Abstract
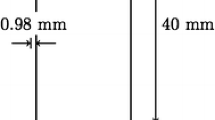
Infusion-based techniques are promising drug delivery methods for treating diseases of the nervous system. Direct infusion into tissue parenchyma circumvents the blood–brain barrier, localizes delivery, and facilitates transport of macromolecular agents. Computational models that predict interstitial flow and solute transport may aid in protocol design and optimization. We have developed a biphasic finite element (FE) model that accounts for local, flow-induced tissue swelling around an infusion cavity. It solves for interstitial fluid flow, tissue deformation, and solute transport in surrounding isotropic gray matter. FE solutions for pressure-controlled infusion were validated by comparing with analytical solutions. The influence of deformation-dependent hydraulic permeability was considered. A transient, nonlinear relationship between infusion pressure and infusion rate was determined. The sensitivity of convection-dominated solute transport (i.e., albumin) over a range of nervous tissue properties was also simulated. Solute transport was found to be sensitive to pressure-induced swelling effects mainly in regions adjacent to the infusion cavity (r/a 0 ≤ 5 where a 0 is the outer cannula radius) for short times infusion simulated (3 min). Overall, the biphasic approach predicted enhanced macromolecular transport for small volume infusions (e.g., 2 μL over 1 h). Solute transport was enhanced by decreasing Young’s modulus and increasing hydraulic permeability of the tissue.









Similar content being viewed by others
Abbreviations
- FE:
-
Finite element
- CED:
-
Convection-enhanced delivery
- CSF:
-
Cerebrospinal fluid
- a :
-
Radius of infusion cavity
- c :
-
Solute concentration in tissue
- D eff :
-
Effective diffusivity of solute in tissue
- e :
-
Volume dilatation \((=Tr(\varvec{\upvarepsilon}))\)
- E :
-
Young’s modulus
- H A :
-
Aggregate modulus (= λ + 2μ)
- k :
-
Hydraulic permeability
- M :
-
Material constant for deformation-dependent hydraulic permeability
- p :
-
Pore (interstitial) fluid pressure
- t 0 :
-
Ramping time of load
- u :
-
Displacement vector
- v :
-
Volume-averaged bulk velocity
- v c :
-
Solute velocity
- v f :
-
Intrinsic fluid velocity
- v s :
-
Solid velocity
- χ:
-
Retardation coefficient
- \(\varvec{\upvarepsilon}\) :
-
Infinitesimal deformation tensor
- ϕf :
-
Volume fraction of fluid phase; Porosity
- ϕs :
-
Volume fraction of solid phase
- λ:
-
Lamé elastic constant of solid phase
- μ:
-
Shear modulus of solid phase
- ν:
-
Poisson ratio
- \(\varvec{\upsigma}^{E}\) :
-
Contact stress tensor
- \(\varvec{\upsigma}^{f}\) :
-
Cauchy stress tensor of fluid phase
- \(\varvec{\upsigma}^{s}\) :
-
Cauchy stress tensor of solid phase
References
Barry S. I., Aldis G. K. (1992) Flow-induced deformation from pressurized cavities in absorbing porous tissues. Bull. Math. Biol. 54(6):977–997
Basser P. J. (1992) Interstitial pressure, volume, and flow during infusion into brain tissue. Microvasc. Res. 44(2):143–165
Bobo R. H., Laske D. W., Akbasak A., Morrison P. F., Dedrick R. L., Oldfield E. H. (1994) Convection-enhanced delivery of macromolecules in the brain. Proc. Natl. Acad. Sci. 91(6): 2076–2080
Bradbury M. (1979) The Concept of a Blood-Brain Barrier. New York, Wiley
Chen M. Y., Lonser R. R., Morrison P. F., Governale L. S., Oldfield E. H. (1999) Variables affecting convection-enhanced delivery to the striatum: a systematic examination of rate of infusion, cannula size, infusate concentration, and tissue-cannula sealing time. J. Neurosurg. 90(2):315–320
Chen Z.-J., Broaddus W. C., Viswanathan R. R., Raghavan R., Gillies G. T. (2002) Intraparenchymal drug delivery via positive-pressure infusion: experimental and modeling studies of poroelasticity in brain phantom gels.IEEE Trans. Biomed. Eng. 49(2):85–96
Dykstra K. H., Hsiao J. K., Morrison P. F., Bungay P. M., Mefford I. N., Scully M. M., Dedrick R. L. (1992) Quantitative examination of tissue concentration profiles associated with microdialysis. J. Neurochem. 58:931–940
Ferguson S. J., Ito K., Nolte L. P. (2004) Fluid flow and convective transport of solutes within the intervertebral disk. J. Biomech. 37:213–221
Gu W. Y., Yao H., Huang C. Y., Cheung H. S. (2003) New insight into deformation-dependent hydraulic permeability of gels and cartilage, and dynamic behavior of agarose gels in confined compression. J. Biomech 36(4): 593–598
Gurbanova A. A., Aker R., Berkman K., Onat F. Y., van Rijn C. M., van Luijtelaar G. (2006) Effect of systemic and intracortical administration of phenytoin in two genetic models of absence epilepsy. Br. J. Pharmacol 148(8):1076–1082
Holmes M. H., Mow V. C. (1990) The nonlinear characteristics of soft gels and hydrated connective tissues in ultrafiltration. J. Biomech 23(11):1145–1156
Hou J. S., Holmes M. H., Lai W. M., Mow V. C. (1989) Boundary conditions at the cartilage-synovial fluid interface for joint lubrication and theoretical verifications. J. Biomech. Eng. 111(1):78–87
Johnson E. M., Deen W. M. (1996) Hydraulic permeability of agarose gels. AIChE J 42(5):1220–1224
Johnston S. T., Deen W. M. (1999) Hindered convection of proteins in agarose gels. J. Membr. Sci. 153(2):271–279
Kaczmarek M., Subramaniam R. P., Neff S. R. (1997) The hydromechanics of hydrocephalus: steady-state solutions for cylindrical geometry. Bull. Math. Biol 59(2): 295–323
Kenyon D. E. (1979) Transient filtration in a porous elastic cylinder. ASME Trans. Series E, J. Appl. Mech. 43(4): 594–598
Kenyon D. E. (1979) A mathematical model of water flux through aortic tissue. Bull. Math. Biol 41(1):79–90
Lai W. M., Mow V. C. (1980) Drag-induced compression of articular cartilage during a permeation experiment. Biorheology. 17(1–2):111–123
Laske D. W., Morrison P. F., Lieberman D. M., Corthesy M. E., Reynolds J. C., StewartHenney P. A., Koong S. S., Cummins A., Paik C. H., Oldfield E. H. (1997) Chronic interstitial infusion of protein to primate brain: determination of drug distribution and clearance with single-photon emission computerized tomography imaging. J. Neurosurg. 87(4):586–594
Lieberman D. M., Laske D. W., Morrison P. F., Bankiewicz K. S., Oldfield E. H. (1995) Convection-enhanced distribution of large molecules in gray matter during interstitial drug infusion. J. Neurosurg. 82(6):1021–1029
Lonser R. R., Weil R. J., Morrison P. F., Governale L. S., Oldfield E. H. (1998) Direct convective delivery of macromolecules to peripheral nerves. J. Neurosurg. 89(4): 610–615
Lonser, R. R., S. Walbridge, K. Garmestani, J. A. Butman, H. A. Walters, A. O. Vortmeyer, P. F. Morrison, M. W. Brechbiel, and E. H. Oldfield. Successful and safe perfusion of the primate brainstem: in vivo magnetic resonance imaging of macromolecular distribution during infusion. J. Neurosurg. 97(4):905–913, 2002
Mauck R. L., Hung C. T., Ateshian G. A. (2003) Modeling of neutral solute transport in a dynamically loaded porous permeable gel: implications for articular cartilage biosynthesis and tissue engineering. J. Biomech. Eng 125(5): 602–614
McGuire S., Zaharoff D., Yuan F. (2006) Nonlinear dependence of hydraulic conductivity on tissue deformation during intratumoral infusion. Ann. Biomed. Eng. 34(7):1173–1181
Metz H., McElhaney J., Ommaya A. K. (1970) A comparison of the elasticity of live, dead, and fixed brain tissue. J. Biomech. 3(4):453–458
Miller K., Chinzei K. (1997) Constitutive modelling of brain tissue: Experiment and theory. J. Biomech 30(11–12):1115–1121
Morrison P. F., Chen M. Y., Chadwick R. S., Lonser R. R., Oldfield E. H. (1999) Focal delivery during direct infusion to brain: role of flow rate, catheter diameter, and tissue mechanics. Am. J. Physiol 277(4, Part 2): R1218-R1229
Morrison P. F., Laske D. W., Bobo H., Oldfield E. H., Dedrick R. L. (1994) High-flow microinfusion: tissue penetration and pharmacodynamics. Am. J. Physiol 266(1):R292-R305
Mostachfi O., Drake J. M., Tenti G., Sivaloganathan S. (1996) Realistic simple mathematical model of brain biomechanics for computer simulation of hydrocephalus and other brain abnormalities. Can J Neurol Sci 23 (Suppl. 1):S33
Mow V. C., Kuei S. C., Lai W. M., Armstrong C. G. (1980) Biphasic creep and stress-relaxation of articular-cartilage in compression – theory and experiments. J. Biomech. Eng. 102(1):73–84
Mow V. C., Holmes M. H., Lai W. M. (1984) Fluid transport and mechanical-properties of articular-cartilage – a review. J. Biomech. 17(5):377–394
Neeves K. B., Lo C. T., Foley C. P., Saltzman W. M., Olbricht W. L. (2006). Fabrication and characterization of microfluidic probes for convection enhanced drug delivery. J. Control Release 111(3):252–262
Netti P. A., Travascio F., Jain R. K. (2003). Coupled Macromolecular Transport and Gel Mechanics: Poroviscoelastic Approach. AIChE J. –Bioengineering, Food, and Products 49(6):1580–1596
Nicholson C., Sykova E. (1998) Extracellular space structure revealed by diffusion analysis. Trends Neurosci. 21: 207–215
Oomens C. W. J., van Campen D. H., Grootenboer H. J. (1987) A mixture approach to the mechanics of skin. J. Biomech 20:877–885
Pardridge W. M. (1995) Transport of small molecules through the blood-brain barrier: biology and methodology. Adv. Drug Deliv. Rev 15:5–36
Parker K. H., Mehta R. V., Caro C. G. (1987) Steady flow in porous, elastically deformable materials. ASME Trans. J. Appl. Mech 54(4):794–800
Prabhu S. S., Broaddus W. C., Gillies G. T., Loudon W. G., Chen, Z., Smith B. (1998) Distribution of macromolecular dyes in brain using positive pressure infusion: A model for direct controlled delivery of therapeutic agents. Surg. Neurol 50:367–375
Reulen H. J., Graham R., Spatz M., Klatzo I. (1977) Role of pressure gradients and bulk flow in dynamics of vasogenic brain edema. J. Neurosurg 46:24–35
Sarntinoranont M., Banerjee R. K., Lonser R. R., Morrison P. F. (2003) A computational model of direct interstitial infusion of macromolecules into the spinal cord. Ann. Biomed. Eng. 31(4):448–461
Sarntinoranont M., Chen X. M., Zhao J. B., and Mareci T. H. (2006) Computational model of interstitial transport in the spinal cord using diffusion tensor imaging. Ann. Biomed. Eng. 34(8):1304–1321
Sengers B. G., Oomens C. W. J., Baaijens F. P. T. (2004) An integrated finite-element approach to mechanics, transport and biosynthesis in tissue engineering. J. Biomech. Eng. 126(1):82–91
Simon B. R., Kaufman M. V., Liu J., Baldwin A. L. (1998) Porohyperelastic-transport-swelling theory, material properties and finite element models for large arteries. Int. J. Solids Struct. 35(34–35):5021–5031
Spilker R. L., Suh J. K., Mow V. C. (1992) A Finite-Element Analysis of the indentation stress-relaxation response of linear biphasic articular-cartilage. J. Biomech. Eng. 114(2):191–201
Sugihara-Seki M., Fu B. M. M. (2005) Blood flow and permeability in microvessels. Fluid Dyn. Res. 37(1–2):82–132
Tao L., Nicholson C. (1996) Diffusion of albumins in rat cortical slices and relevance to volume transmission. Neuroscience 75(3):839–847
Walsh E. K., Schettini A. (1976) Elastic behavior of brain-tissue in vivo. Am. J. Physiol. 230(4):1058–1062
Wood J. D., Lonser R. R., Gogate N., Morrison P. F., Oldfield E. H. (1999) Convective delivery of macromolecules into the naive and traumatized spinal cords of rats. J. Neurosurg. 90(1): 115–120
Yao H., Gu W. Y. (2004) Physical signals and solute transport in cartilage under dynamic unconfined compression: Finite element analysis. Ann. Biomed. Eng. 32(3): 380–390
Zhang X. Y., Luck J., Dewhirst M. W., Yuan F. (2000) Interstitial hydraulic conductivity in a fibrosarcoma. Am. J. Physiol.-Heart Circ. Physiol. 279(6):H2726-H2734
Acknowledgment
This study was supported in part by a grant from the National Institutes of Health (R21 NS052670).
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Analytical infusion solutions for constant pressure and constant hydraulic permeability were used for our biphasic FE validation analysis. We solved for tissue displacement for pressure-controlled infusion using the solutions for pore pressure and fluid velocity determined by Basser2
where p 0 is the constant infusion pressure, a is the radius of the infusion cavity (constant), and ω = k· H A . The Laplace transform of the radial displacement, u(r, t), was given by2
where B(s) and C(s) are unknown functions and can be determined by using the zero contact stress boundary condition, \(\varvec{\upsigma}^{E}={\mathbf{0}}\) at r = a, + ∞, and the solution of p(r,t), respectively. These were calculated to be
Substituting Eq. (A.4) into Eq. (A.3) results in
Taking the inverse Laplace transform provides the solution for displacement (Fig. 2)
Rights and permissions
About this article
Cite this article
Chen, X., Sarntinoranont, M. Biphasic Finite Element Model of Solute Transport for Direct Infusion into Nervous Tissue. Ann Biomed Eng 35, 2145–2158 (2007). https://doi.org/10.1007/s10439-007-9371-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-007-9371-1