgh RH, Wegner S, Agan B, Tasker S, Spooner K, et al. Comparisons of causes of death and mortality rates among HIV-infected persons: analysis of the pre-, early, and late HAART (highly active antiretroviral therapy) eras. J Acquir Immune Defic Syndr. 2006;41:194–200.
Lima V, Harrigan R, Bangsberg D, Hogg R, Gross R, Yip B, et al. The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. J Acquir Immune Defic Syndr. 2009;50:529–36.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, HPTN 052 Study Team, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Attia S, Egger M, Muller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23:1397–404.
Donnell D, Baeten JM, Kiaire J, Thomas KK, Stevens W, Cohen CR, Partners in Prevention HSV/HIV Transmission Study Team, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–8.
Kenya National AIDS Control Council. Kenya National AIDS Strategic Plan, 2009/2010–2012/13: delivering on universal access to services. Nairobi: National AIDS Control Council; 2009.
Adazu K, Lindblade KA, Rosen DH, Odhiambo F, Ofware P, Kwach J, et al. Health and demographic surveillance in rural western Kenya: a platform for evaluating interventions to reduce morbidity and mortality from infectious diseases. Am J Trop Med Hyg. 2005;73:1151–8.
Ombok M, Adazu K, Odihambo F, Bayoh N, Kiriinya R, Slutsker L, et al. Geospatial distribution and determinants of child mortality in rural western Kenya 2002–2005. Trop Med Int Health. 2010;15:423–33.
Zeger S, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30.
Hatcher A, Turan J, Leslie H, Kanya L, Kwena Z, Johnson M, et al. Predictors of linkage to care following community-based HIV counseling and testing in rural Kenya. AIDS Behav. 2012;16:1295–307.
Assefa Y, Van D, Mariam DH, Kloos H. Toward universal access to HIV counseling and testing and antiretroviral treatment in Ethiopia: looking beyond HIV testing and ART initiation. AIDS Patient Care STDS. 2010;24:521–5.
Govindasamy D, van Schaik N, Kranzer K, Wood R, Matthews C, Bekker LG. Linkage to HIV care from a mobile testing unit in South Africa by different CD4 count strata. J Acquir Immune Defic Syndr. 2011;58(3):344–52.
Govindasamy D, Ford N, Kranzer K. Risk factors, barriers, and facilitators for linkage to ART care in sub-Saharan Africa: a systematic review. AIDS. 2012; (epub).
Posse M, Baltussen R. Barriers to access to antiretroviral treatment in Mozambique, as perceived by patients and health workers in urban and rural settings. AIDS Patient Care STDS. 2009;23:867–75.
Zachariah R, Harries AD, Manzi M, Gomanj P, Teck R, Philips M, et al. Acceptance of anti-retroviral therapy among patients infected with HIV and tuberculosis in rural Malawi is low and associated with cost of transport. PLoS One. 2006;1:e121.
Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19:658–65.
Miller CM, Kelthapile M, Rybasack-Smith H, Rosen S. Why are antiretroviral treatment patients lost to follow-up? A qualitative study from South Africa. Trop Med Int Health. 2010;15(suppl 1):48–54.
Harries AD, Zachariah R, Lawn SD, Rosen S. Strategies to improve patient retention on antiretroviral therapy in sub-Saharan Africa. Trop Med Int Health. 2010;15(suppl 1):70–5.
Geng EH, Nash D, Kambugu A, Zhang Y, Braitstein P, Christopoulos KA, et al. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep. 2010;7:234–44.
Abaynew Y, Deribew A, Deribe K. Factors associated with late presentation to HIV/AIDS care in South Wollo Zone Ethiopia: a case–control study. AIDS Res Ther. 2011;8:8.
Lawn S, Harries A, Anglaret X, Myer L, Wood R. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS. 2008;22:1897–908.
Kigozi IM, Dobkin LM, Martin JN, Geng EH, Muyindike W, Emenyonu NI, et al. Late-disease stage at presentation to an HIV clinic in the era of free antiretroviral therapy in sub-Saharan Africa. J Acquir Immune Defic Syndr. 2009;52:280–9.
Battegay M, Fluckiger U, Hirschel B, Furrer H. Late presentation of HIV-infected individuals. Antivir Ther. 2007;12:841–51.
Lawn SD, Harries AD, Wood R. Strategies to reduce early morbidity and mortality in adults receiving antiretroviral therapy in resource-limited settings. Curr Opin HIV/AIDS. 2010;5:18–26.
Lahuerta M, Lima J, Elul B, Okamura M, Alvim MF, Nuwagaba-Birbonwoha H, et al. Patients enrolled in HIV care in Mozambique: baseline characteristics and follow-up outcomes. J Acquir Immune Defic Syndr. 2011;58:e75–86.
Ware NC, Idoko J, Kaaya S, Biraro IA, Wyatt MA, Agabji O, et al. Explaining adherence success in sub-Saharan Africa: an ethnographic study. PLoS Med. 2009;6:e11.
Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004;82:299–307.
Rosen S, Fox M. Retention in HIV care between testing and treatment in sub-Saharan Africa: a systematic review. PLoS Med. 2011;8:e1001056.
Wachira J, Kimaiyo S, Ndege S, Mamlin J, Braitstein P. What is the impact of home-based HIV counseling and testing on the clinical status of newly enrolled adults in a large HIV care program in Western Kenya? Clin Infect Dis. 2012;54(2):275–81.
Nakanjako D, Colebunders R, Coutinho AG, Kamya MR. Strategies to optimize HIV treatment outcomes in resource-limited settings. AIDS Rev. 2009;11:179–89.
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52:793–800.
World Health Organization: Patient monitoring guidelines for HIV care and antiretroviral therapy. Available at http://www.who.int/3by5/capacity/ptmonguidelinesfinalv1.PDF (2012). Accessed 10 Mar 2012.
Acknowledgments
This work received funding support through the President’s Emergency Plan for AIDS Relief (PEPFAR) through the U.S. Centers for Disease Control and Prevention (cooperative agreement 5U19CI000323-05). The authors would like to express their gratitude to Maurice Ombok and Alan Rubin for their assistance with the GIS mapping data and to Jan Moore for her insightful comments on earlier drafts of this manuscript. The authors are also grateful for the extraordinary efforts of the HBTC counselors, the field and data management staff of the HDSS, and the facility-based peer educators without whom this study could not have taken place. The authors would also like to thank KEMRI and CDC/KEMRI administrative staff for the support they provided and continue to provide to the project. Finally, the authors would like to thank the HDSS residents for their continued participation. This paper was published with the approval of the director of the Kenya Medical Research Institute.
Conflict of interest
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Medley, A., Ackers, M., Amolloh, M. et al. Early Uptake of HIV Clinical Care After Testing HIV-Positive During Home-Based Testing and Counseling in Western Kenya. AIDS Behav 17, 224–234 (2013). https://doi.org/10.1007/s10461-012-0344-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0344-5