Abstract
Background: The need for deep groin dissection when superficial nodes contain metastatic melanoma is controversial.
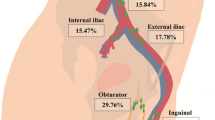
Methods: A review of 362 therapeutic groin dissections performed at our tertiary referral center between 1961 and 1995 revealed 71 patients (20%) with positive iliac and/or obturator nodes. This group was analyzed for survival rates, prognostic factors for survival, regional tumor control, and morbidity.
Results: Patients with involved deep nodes exhibited overall 5-year and 10-year survival rates of 24% (SE, 5%) and 20% (SE, 5%), respectively. Independent prognostic factors for survival were the number of positive iliac nodes (P = .0011), the Breslow thickness (P = .0069), and the site of the primary tumor (P = .0075). Patients with an unknown primary tumor seemed to have better prognoses. Seven patients (10%) experienced recurrence in the surgically treated groin. The shortand long-term morbidity rates (infection, 17%; skin flap necrosis, 15%; seroma, 17%; mild/ moderate lymphedema, 19%; severe lymphedema, 6%) compared well with those of other series studying inguinal as well as ilioinguinal dissections.
Conclusions: From the present study it can be concluded that removal of deep lymph node metastases is worthwhile, because one of every five such patients survives for 10 years. Prognostic factors for survival are the number of involved iliac nodes, the Breslow thickness, and the site of the primary tumor. Long-term regional tumor control can be obtained for 90% of the patients. The morbidity of an additional deep lymph node dissection is acceptable.
Similar content being viewed by others
REFERENCES
Slingluff CL, Stidham KR, Ricci WM, Stanley WE, Seigler HF. Surgical management of regional lymph nodes in patients with melanoma. Ann Surg 1994;219:120–1230.
Miliotes G, Albertini J, Berman C, et al. The tumor biology of melanoma nodal metastases. Am Surg 1996;62:81–88.
Ross MI. Surgical management of stage I and II melanoma patients: approach to the regional lymph node basin. Semin Surg Oncol 1996;12:394–401.
Balch CM, Soong SJ, Bartolucci AA, et al. Efficacy of an elective regional lymph node dissection of 1 to 4 mm thick melanomas for patients 60 years of age and younger. Ann Surg 1996;224:255–263 (discussion, 263–6).
Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992;127:392–399.
Ross MI, Balch CM. General principles of regional lymphadenectomy. In: Balch CM, Houghton AN, Milton GW, Sober AJ, Soong S, eds. Cutaneous melanoma, 2nd edn. Philadelphia: Lippincott, 1992:339–344.
Singletary SE, Shallenberger R, Guinee VF. Surgical management of groin nodal metastases from primary melanoma of the lower extremity. Surg Gynecol Obstet 1992;174:195–200.
Balch CM, Soong SJ, Shaw HM, Urist MM, McCarthy WH. An analysis of prognostic factors in 8500 patients with Cutaneous melanoma. In: Balch CM, Houghton AN, Milton GW, Sober AJ, Soong S, eds. Cutaneous melanoma, ed. 2. Philadelphia: Lippincott, 1992:165–187.
Karakousis CP, Driscoll DL, Rose B, Walsh DL. Groin dissection in malignant melanoma. Ann Surg Oncol 1994;1:271–277.
Beitsch P, Balch CM. Operative morbidity and risk factor assessmentin melanoma patients undergoing inguinal lymph node dissection. Am J Surg 1992;164:462–466.
Coit DG. Extent of groin dissection for melanoma. Surg Oncol Cin North Am 1992;1:271–280.
Fink SJ, Guiliano AE, Mann BD, Morton DL. Results of ilioinguinal dissection for stage II melanoma. Ann Surg 1982;196:180–186.
Coit DG, Brennan MF. Extent of lymph node dissection in melanomaof the trunk or lower extremity. Arch Surg 1989;124:162–166.
Karakousis CP, Driscoll DL. Groin dissection in malignant melanoma.Br J Surg 1994;81:1771–1774.
Jonk A, Kroon BBR, Ru¨mke Ph van der Esch EP, Hart AAM. Results of radical dissection of the groin in patients with stage II melanoma and histologically proved metastases of the iliac or obturator lymph nodes, or both. Surg Gynecol Obstet 1988;167:28–32.
Karakousis CP, Driscoll DL. Positive nodes in the groin and survival in malignant melanoma. Am J Surg 1996;171:421–422.
Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika 1982;69:239–241.
Wright P. Adjusted P-values for simultaneous inference. Biometrics 1992;48:1005–1013.
Drepper H, Biess B, Hoffherr B, et al. The prognosis of patients with stage III melanoma. Cancer 1993;71:1239–1246.
Reintgen DS, Tso CY, Seigler HF. Prognosis for recurrent malignant melanoma. Ann Plast Surg 1992;28:81–84.
Buzaid AC, Tinoco LA, Jendiroba D, et al. Prognostic value of size of lymph node metastases in patients with cutaneous melanoma. J Clin Oncol 1995;13:2361–2368.
Norman J, Cruse CW, Wells KE, Saba HI, Reintgen DS. Metastatic melanoma with an unknown primary. Ann Plast Surg 1992;28:81–84.
Lopez R, Holyoke ED, Moore RH, Karakousis CP. Malignant melanoma with unknown primary site. J Surg Oncol 1982;19:151–154.
Chang P, Knapper WH. Metastatic melanoma of unknown primary.Cancer 1982;49:1106–1111.
Schlagenhauff B, Stroebel W, Ellwanger U, et al. Metastatic melanoma of unknown primary origin shows prognostic similarities to regional metastatic melanoma: recommendations for initial staging examinations. Cancer 1997;80:60–65.
Law MM, Wong JH. Evaluation of the prognostic significance of the site of origin of cutaneous melanoma. Am Surg 1994;60:362–366.
Jonk A, Kroon BBR, Rümke Ph, Mooi WJ, Hart AAM, van Dongen JA. Lymph node metastasis from melanoma with an unknown primary site. Br J Surg 1990;77:665–668.
Buzaid AC, Ross MI, Balch CM, et al. Critical analysis of the current American Joint Committee on Cancer staging system for cutaneous melanoma and proposal of a new staging system. J Clin Oncol 1997;15:1039–1051.
Das Gupta TK. Results of treatment of patients with primary cutaneous melanoma. Ann Surg 1977;186:201–205.
Illig L, Aigner KR, Biess B, et al. Diagnostic excision of the Rosenmu¨ller’s node. Cancer 1988;61:1200–1206.
Coit DG, Rogatko A, Brennan MF. Prognostic factors in patients with melanoma metastatic to axillary or inguinal nodes: a multivariate analysis. Ann Surg 1991;214:627–636.
Kuvshinov BW, Kurtz C, Coit DG. Computed tomography in evaluation of patients with stage III melanoma. Ann Surg Onco1997;4:252–258.
Horgan K, Hughes LE. Staging of melanoma. Clin Radiol 1993;48:297–300.
Holmes EC, Moseley HS, Morton DL, Clark W, Robinson D, Urist MM. A rational approach to the surgical management of melanoma. Ann Surg 1977;186:481–490.
Shaw JH, Koea J. Morbidity of lymphadenectomy for melanoma. Surg Oncol Clin North Am 1992;1:195–203.
Ames FC, Singletary SE. Cutaneous malignancies of the trunk and lower extremities. In: Johnson DE, Ames FC, eds. Groin dissection. Chicago: Mosby-Year Book, 1985:111–137.
Bowsher WG, Taylor BA, Hughes LE. Morbidity, mortality and local recurrence following regional node dissection for melanoma. Br J Surg 1986;73:906–908.
Baas PC, Schraffordt Koops H, Hoekstra HJ, et al. Groin dissection in the treatment of lower-extremity melanoma. Arch Surg 1992;127:281–286.
Kapteijn BAE, Nieweg OE, Liem IH, et al. Localizing the sentinel node in cutaneous melanoma: gamma probe detection versus bluedye. Ann Surg Oncol 1997;4:156–160.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Strobbe, L.J.A., Jonk, A., Hart, A.A.M. et al. Positive Iliac and Obturator Nodes in Melanoma: Survival and Prognostic Factors. Ann Surg Oncol 6, 255–262 (1999). https://doi.org/10.1007/s10434-999-0255-5
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10434-999-0255-5