Abstract
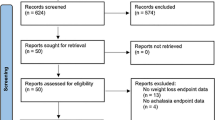
Pseudoachalasia, also known as secondary achalasia, is a clinical condition mimicking idiopathic achalasia but most commonly caused by malignant tumors of gastroesophageal junction (GEJ). Our aim was to systematically review and present all available data on demographics, clinical features, and diagnostic modalities involved in patients with pseudoachalasia. A systematic search of literature published during the period 1978–2019 was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (end-of-search date: June 25th, 2019). Two independent reviewers extracted data with regards of study design, interventions, participants, and outcomes. Thirty-five studies met our inclusion criteria and were selected in the present review. Overall, 140 patients with pseudoachalasia were identified, of whom 83 were males. Mean patient age was 60.13 years and the mean weight loss was 13.91 kg. A total of 33 (23.6%) patients were wrongly ‘treated’ at first for achalasia. The most common presenting symptoms were dysphagia, food regurgitation, and weight loss. The median time from symptoms’ onset to hospital admission was 5 months. Most common etiology was gastric cancer (19%). Diagnostic modalities included manometry, barium esophagram, endoscopy, and computed tomography (CT). Pseudoachalasia is a serious medical condition that is difficult to be distinguished from primary achalasia. Clinical feature assessment along with the correct interpretation of diagnostic tests is nowadays essential steps to differentiate pseudoachalasia from idiopathic achalasia.

Similar content being viewed by others
References
Ogilvie H. The early diagnosis of cancer of the oesophagus and stomach. Br Med J. 1947;2:405–7.
Kahrilas PJ, Kishk SM, Helm JF, et al. Comparison of pseudoachalasia and achalasia. Am J Med. 1987;82:439–46.
Bonavina L, Fociani P, Asnaghi D, et al. Synovial sarcoma of the esophagus simulating achalasia. Dis Esophagus. 1998;11:268–71.
Moonka R, Patti MG, Feo CV, et al. Clinical presentation and evaluation of malignant pseudoachalasia. J Gastrointest Surg. 1999;3:456–61.
Roman S, Kahrilas PJ. Pseudoachalasia and laparoscopic gastric banding. J Clin Gastroenterol. 2011;45:745–7.
Brown WR, Dee E. Dysphagia in a patient with recurrent small-cell lung cancer. Gastroenterology. 2013;144(34):252–3.
Tracey JP, Traube M. Difficulties in the diagnosis of pseudoachalasia. Am J Gastroenterol. 1994;89:2014–8.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Campo SM, Lorenzetti R, de Matthaeis M, et al. Palliation with oesophageal metal stent of pseudoachalasia from gastric carcinoma at the cardia: a case report. Diagn Ther Endosc. 2009;2009:791627.
Lahbabi M, Ihssane M, Sidi Adil I, et al. Pseudoachalasia secondary to metastatic breast carcinoma mimicking radiation stenosis. Clin Res Hepatol Gastroenterol. 2012;36:e117–e12121.
Lazaraki G, Nakos A, Katodritou E, et al. A rare case of multiple myeloma initially presenting with pseudoachalasia. Dis Esophagus. 2009;22:E21–E2424.
Losh JM, Sanchez B, Waxman K. Refractory pseudoachalasia secondary to laparoscopically placed adjustable gastric band successfully treated with Heller myotomy. Surg Obes Relat Dis. 2017;13:e4–e8.
Mainprize KS, Dehn TC. Laparoscopic management of pseudoachalasia, esophageal diverticulum, and benign esophageal stromal tumor. Dis Esophagus. 2001;14:73–5.
Mizrak D, Alkan A, Erdogdu B, et al. Osteogenesis imperfecta, pseudoachalasia, and gastric cancer. Case Rep Gastrointest Med. 2015;2015:685459.
Roushan N, Zolfaghari A, Asadi M, et al. Pseudoachalasia: a diagnostic challenge. Med J Islam Repub Iran. 2014;28:54.
Paulsen JM, Aragon GC, Ali MA, et al. Pseudoachalasia secondary to metastatic breast carcinoma. Dig Dis Sci. 2010;55:1179–81.
Moorman AJ, Oelschlager BK, Rulyak SJ. Pseudoachalasia caused by retroperitoneal B-cell lymphoma. Clin Gastroenterol Hepatol. 2008;6:A32.
Portale G, Costantini M, Zaninotto G, et al. Pseudoachalasia: not only esophago-gastric cancer. Dis Esophagus. 2007;20:168–72.
Campos CT, Ellis FH Jr, LoCicero J 3rd. Pseudoachalasia: a report of two cases with comments on possible causes and diagnosis. Dis Esophagus. 1997;10:220–4.
Ravi K, Sweetser S, Katzka DA. Pseudoachalasia secondary to bariatric surgery. Dis Esophagus. 2016;29:992–5.
Roark G, Shabot M, Patterson M. Achalasia secondary to hepatocellular carcinoma. J Clin Gastroenterol. 1983;5:255–8.
Seki H, Matsumoto K, Ohmura K, et al. Malignant pleural mesothelioma presenting as achalasia. Intern Med. 1994;33:624–7.
Seo P. Cases from the Osler Medical Service at Johns Hopkins University. Pseudoachalasia due to esophageal adenocarcinoma. Am J Med. 2002;113:522–4.
Shaikh S, Dexter SP, Jameel JK. Esophageal rupture: a pseudo-achalasia related delayed complication after laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2014;10:e27–e2929.
Song CW, Chun HJ, Kim CD, et al. Association of pseudoachalasia with advancing cancer of the gastric cardia. Gastrointest Endosc. 1999;50:486–91.
Sousa RG, Figueiredo PC, Pinto-Marques P, et al. An unusual cause of pseudoachalasia: the Alport syndrome-diffuse leiomyomatosis association. Eur J Gastroenterol Hepatol. 2013;25:1352–7.
Stone ML, Kilic A, Jones DR, et al. A diagnostic consideration for all ages: pseudoachalasia in a 22-year-old male. Ann Thorac Surg. 2012;93:e11–e12.
Ter RB, Govil YK, Leite L, et al. Adenosquamous carcinoma in Barrett's esophagus presenting as pseudoachalasia. Am J Gastroenterol. 1999;94:268–70.
Thomas LA, Balaratnam N, Richards DG, et al. Diffuse esophageal leiomyomatosis: another cause of pseudoachalasia. Dis Esophagus. 2000;13:165–8.
Ray S, Saluja SS, Gupta R, et al. Esophageal leiomyomatosis—an unusual cause of pseudoachalasia. Can J Gastroenterol. 2008;22:187–9.
Tucker HJ, Snape WJ Jr, Cohen S. Achalasia secondary to carcinoma: manometric and clinical features. Ann Intern Med. 1978;89:315–8.
Ulla JL, Fernandez-Salgado E, Alvarez V, et al. Pseudoachalasia of the cardia secondary to nongastrointestinal neoplasia. Dysphagia. 2008;23:122–6.
Wang AJ, Tu LX, Yu C, et al. Achalasia secondary to cardial tuberculosis caused by AIDS. J Dig Dis. 2015;16:752–3.
Woods CA, Foutch PG, Waring JP, et al. Pancreatic pseudocyst as a cause for secondary achalasia. Gastroenterology. 1989;96:235–9.
Yeoman LJ, Grundy A, Parker MC, et al. Pseudoachalasia after radical gastrectomy. Br J Surg. 1989;76:97–8.
Gockel I, Eckardt VF, Schmitt T, et al. Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroenterol. 2005;40:378–85.
Bholat OS, Haluck RS. Pseudoachalasia as a result of metastatic cervical cancer. Jsls. 2001;5:57–62.
Kahlberg A, Marrocco-Trischitta MM, Marone EM, et al. An unusual case of dysphagia after endovascular exclusion of thoracoabdominal aortic aneurysm. J Endovasc Ther. 2009;16:238–42.
Khan A, Ren-Fielding C, Traube M. Potentially reversible pseudoachalasia after laparoscopic adjustable gastric banding. J Clin Gastroenterol. 2011;45:775–9.
Katzka DA, Farrugia G, Arora AS. Achalasia secondary to neoplasia: a disease with a changing differential diagnosis. Dis Esophagus. 2012;25:331–6.
Kotoulas C, Galanis G, Yannopoulos P. Secondary achalasia due to a mesenchymal tumour of the oesophagus. Eur J Surg Oncol. 2000;26:425–7.
Ponce J, Garrigues V, Nos P, et al. Esophageal pseudoachalasia related to a neoplasm. Rev Esp Enferm Dig. 1993;83:1–4.
Liu W, Fackler W, Rice TW, et al. The pathogenesis of pseudoachalasia: a clinicopathologic study of 13 cases of a rare entity. Am J Surg Pathol. 2002;26:784–8.
Abubakar U, Bashir MB, Kesieme EB. Pseudoachalasia: a review. Niger J Clin Pract. 2016;19:303–7.
Taft TH, Carlson DA, Triggs J, et al. Evaluating the reliability and construct validity of the Eckardt symptom score as a measure of achalasia severity. Neurogastroenterol Motil. 2018;30:e13287.
Hirano I, Tatum RP, Shi G, et al. Manometric heterogeneity in patients with idiopathic achalasia. Gastroenterology. 2001;120:789–98.
Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013;108:1238–49.
Woodfield CA, Levine MS, Rubesin SE, et al. Diagnosis of primary versus secondary achalasia: reassessment of clinical and radiographic criteria. AJR Am J Roentgenol. 2000;175:727–31.
Zagouri F, Sergentanis TN, Bartsch R, et al. Intrathecal administration of trastuzumab for the treatment of meningeal carcinomatosis in HER2-positive metastatic breast cancer: a systematic review and pooled analysis. Breast Cancer Res Treat. 2013;139:13–22.
Zagouri F, Sergentanis TN, Azim HA Jr, et al. Aromatase inhibitors in male breast cancer: a pooled analysis. Breast Cancer Res Treat. 2015;151:141–7.
Zagouri F, Sergentanis TN, Chrysikos D, et al. Fulvestrant and male breast cancer: a pooled analysis. Breast Cancer Res Treat. 2015;149:269–75.
Zagouri F, Kastritis E, Gavriatopoulou M, et al. Lenalidomide in patients with POEMS syndrome: a systematic review and pooled analysis. Leuk Lymphoma. 2014;55:2018–23.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schizas, D., Theochari, N.A., Katsaros, I. et al. Pseudoachalasia: a systematic review of the literature. Esophagus 17, 216–222 (2020). https://doi.org/10.1007/s10388-020-00720-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-020-00720-1