Abstract
Menorrhagia is the presenting symptom among the majority of women who undergo hysterectomy. The levonorgestrel intrauterine system (LNG-IUS) is highly effective in reducing menstrual bleeding. The aim of this randomized study was to compare the effect of endometrial resection (ER) as a surgical modality and the LNG-IUS as a hormonal modality for treating menorrhagia. This is a therapeutic, phase III randomized study that included 60 premenopausal women with excessive uterine bleeding. The patients were randomly allocated to two treatment groups – LNG-IUS or endometrial resection (ER). Uterine bleeding was quantified by the pictorial blood loss assessment score (PBAC). The degree of disturbance caused by menstrual bleeding on general well-being, work performance, physical activity and sexual activity was assessed using a visual analogue scale at screening. Initial evaluation was followed by reassessment at 6 months, and at 12 months or at discontinuation. Both groups were matched for age, duration of flow and uterine characteristics. In the LNG-IUS group, four patients discontinued treatment and, ultimately, treatment success was 77%. In the ER Group, all operations were uneventful. A significant reduction in the amount of blood loss monthly was achieved in 83% of the cases, and there was a significant improvement in the quality of life of the patients in both study groups. The difference between the two groups was not statistically significant (p=0.747). The placement of LNG-IUS has a dramatic effect in lowering bleeding intensity in menorrhagic patients, with the advantage of reversibility, and mild adverse events. It may be the first-line treatment in younger women with menorrhagia.
Similar content being viewed by others
Introduction
Menorrhagia is a prevalent cause of ill health in women worldwide, with about one third of all women reporting heavy menstrual bleeding at some time in their lives. It is the presenting symptom among the majority of women who undergo hysterectomy, and recent data suggest that menorrhagia is becoming an increasingly common health problem [1].
Cole et al. [2] suggested that excess menstruation should be considered to be present when more than 80 ml of blood is lost per cycle. However, the initial complaint of menorrhagia is a subjective one and most often originates from the woman’s perceived menstrual loss. One study has shown that 40% of women with an objectively measured menstrual loss of more than 80 ml report that their periods are either light or moderate [3]. In a study in women with iron-deficiency anaemia due to menorrhagia, only 15% described their periods as heavy [4]. At the other end of the spectrum, it has also been reported that 26–38% of women complaining of heavy periods had objective menstrual losses of less than 80 ml per cycle [5].
Twenty years ago 60% of patients with menorrhagia who were referred to a gynaecologist had a hysterectomy as treatment [6]. Endometrial ablation was first described in the UK in 1989 and has since become a viable surgical alternative to hysterectomy. The levonorgestrel intrauterine system (LNG-IUS; Mirena, Schering Health, Berlin, Germany) is highly effective in reducing menstrual bleeding and has been shown to reduce the numbers of patients ultimately undergoing surgical treatment in the form of a hysterectomy [6].
The LNG-IUS, a steroid-releasing intrauterine system, is a T-shaped device that releases levonorgestrel directly into the uterine cavity at an initial rate of 20 μg per day. The contraceptive and therapeutic benefits of the LNG-IUS stem primarily from its local effects. The local hormone delivery results in high levonorgestrel levels in the endometrial tissue but low levels in the systemic circulation. This leads to strong endometrial suppression and, in many cases, a dramatic reduction in menstrual blood loss (MBL). Extensive international clinical research has documented the high contraceptive efficacy of this device [7].
A Cochrane review has been published on the use of progestogen-releasing intrauterine systems for the treatment of menorrhagia. Based on comparisons of these systems against other treatments for menorrhagia, the authors report that the former are more effective than 21 days of oral progestagens for the treatment for menorrhagia. In general, women are more satisfied with IUS and are more likely to continue with this system than with medical treatments. They are, however more likely to suffer side effects with LNG-IUS than with other medical treatments [8].
The objective to treating a patient with menorrhagia is to alleviate heavy menstrual flow and, consequently, to improve the quality of life. Iron-deficiency anaemia must also be prevented. The guidelines for the management of menorrhagia in secondary care published by the Royal College of Obstetricians and Gynecologists (RCOG) recommend bimanual examination and transvaginal sonography (TVS) followed by endometrial biopsy – after it has been shown that prior drug treat of menorrhagia has failed. If these recommendations are widely implemented, progestogen-releasing intrauterine devices (IUD) will become one of three options with second line drugs and surgical treatment. Endometrial ablation and hysterectomy are the other two surgical options [9].
The aim of this randomized study was to compare the effect of endometrial resection (ER) as a surgical modality and the LNG-IUS as a hormonal modality for treating menorrhagia. Adverse events associated with both approaches are assessed.
Materials and methods
Patients
Patients enrolled into the study were recruited from premenopausal women who had spontaneous cycles and who were scheduled to undergo hysterectomy for treatment of excessive uterine bleeding with or without dysmenorrhoea. Failed attempts at conservative medical treatment were reported by 80% of the women questioned. The other patients entered the study directly without previous medication. Inclusion criteria included age between 40 and 50 years, a regular uterine cavity <10 cm in length as measured by ultrasound and no wish for further pregnancy.
Women were excluded from the study if they had one fibroid larger than 3 cm in diameter or more than three uterine fibroids as assessed by ultrasonography, a history or current clinical evidence or suspicion of malignancy or active liver disease, adnexal tumours or cysts or pelvic inflammatory disease within the previous 12 months.
Study design
The study was designed as an open, therapeutic, phase III randomized comparative study with an LNG-IUS group and an ER group, each consisting of 30 patients. The study was conducted in Kasr El-Aini Hospital, Cairo University (Egypt). An informed consent was obtained from each woman. The women were randomly allocated to the LNG-IUS or ER group using a randomization table. Concealment was secured by using sealed envelopes.
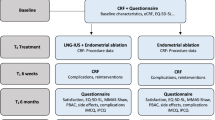
Evaluation
Uterine bleeding was quantified by the semiquantitative pictorial blood loss assessment score (PBAC), which was completed by all subjects over a screening period of 2 months prior to enrollment [10]. The score is recorded on a chart on which the patient registers the number of sanitary pads used each day, the degree of soiling on each pad, the number and size of clots passed and episodes of flooding. A monthly score of >100 on this chart is regarded as excessive bleeding.
The degree of disturbance caused by menstrual bleeding or pain, or both, on general well-being, work performance, physical activity and sexual activity was assessed using an EuroQol-visual analogue scale (EQ-VAS) at screening, at 6 months and at 12 months or at discontinuation. The EQ-VAS offers a simple method for obtaining self-rated scores of current health status. The VAS scale used is a vertical 20-cm scale, with endpoints of 100 (‘best imaginable health state’) at the top and 0 (‘worst imaginable health state’) at the bottom. The respondent was asked to rate her current health state on the EQ-VAS by drawing a line to the appropriate point on the EQ-VAS.
The evaluation of the uterus was evaluated by means of transvaginal ultrasound followed by hysteroscopy of the cavity to exclude intrauterine pathology. An endometrial biopsy was performed in all cases. No pretreatment to suppress the endometrium was given.
Treatment trial
The LNG-IUS (Mirena) was inserted into the uterine cavity following menstruation according to the insertion instructions. All endometrial resections were conducted under general anesthesia. The cervical canal was dilated to Hegar 11, and a Stortz rigid resectoscope (Stortz, Tuttlingen, Germany) equipped with a Hopkins 27005 B 30° optic (Stortz) was passed into the uterine cavity. Glycine (1.5%) was infused for irrigation. A mixed diathermal current of 120 W was routinely used for resection of the endometrium. For haemostasis, a coagulation current of 80 W was applied.
Follow-up and outcome measures
The patients were followed at the outpatient clinic with visits scheduled at 6 months and 12 months after the operation or the insertion of the IUD. The PBAC for the preceding months were collected at each follow-up visit. The patients had a gynaecological examination, and their weight and blood pressure was controlled. No additional treatment for menorrhagia was allowed during the study period.
The primary measure of efficacy was the woman’s decision at 6 months or at discontinuation. If she chose to continue the current treatment she was asked again at 12 months. Treatment success was defined as a PBAC score of <75 at 12 months. Treatment failure was defined as a PBAC score of >75, removal of the intrauterine device in the LNG-IUS group or resurgery for any reason in the ER group. Any adverse event occurring after treatment was recorded whether local or generalized. In the ER group, only barrier methods were allowed for anti-contraception.
Statistical analysis
Continuous variables were expressed as the mean ± standard deviation (SD), median, minimum and maximum. Qualitative data were expressed as frequency and percentage. For the quantitative data, a comparison between the two groups was carried out using the Studentt-test or Mann-Whitney U-test, as appropriate. The chi-square test was used to compare qualitative data. The level of significance was set at p<0.05. We expected a success rate of 85% in the LNG-IUS group and 70% in the ER group. The sample size required at the 5% level, when the power is 90, was 30 per group.
Results
The demographic data and gynaecological histories of the 60 patients treated by either LNG-IUS or by ER revealed no differences in average age and uterine cavity depth. However there was a difference for parity (Table 1).
LNG-IUS group
No complications occurred during the insertions of the IUDs. Dilatation of the cervix was needed in three cases. Four patients discontinued treatment during the follow-up period: three because of irregular bleeding or spotting after insertion and one because of pain. Of the 26 patients still retaining the LNG-IUS after 12 months, 23 (88%) showed a significant reduction in monthly blood loss, as assessed with the PBAC (Table 1), and treatment success was thus achieved in 77% of the original LNG-IUS cohort. The four patients who discontinued treatment subsequently underwent a successful endometrial resection. Seven patients reported one or more local adverse events: metrorrhagia (n=2), pelvic pain (n=3) and vaginal discharge (n=4). Ten patients reported generalized symptoms, including abdominal pain (n=5), breast tenderness (n=3), headache (n=2), acne (n=2) and mood changes (n=1).
ER group
All operations were uneventful. The mean operating time was 34.8 min. Nine patients reported one or more local pelvic adverse events: pelvic pain and local tenderness indicating inflammation (n=4), bleeding (n=5), vaginitis (n=2) and genital ulceration (n=1). One patient reported abdominal pain, and one patient had a repeat ER because of haematometra.
Of the 30 patients who underwent an endometrial resection, 25 (83%) showed a significant reduction of monthly blood loss 12 months after the operation, with the median monthly blood loss reduced from 385 to 45 mL.
Comparison of groups
There was no difference between the groups with regard to baseline variables, including the median PBAC score (Tables 1, 2).
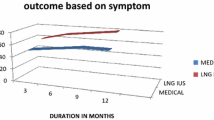
Blood loss
Treatment success at 12 months was achieved in 23 (77%) of the 30 patients in the LNG-IUS group and in 25 (83%) of the patients in the ER group. The difference is not statistically significant (p=0.747). The bleeding pattern of the two groups is outlined in Table 3 and shown in Fig. 1. The rate of amenorrhea was higher in the LNG-IUS group, but there was no statistically significant difference between the two groups (p=1.000).
The median VAS score for each of the four items of the EQ-VAS score is shown in Table 4. There was a significant improvement for all four items in the two study groups. Figure 2 shows the magnitude of improvement in the two groups for comparison purposes. A greater improvement was observed in the LNG-IUS patients for the items of general well-being and sexual activity, while the median scores for the items of improvement of work performance and physical activity were slightly higher in the ER group.
Discussion
The ideal approach to diagnosing menorrhagia should be readily available, inexpensive and able to measure actual blood loss. However, to date no such test exists. Attempts have been made to increase the accuracy of diagnosing menorrhagia using PBACs. Initial studies have demonstrated a sensitivity and specificity of >80% for a PBAC score of >100 [10]. Other reports have demonstrated that the same sensitivity and specificity can be achieved, but with a cut-off point of 185 [11]; still more recently one study has reported that there is no correlation between the observed PBAC and actual measured blood loss [12]. The advantage of the PBAC is that it does provide semi-objective comparative information in the absence of a more valid and reliable test. In our study, we employed PBAC scores as the semi-quantitative means for assessing MBL in the study group.
We found a dramatic decrease in blood loss in the two groups of patients following treatment. In 1998, Kittelsen and Istre [13] performed a randomized study quite similar to the present study with the aim of identifying the effect of the two approaches – LNG-IUS and transcervical resection of the endometrium – for the treatment of menorrhagia. These researchers reported a significant drop in the PBAC score, which was used to assess bleeding intensity, in the two study groups. In addition, they concluded that an addition advantage of the LNG-IUS is that it is reversible and has no operative hazards or side-effects. Another similar study by Istre and Trolle [14] reported a treatment success rate of 67% in 30 patients treated with LNG-IUS and in 90% of 29 patients treated with transcervical resection at the 12-month follow-up.
Rauramo et al. [15] studied the long-term efficacy of the LNG-IUS and transcervical resection of the endometrium in the treatment of menorrhagia in an open, randomized 3-year trial. They concluded that both treatments efficiently reduced menstrual bleeding. Of the 30 women using the LNG-IUS, 19 completed the 3-year follow-up in comparison with 22 of 29 women who had undergone transcervical resection of the endometrium.
In the present study, the rate of amenorrhea in the LNG-IUS group was 53.8%, which was higher than that in the ER group (43.3%), but the difference is not statistically significant. Following transcervical endometrial resection, amenorrhoea rates of between 26 and 40% have been reported [16, 17], with an 85% improvement in those continuing to menstruate.
In a Cochrane systematic review, Lethaby et al. [18] included nine randomized controlled trials – all between 1980 and 2005 – in women of reproductive age treated with progesterone or progestogen-releasing IUDs versus no treatment, placebo or other medical or surgical therapy for heavy menstrual bleeding. The LNG-IUS was compared with oral cyclical norethisterone, transcervical resection of the endometrium or balloon ablation. Lethaby et al. concluded that the LNG-IUS is more effective than cyclical norethisterone as a treatment for heavy menstrual bleeding. Women with an LNG-IUS are more satisfied with the results of the treatment and more willing to continue with the treatment, but they also experience more side effects, such as intermenstrual bleeding and breast tenderness. The LNG-IUS resulted in a smaller mean reduction in MBL (as assessed by the PBAC chart) than endometrial ablation but there was no evidence of a difference in the rate of satisfaction with treatment.
The results found in the present study imply that the LNG-IUS may be applicable for treating 70–80% of patients scheduled for operative procedures. The result of this study has clearly demonstrated that both LNG-IUS and ER reduce menstrual blood loss. Although both methods seem to be equally effective in reducing MBL, ER is an invasive procedure requiring operative equipment and an operation theatre, while the placement of the LNG-IUS can be carried out in the outpatient department. This is in line with other studies that found that 64% of 28 women scheduled for hysterectomy due to bleeding problems could cancel their decision to undergo hysterectomy, compared with 14% in the control group [19]. Another aspect is the reversibility of the treatment and potential return of fertility associated with the LNG-IUS.
Menorrhagia has a detrimental impact on the quality of life and can adversely affect the physical and mental health of the sufferer. It is also associated with disruption to vocational, family and social life [20]. It is difficult for the clinician to assess the importance of the above disruptions to an individual patient and, therefore, to tailor the best treatment to her needs.
We found a significant improvement in the four items studied as indicators of the quality of life of the patients. These items include general well-being, work performance, physical activity and sexual activity. There was no significant difference between the two study groups with respect to the magnitude of improvement of the median VAS of these four items. What is apparent is that quality of life is improved after any treatment for menorrhagia, with this improvement being the least with medical interventions [21, 22] and the greatest with hysterectomy. Endometrial ablation offers a significant improvement in quality of life with either first-generation or second-generation techniques, although it will be less than that provided by a hysterectomy. The improvement in the quality of life from the use of a medicated IUD device lies between that achieved with medical and ablation treatments.
Adverse events were more frequently reported in the LNG-IUS group (n=14) than in the ER group (n=11). The difference is not statistically significant, and all of the reported effects were rather mild and not a reason for discontinuing the treatment in the LNG-IUS group.
To conclude, the LNG-IUS is a contraceptive that is able to substantially decrease bleeding intensity in menorrhagic patients. It is further characterized by reversibility and may be the first-line treatment in younger women with menorrhagia. In addition, the adverse events are mild and few owing to its low systemic steroidal dose. Endometrial resection implies the use of operation facilities, is irreversible and often requires a new operation if the first treatment fails. Overall, the tolerability of both treatments is good.
References
Hurskainen R, Teperi J, Rissanen P et al (2004) Clinical outcomes and costs with the levonorgestrel-releasing intrauterine system or hysterectomy for treatment of menorrhagia: randomized trial 5-year follow-up. JAMA 291:1456–1463
Cole SK, Billewicz WZ, Thomson AM (1971) Sources of variation in menstrual blood loss. J Obstet Gynaecol Br Commonw 78:933–939
Hallberg L, Hogdahl AM, Nilsson L et al (1966) Menstrual blood loss-a population study. Variation at different ages and attempts to define normality. Acta Obstet Gynaecol Scand 45:320–351
McKenna DM, Dockeray CJ, McCann X (1989) Iron deficiency anaemia in pre-menopausal women. Ir Med J 82:69–70
Fraser IS, McCarron G, Markham R (1984) A preliminary study of factors influencing perception of menstrual blood loss volume. Am J Obstet Gynecol 149:788–793
Reid PC, Mukri F (2005) Trends in number of hysterectomies performed in England for menorrhagia: examination of health episode statistics, 1989 to 2002-2003. BMJ 330:938–939
Jensen JT (2005) Contraceptive and therapeutic effects of the levonorgestrel intrauterine system: an overview. Obstet Gynecol Surv 60:604–612
Lethaby A, Cook I, Rees M (2000) Progesterone/progesterone releasing intrauterine systems versus either placebo or any other medication for heavy menstrual bleeding (Cochrane review). In: The Cochrane Library, Issue 3
RCOG green top guidelines on the secondary management of menorrhagia. http://www.rcog.org.uk
Higham J, O’Brien PM, Shaw RW (1990) Assessment of menstrual blood loss using a pictorial chart. Br J Obstet Gynaecol 97:734–739
Janssen CA, Scholten PC, Heintz AP (1995) A simple visual assessment technique to discriminate between menorrhagia and normal menstrual blood loss. Obstet Gynecol 85:977–982
Reid PC, Coker A, Coltart R (2000) Assessment of menstrual blood loss using a pictorial chart: a validation study. Br J Obstet Gynaecol 107:320–322
Kittelsen N, Istre O (1998) A randomized study comparing levonorgestrel intrauterine system (LNG IUS) and transcervical resection of the endometrium (TCRE) in the treatment of menorrhagia: preliminary results. Gynaecol Endosc 7:61–65
Istre O, Trolle B (2001) Treatment of menorrhagia with the levonorgestrel intrauterine system versus endometrial resection. Fertil Steril 76:304–309
Rauramo I, Elo I, Istre O (2004) Long-term treatment of menorrhagia with levonorgestrel intrauterine system versus endometrial resection. Obstet Gynecol 104:1314–1321
O’Connor H, Magos A (1996) Endometrial resection for the treatment of menorrhagia. Lancet 335:151–156
Hart R, Magos A (1997) Endometrial ablation. Curr Opin Obstet Gynecol 9:226–232
Lethaby A, Cooke I, Rees M (2005) Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev 2005:CD002126
Chi IC, Farr G (1994) The non-contraceptive effects of the levonorgestrel releasing intrauterine device. Adv Contracept 10:271–285
Shaw RW, Brickley MR, Evans L et al (1998) Perceptions of women on the impact of menorrhagia on their health using multi-attribute utility assessment. Br J Obstet Gynaecol 105:1155–1159
Coulter A, Peto V, Jenkinson C (1994) Quality of life and patient satisfaction following treatment for menorrhagia. Fam Pract 11:394–401
Cooper KG, Parkin DE, Garratt AM et al (1997) A randomised comparison of medical and hysteroscopic management in women consulting a gynaecologist for the treatment of heavy menstrual loss. Br J Obstet Gynaecol 104:1360–1366
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdel Malak, K., Shawki, O. Management of menorrhagia with the levonorgestrel intrauterine system versus endometrial resection. Gynecol Surg 3, 275–280 (2006). https://doi.org/10.1007/s10397-006-0234-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-006-0234-9