Abstract
Evaluation of vapor uptake by lung airways and subsequent dose to lung tissues provides the bridge connecting exposure episode to biological response. Respiratory vapor absorption depends on chemical properties of the inhaled material, including solubility, diffusivity, and metabolism/reactivity in lung tissues. Inter-dependent losses in the air and tissue phases require simultaneous calculation of vapor concentration in both phases. Previous models of lung vapor uptake assumed steady state, one-way transport into tissues with first-order clearance. A new approach to calculating lung dosimetry is proposed in which an overall mass transfer coefficient for vapor transport across the air–tissue interface is derived using air-phase mass transfer coefficients and analytical expressions for tissue-phase mass transfer coefficients describing unsteady transport by diffusion, first-order, and saturable pathways. Feasibility of the use of mass transfer coefficients was shown by calculating transient concentration levels of inhaled formaldehyde in the human tracheal airway and surrounding tissue. Formaldehyde tracheal air concentration and wall-flux declined throughout the breathing cycle. After the inhalation period, peak tissue concentration moved from the air–tissue interface into the tissue due to desorption into the air and continued diffusional transport across the tissue layer. While model predictions were performed for formaldehyde, which serves as a model of physiologically relevant, highly reactive vapors, the model is equally applicable to other soluble and reactive compounds.








Similar content being viewed by others
Abbreviations
- C a :
-
Vapor concentration in the air
- C t :
-
Vapor concentration in the tissue
- C a:t :
-
Vapor concentration in the air at the air–tissue interface
- C t:a :
-
Vapor concentration in the tissue at the air–tissue interface
- \( C_{{t^{*} }} \) :
-
Maximum tissue concentration in the saturable pathway
- D a :
-
Vapor diffusion coefficient in the air (cm2/s)
- D t :
-
Vapor diffusion coefficient in the tissue (cm2/s)
- J R :
-
Vapor flux across the air–tissue interface
- H t :
-
Height of the tissue layer (cm)
- K f :
-
First-order elimination rate constant (1/s)
- K m :
-
Michaelis–Menten parameter (mg/m3)
- K o :
-
Overall mass transfer coefficient
- k g :
-
Air-phase mass transfer coefficient
- k t :
-
Tissue-phase mass transfer coefficient
- k i :
-
Transient coefficient defined in Eq. (4)
- P t:a :
-
Tissue–air partition coefficient
- Pe :
-
Peclet number
- Re :
-
Reynolds number
- r :
-
Tissue depth
- R :
-
Airway radius
- Sc :
-
Schmidt number
- Sh :
-
Sherwood number
- t :
-
Elapsed time
- t*:
-
Time when C t rises to \( C_{{t^{*} }} \)
- t i :
-
Time when the vapor reaches an airway
- T :
-
Inhalation or inhalation plus pause time
- T inh+pau :
-
Inhalation plus pause time
- T exh :
-
Exhalation time
- U :
-
Average airflow velocity in the airway
- V max :
-
Michaelis–Menten parameter (mg/s)
- V t :
-
Tissue volume (m3)
- z :
-
Airway axial direction
References
Asgharian, B., and O. T. Price. Deposition of ultrafine (nano) particles in the human lung. Inhal. Toxicol. 19:1045–1052, 2007.
Bird, R. B., W. E. Steward, and E. N. Lightfoot. Transport Phenomena. New York: John Wiley & Sons, 1960.
Bush, M. L., T. Raybold, S. Abeles, S.-C. Hu, A. Ben-Jebria, and J. S. Ultman. Longitudinal distribution of ozone absorption in the lung: simulation with a single-path model. Toxicol. Appl. Pharmacol. 140:219–226, 1996.
Bush, M. L., W. Zhang, A. Ben-Jebria, and J. S. Ultman. Longitudinal distribution of ozone and chlorine in the human respiratory tract: simulation of nasal and oral breathing with the single-path diffusion model. Toxicol. Appl. Pharmacol. 173:137–145, 2001.
Cai, F. S., and C. P. Yu. Inertial and interceptional deposition of spherical particles and fibers in a bifurcating airway. J. Aerosol Sci. 19:679–688, 1988.
Cohen Hubal, E. A., J. S. Kimbell, and P. S. Fedkiw. Incorporation of nasal-lining mass-transfer resistance into a CFD model for prediction of ozone dosimetry in the upper respiratory tract. Inhal. Toxicol. 8:831–857, 1996.
Condorelli, P., and S. C. George. Theoretical gas phase mass transfer coefficients for endogenous gases in the lungs. Ann. Biomed. Eng. 27:326–339, 1999.
Conolly, R. B., P. D. Lilly, and J. S. Kimbell. Simulation modeling of the tissue disposition of formaldehyde to predict nasal DNA–protein cross-links in Fischer 344 rats, rhesus monkeys, and humans. Environ. Health Perspect. 108:919–924, 2000.
Cussler, E. L. Diffusion: Mass Transfer in Fluid Systems (2nd ed.). Cambridge, UK: Cambridge University Press, 2003.
Gaston, B., B. J. M. Drazen, J. Loscalzo, and J. S. Stamler. The biology of nitrogen oxides in the airways. Am. J. Respir. Crit. Care Med. 149:538–551, 1994.
Gehr, P., M. Bachofen, and R. R. Weibel. The normal human lung: ultrastructure and morphometric estimation of diffusion capacity. Respir. Physiol. 32:121–140, 1978.
George, S. C., A. L. Babb, and M. P. Hlastala. Dynamics of soluble gas exchange in the airways III. Single-exchange breathing maneuvers. J. Appl. Physiol. 75:2439–2449, 1993.
Grotberg, J. B. Gas absorption in pulmonary airways at low Peclet number. J. Biomech. Eng. 112:177–182, 1990.
Hanna, L. M., S.-R. Lou, S. Su, and A. M. Jarabek. Mass transport analysis: inhalation RfC methods framework for interspecies dosimetric adjustment. Inhal. Toxicol. 13:437–463, 2001.
Hanna, L. M., and P. W. Scherer. A theoretical model of localized heat and water vapor transport in the human respiratory tract. J. Biomech. Eng. 108:19–27, 1986.
Ingham, D. B. Diffusion of aerosols from a stream flowing through a cylindrical tube. Aerosol Sci. 6:125–132, 1975.
International Commission on Radiological Protection (ICRP). Human Respiratory Tract Model for Radiological Protection, Publication 66, Annals of ICRP, Vol. 24. Oxford: Pergamon Press, 16 pp., 1994.
Jackman, J., and O. R. Moss. Mass spectrometry of breath for the diagnosis of infection and exposure. Johns Hopkins APL Tech. Digest 25(1):6–13, 2004.
Jarabek, A. M. The application of dosimetry models to identify key processes and parameters for default dose–response assessment approaches. Toxicol. Lett. 79:171–184, 1995.
Kimbell, J. S., J. H. Overton, R. Subramaniam, P. M. Schlosser, K. T. Morgan, R. B. Conolly, and F. J. Miller. Dosimetry modeling of inhaled formaldehyde: binning nasal flux predictions for quantitative risk assessment. Toxicol. Sci. 64:111–121, 2001.
Longest, P. W., and C. Kleinstreuer. Computational models for simulating multicomponent aerosol evaporation in the upper respiratory airways. Aerosol Sci. Technol. 39:124–138, 2005.
Lou, S.-R. Modeling of Gas Absorption: Upper Airway Scrubbing. Dissertation, John Hopkins University, Baltimore, MD, 1993.
McJilton, C., J. Thielke, and R. Frank. Ozone uptake for the respiratory system. In: Abstracts of Technical Papers, American Industrial Hygiene Conference, May 14–19, Paper No. 45, 1972.
Miller, F. J., D. B. Daniel, and D. L. Coffin. Similarity between man and laboratory animals in regional pulmonary deposition of ozone. Environ. Res. 17:84–101, 1978.
Miller, F. J., J. H. Overton, R. H. Jaskot, and D. B. Menzel. A model of the regional uptake of gaseous pollutants in the lung. Toxicol. Appl. Pharmacol. 79:11–27, 1985.
Nodelman, V., and J. S. Ultman. Longitudinal distribution of chlorine absorption in human airways: a comparison to ozone absorption. J. Appl. Physiol. 87:2073–2080, 1999.
Nuckols, M. L. Heat and Water Vapor Transfer in the Human Respiratory System at Hyperbaric Condition. PhD Dissertation, Duke University, Durham, NC, 1981
Overton, J. H., and R. C. Graham. Predictions of ozone absorption in human lungs from newborn to adults. Health Phys. 57:29–36, 1989.
Overton, J. H., R. C. Graham, and F. J. Miller. A model of ozone uptake of gaseous pollutants in the lung. Toxicol. Appl. Pharm. 88:418–432, 1987.
Overton, J. H., J. S. Kimbell, and F. J. Miller. Dosimetry modeling of inhaled formaldehyde: the human respiratory tract. Toxicol. Sci. 64:122–134, 2001.
Padaki, A., J. S. Ultman, and A. Borhan. Ozone uptake during inspiratory flow in a model of the larynx, trachea and primary bronchial bifurcation. Chem. Eng. Sci. 64:4640–4648, 2009.
Pich, J. Theory of gravitational deposition of particles from laminar flows in channels. Aerosol Sci. 3:351–361, 1972.
Ranz, W. E., and W. R. Marshall. Evaporation from drops: part I. Chem. Eng. Progr. 48:141–146, 1952.
Ranz, W. E., and W. R. Marshall. Evaporation from drops: part II. Chem. Eng. Progr. 48:173–180, 1952.
Scherer, P. W., L. H. Shendalman, and N. M. Greene. Simultaneous diffusion and convection in single breath lung washout. Bull. Math. Biophys. 34:393–412, 1972.
Schroeter, J. D., J. S. Kimbell, E. A. Gross, G. A. Willson, D. C. Dorman, Y. M. Tan, and H. J. Clewell. Application of physiological computational fluid dynamics models to predict interspecies nasal dosimetry of inhaled acrolein. Inhal. Toxicol. 20:227–243, 2008.
Taulbee, D. B., and C. P. Yu. A theory of aerosol deposition in the human respiratory tract. J. Appl. Physiol. 38:77–84, 1975.
Taylor, A. B., A. Borhan, and J. S. Ultman. Three-dimensional simulations of reactive gas uptake in single airway bifurcations. Ann. Biomed. Eng. 35:235–249, 2007.
Tian, G., and P. W. Longest. Application of a new dosimetry program TAOCS to assess transient vapor adsorption in the upper airways. Inhal. Toxicol. 22(13):1047–1063, 2010.
Tian, G., and P. W. Longest. Development of a CFD boundary condition to model transient vapor absorption in the respiratory airways. ASME J. Biomech. Eng. 132:051003, 2010.
Tian, G., and P. W. Longest. Transient absorption of inhaled vapors into a multilayer mucus–tissue–blood system. Ann. Biomed. Eng. 38:517–536, 2010.
U. S. EPA. Methods for Derivation of Inhalation Reference Concentration and Application of Inhalation Dosimetry, EPA/600/8-90066F. Washington, DC: Office of Health and Environment Assessment, U.S. Environmental Protection Agency, 1994.
White, D. C., R. Geyer, J. Cantu, S.-C. Jo, A. D. Peacock, A. M. Saxton, S. Mani, M. Jett, and O. R. Moss. Feasibility of assessment of regulatory lipids in breath condensate as potential presymptomatic harbingers of pulmonary pathobiology. J. Microbiol. Methods 62(3):293–302, 2005.
Wink, D. A., B. Grisham, J. B. Mitchell, and P. C. Ford. Direct and indirect effects of nitric oxide in chemical reactions relevant to biology. Methods Enzymol. 268:12–31, 1996.
Zhang, Z., and C. Kleinstreuer. Transport and uptake of MTBE and ethanol vapors in a human upper airway model. Inhal. Toxicol. 18:169–184, 2006.
Acknowledgments
The funding for this study was provided by Research Institute for Fragrance Materials (RIFM).
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Kenneth R. Lutchen oversaw the review of this article.
Appendices
Appendix A
The tissue transport reactive–diffusion equation is given by:
For small tissue concentrations below the saturable plateau for which C t ≤ C * t , Eq. (A1) is further simplified to give:
and for tissue concentrations above the saturation limit (C t > C * t ):
Equations (A2) and (A3) have to be solved during inhalation, pause, and exhalation to find tissue concentration and flux.
Inhalation and Pause
Since tissue concentration is always highest at the air–tissue interface during inhalation and pause, the same processes occur during these two time intervals. Hence, they can be combined to a single case. The governing equation for C t ≤ C * t is given by:
where
There is no vapor in the tissue at the start of the inhalation; thus at t = 0, C t = 0. In addition, tissue concentrations at both ends of the tissue layer are:
The solution to Eq. (A4) subject to initial and boundary conditions (A5) and (A6) is given by:
in which
By taking the derivative of the concentration with respect to radial distance in Eq. (A7) and time averaging over time 0 to t*, the following equation is obtained for the flux at the air–tissue interface:
where t i is the initial time. The initial time is zero if the vapor front has not reached the airway and is equal to the time the front reaching the airway if the airway is occupied by the inhaled air. The governing equation for C t > C * t is given by:
Initially tissue concentration is given by Eq. (A7) at time t = t*.
The solution to Eq. (A11) subject to initial and boundary conditions given by (A12) is:
where
and γ 2 n is defined by Eq. (25). Taking the derivative of Eq. (A13) and time averaging over the time interval (T inh − t*) leads to the following expression for the tissue flux at the air interface:
in which T inh is the inhalation time. The transition time t* can be found by equating the elimination rates from Eqs. (A7) to (A13) and solving for time t*.
Variable r in Eq. (A18) drops out when both sides of the equation are multiplied by \(\sin \frac{m \pi r}{{H_{\rm t}}} \) and integrated from 0 to H t.
The solution to Eq. (A19) can then be found numerically using Newton’s method or any similar root finding method.
Exhalation
Similar steps can be followed to find mass transfer coefficients for exhalation. However, the steps are more involved. Since the air-phase concentration is decreased during exhalation, it is safe to assume that tissue concentration drops quickly to remain unsaturated. Therefore, the governing tissue transport equation is simply:
Tissue concentration at the start of exhalation (t = T inh+pau) is equal to that at the end of pause and is given by Eq. (A7):
in which \( \bar{C}_{\rm a:t} \) corresponds to the tissue concentration at the air–tissue interface at the start of exhalation. Equation (A21) cannot be applied at r = 0 because the concentration at the interface varies over time as air-phase concentration drops and changes from \( \bar{C}_{\text{a:t}} \) to C a:t. The solution to Eq. (A20) is given by:
Taking the derivative of Eq. (A22) with respect to radial distance and time averaging during exhalation leads to the following expression for the flux:
Appendix B
We lump the mucus and tissue layers together and assume that the transport of the gas through the mucosal layer is by diffusion and reaction of saturable and first-order pathways. The governing transport equation for the chemical through the tissue layer is described by:
Tissue concentration is zero at the start of inhalation. In addition, concentration at the start of the pause is equal to that at the end of inhalation. Similarly, tissue concentration at the start of exhalation is equal to concentration at the end of the pause. Tissue concentration at the air–tissue interface is described by (see Eq. (5) for details):
Three different scenarios are simulated at the tissue–blood interface: (a) zero concentration or no resistance to vapor transport across tissue–blood barrier, (b) zero flux or no transport of the vapor across the tissue–blood interface, and (c) constant flux across the barrier or free boundary conditions in which transport from the tissue to blood compartment is dominated by vapor reaction in the tissue and diffusion through the tissue. The mathematical formulations vary slightly among the three cases and are described separately.
-
(a)
Constant concentration or C t = 0
The air-phase concentration is first solved during inhalation, pause, and exhalation and used to calculate tissue-phase concentration from Eq. (B1). The solution to Eq. (B1) is found by numerical integration. The following equation is found by dropping subscript t for simplicity and discretizing Eq. (B1) by simple implicit method using backward difference in time (j) and central difference in position (k)37:
where C a is the average concentration over airway length and may vary with time. Coefficients α and β, and function f(C j k ) are known. By writing out Eq. (B3) at time point j + 1 for k = 1 to N, the following matrix equation is obtained.
Initial and boundary conditions are now embedded in the matrix on the right-hand side of Eq. (B9). Equation (B13) can be easily solved at time j + 1 by triangularization method using Gauss elimination.
-
(b)
Constant concentration or ∂C t/∂r = 0 at r = H t
Backward differencing in time with second-order accuracy gives:
Replacing Eq. (B10) in Eq. (B3) and converting the resulting matrix to triangular form for computer implementation gives:
Equation (B11) is solved to find tissue concentration as a function of position and time during inhalation, pause, and exhalation.
-
(c)
Constant flux or ∂2 C t/∂r 2 = 0 at r = H t
A central difference representation of ∂2 C t/∂r 2 results in a negative value at the last point N because the equation is symmetric. Instead, a second-order backward difference is obtained for ∂2 C t/∂r 2 that is second-order accurate.
Setting Eq. (B12) to zero gives:
Substituting for Eq. (B13) in Eq. (B3), the following matrix equation is obtained after some manipulations.
Equation (B14) is subsequently solved to find tissue concentration.
Appendix C
Appendices A and B reported analytical and numerical approaches to computations of tissue-phase concentration of inhaled vapor in the trachea. Since the analytical solution of the tissue layer mass transfer coefficient was only feasible by approximating the saturable pathway of vapor elimination, further examination of straight-lines approximation was necessary to assess the accuracy of calculated mass transfer coefficients. Figure 2 indicated that the agreement of straight-lines approximation of the saturable pathway reaction rate with the true curve (numerical solution) depended on the parameter K m. Closer agreement was expected for low K m values at low and high concentrations. The accuracy of the straight-lines approximation of the saturable pathway of vapor elimination was further examined by comparing the approximate solution of the reaction rates (Eq. 14) with the exact curve (Eq. 2). The solutions are shown in Fig. C1 for tissue concentrations from 0 to 200 mg/m3 and k m = 1 or 201 mg/m3. Straight-lines approximation of the saturable pathway agreed reasonably well with the exact solution for low K m values. However, since the saturable pathway elimination curve for high K m values approached a plateau very slowly, straight-lines approximations of the saturable elimination pathway deviated from the actual curve at high tissue concentrations. The difference in reaction rate between straight-line approximation and the actual value reached about 50% at a tissue concentration of 200 mg/m3. Since formaldehyde is a highly reactive vapor and is eliminated from the tissue rapidly, tissue concentrations were predominantly low. While not attempted here, a larger number of lines (three or more) could be used for more accurate assessment of the reaction rate at high tissue concentrations.
Since vapor concentration in the air varied with time during pause and exhalation, mass transfer coefficients had to be calculated at small time intervals during which air-phase concentration was nearly constant. To find the optimum time interval which was a compromise between accuracy and computation time, the mass transfer coefficient was computed at different time intervals. The comparison of the predicted mass transfer coefficients during pause and exhalation for time intervals from 1.25 s down to 0.05 s is given in Fig. C2. Results indicated that the difference in mass transfer coefficients between 0.5 and 0.05 s were negligible. Hence, we selected a 0.05 s time interval for mass transfer coefficient computations.
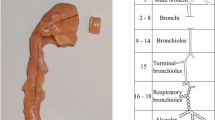
The coupled set of equations (1) and (2) were used to compute whole-lung uptake of inhaled ozone in humans using lung airway parameters from the multiple-path, particle dosimetry model (MPPD).1 Model predictions were compared with measurements of ozone uptake in humans.26 Calculations were carried out for different penetration depths of inhaled ozone with a tissue–air partition coefficient of 0.1449, and diffusion coefficients of 0.19 cm2/s in the air and 2.66 × 10−3 cm2/s in the tissue, respectively. There is no saturable pathway for ozone due to its high reactivity by first-order elimination. Thus, Eq. (2) was used without the saturable pathway route. In addition, no experimental measurements are available on the elimination rate (k f) of ozone. Figure C3 shows a comparison between model predictions and uptake measurements using k f = 106 s −1 which was estimated by Bush et al.4 In our model structure, which is significantly different than that proposed by Bush et al.4 we found that a value of k f = 105 s−1 gave a better comparison of uptake predictions with experimental measurements. Therefore, the uptake model based on the current formulation of vapor transport and uptake in the lung airway and surrounding tissues is capable of predicting uptake of vapors whose transport can be described by the set of Eqs. (1) and (2).
Comparison of predicted uptake fraction of ozone in the human lung with measurements of Nodelman and Ultman26
Rights and permissions
About this article
Cite this article
Asgharian, B., Price, O.T., Schroeter, J.D. et al. Derivation of Mass Transfer Coefficients for Transient Uptake and Tissue Disposition of Soluble and Reactive Vapors in Lung Airways. Ann Biomed Eng 39, 1788–1804 (2011). https://doi.org/10.1007/s10439-011-0274-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-011-0274-9