Abstract
A 65-year-old man reported nausea and anorexia after falling down a flight of stairs. Computed tomography (CT) showed a ruptured descending thoracic aortic aneurysm, and emergency thoracic endovascular aortic repair (TEVAR) was performed. However, after resuming food intake, the patient developed a fever. CT scan showed severe pneumomediastinum and a mediastinal abscess, and the patient was diagnosed with esophageal perforation. Emergency esophagectomy was performed, with an esophageal fistula made at the cervix. Jejunostomy was then performed to enable enteral nutrition. Histological examination showed substantial necrosis at the middle intrathoracic esophagus, and the patient was diagnosed with esophageal necrosis leading to perforation. Five months after the esophagectomy, gastric conduit reconstruction through the retrosternal route was performed. The patient was able to resume food intake, and survived more than 1 year after this surgery. Here, we describe the successful management of this rare case of esophageal necrosis after TEVAR for ruptured traumatic aortic aneurysm.
Similar content being viewed by others
Case report
A 65-year-old man with a medical history of diabetes, hypertension, and cerebral infarction experienced nausea and anorexia after falling down a flight of stairs and was admitted to a nearby hospital 4 days after the accident. Upper gastrointestinal endoscopy showed compression of the middle intrathoracic esophagus (Fig. 1a) but no lesions in the stomach, and chest X-ray showed extension of the mediastinum (Fig. 1b). A computed tomography (CT) scan showed aneurysm of the thoracic aorta and a massive hematoma in the mediastinum (Fig. 2). The patient was diagnosed with a ruptured traumatic thoracic aortic aneurysm and was transferred to a local cardiovascular hospital.
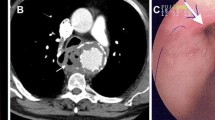
Emergency TEVAR was performed. Two ENDURANT iliac extensions (ETEW2424c80; Medtronic, Minneapolis, MN, USA) were inserted though the right common iliac artery. The patient was unsuited to receiving a TEVAR stent graft because his bilateral common iliac artery was extremely narrow due to arteriosclerosis. Successful extension was performed across the ruptured aortic aneurysm. On Day 3 after TEVAR, the patient resumed food intake, and on Day 8, he developed a fever but had no other symptoms. Chest X-ray showed severe pneumomediastinum (Fig. 1c), and a CT scan further revealed mediastinal abscess (Fig. 3). The patient was transferred to our hospital for emergency surgery.
On admission, he was in a stable condition with a body temperature of 39 °C, blood pressure of 131/68 mmHg, and a pulse rate of 95 beats/min. Blood examination showed high inflammation (white blood cell count, 20300/µl; C-reactive protein, 11.9 mg/dl) and poorly controlled blood sugar (blood sugar, 233 mg/dl; hemoglobin alpha 1, 9.4 %). Oral anticoagulant and antiplatelet agents were not being administered. The patient was diagnosed with esophageal perforation and mediastinitis. Esophagectomy and debridement was proposed, and he was immediately taken into surgery.
A right thoracotomy incision was made through the fourth intercostal space with the patient in the left lateral position. Dense inflammatory adhesions were dissected, and after cutting away the parietal pleura, a massive hematoma, and abscess capsule were revealed in the mediastinum. After breaking the capsule, we observed perforation of the middle intrathoracic esophagus. The stent graft was not exposed. Subtotal esophagectomy and debridement was performed, and a drain was inserted into the right thoracic cavity. With the patient in a supine position, an esophageal fistula was made at the left cervix. Jejunostomy was then performed at the left lateral abdomen to enable enteral nutrition with an 8-Fr catheter.
The resected specimen revealed that a substantial swathe of the middle intrathoracic esophagus had undergone necrosis and a portion of this necrotic area had become perforated (Fig. 4a). Hematoxylin eosin stain showed transmural necrosis with neutrophilic infiltration at the esophageal wall around the perforation (Fig. 4b). The patient was ultimately diagnosed with esophageal necrosis leading to esophageal perforation and mediastinitis.
a Examination of the resected specimen revealed that a substantial swathe of the middle intrathoracic esophagus had undergone necrosis, and a portion of this necrotic area had become perforated. b Hematoxylin eosin (HE) stain × 40 showed necrosis with neutrophilic infiltration at esophageal wall around perforation. The patient was ultimately diagnosed with esophageal necrosis leading to esophageal perforation and mediastinitis
The patient remained in the intensive care unit on a ventilator for 5 days following surgery, with glycemic control maintained with insulin injections. Enteral nutrition was started on Day 6 after surgery. Meropenem hydrate (1.5 g/day) and daptomycin (350 mg/day) were administered for 10 days and micafungin (75 mg/day) for 7 days following surgery, as bacteriologic examination of the mediastinal abscess revealed contamination with Candida albicans. The chest wound became infected on Day 7 following surgery, and debridement of the wound was performed. The wound gradually healed, and the patient was discharged from our hospital on Day 66 following surgery.
Five months after the esophagectomy, he was readmitted to our hospital for esophageal reconstruction. Gastric conduit reconstruction through the retrosternal route was performed. The patient was still alive and symptom-free more than 1 year after this second surgery, and no infection of the stent graft was observed.
Discussion
Esophageal necrosis after TEVAR is remarkably rare, with only three cases reported in the English literature. The pathophysiological mechanism of esophageal necrosis after TEVAR is unknown [1–3].
TEVAR has been found to be a relatively safe procedure in patients with descending thoracic aortic aneurysm, compared with surgical replacement of the graft [4]. Further, a systematic review supports the use of TEVAR as a first line therapy for blunt thoracic aortic trauma. These data support the use of TEVAR as a highly successful technique that may reduce mortality and paraplegia rates by half compared with open surgery [5]. In the present case, TEVAR was successfully performed for ruptured traumatic descending thoracic aortic aneurysm. However, the patient developed esophageal necrosis.
The most common complication experienced following TEVAR of the esophagus is aortoesophageal fistula [6]. Differential diagnosis between esophageal necrosis and aortoesophageal fistula appears difficult. In the present case, stent graft was not exposed and a fistula could not be verified. In addition, the pathology of extensive esophageal necrosis was significantly different from that seen in aortoesophageal fistula. Based on these observations, we diagnosed the case as esophageal necrosis rather than aortoesophageal fistula.
Potential mechanisms of esophageal necrosis after TEVAR include pressure necrosis of the esophagus due to aortic aneurysm and hematoma, ischemic necrosis due to stent graft coverage of the proper esophageal arteries, direct erosion of the rigid stent graft into the esophagus, and inflammation of the esophageal wall due to infection of the stent graft [1–3].
The cause of the esophageal necrosis in the present case was not clear. We suspect that, initially, the esophageal necrosis might have been primarily due to pressure from the hematoma of the aneurysm. However, given that the hematoma was growing well in the mediastinum with no severe pressure, the hematoma may have been growing inside the esophageal wall following the traumatic aortic aneurysm. We were unable to determine whether the hematoma was in the mediastinum or the esophageal wall on CT scan (Figs. 2, 3).
Alternatively, ischemia of the proper esophageal artery may have occurred due to the stent graft coverage. However, we suspect that the possibility of infection or direct erosion of the stent graft was low, as the stent graft was not exposed in the mediastinum.
The rarity of esophageal necrosis after TEVAR and lack of any symptoms particular to this condition might hamper or delay diagnosis. In the present case, for example, the patient had a fever but no other symptoms, while in a previously reported case, the patient had dysphagia, dysphonia, and nocturnal sweating [1]. Including our case, three patients have been diagnosed with esophageal necrosis within 2 weeks of TEVAR [2, 3]. Another patient was diagnosed 3 months after TEVAR [1]. However, in all cases, the actual time of onset of esophageal necrosis was unknown.
Given that the present and previous cases were all definitively diagnosed via CT scan, [1–3] CT scan should be performed promptly if esophageal necrosis is suspected after TEVAR. While we did not perform upper gastrointestinal endoscopy in the present case, this method may also be useful for diagnosing esophageal necrosis and assessing the extent of necrosis to determine surgical indications.
No consensus has yet been reached regarding optimum standard therapy for esophageal necrosis. In the present case, given that we noted no infection of the stent graft, the patient was treated with best practice by managing the esophageal perforation. We selected this course of treatment from among conservative antibiotics, primary repair, omental implantation repair, and esophageal resection after considering the etiology, location, and size of the perforation, time after perforation, inflammation, and patient’s general status, age, and medical history [7, 8].
In our patient, a substantial swathe of the middle intrathoracic esophagus had become necrotic, resulting in esophageal perforation and mediastinitis. We therefore decided to perform a two-stage operation. Esophagectomy and debridement were first performed to treat the esophageal perforation and mediastinitis, and once the patient’s physical condition had recovered sufficiently, gastric conduit reconstruction through the retrosternal route was performed. We elected to perform surgery in two stages to control inflammation from infection. This two-stage strategy also allowed for easy replacement of the aortic graft, if the stent graft had become infected.
Including our case, two patients with esophageal necrosis have undergone esophagectomy and remained alive 5–12 months after surgery [3]. In two other cases, the patients underwent drainage and died within 3–4 weeks [1, 2]. Esophagectomy is the most appropriate option for treating esophageal necrosis.
Given that the stent graft did not appear to be infected, we did not perform aortic replacement. However, if infection of the stent graft is suspected, antibiotic treatment and aortic replacement with cryopreserved homografts or a rifampicin-bonded Dacron graft should be performed immediately to remove potential sites of infection [9, 10].
In the present case, the cause of necrosis is unclear. However, it is important to recognize the possibility of the development of esophageal necrosis following TEVAR for ruptured aneurysm. If it is possible to diagnose the esophageal necrosis at an early stage and provide appropriate treatment, the possibility of saving the patient’s life will improve.
Conclusion
We successfully managed a rare case of esophageal necrosis after TEVAR for ruptured traumatic thoracic aortic aneurysm. It is essential to diagnose the esophageal necrosis at an early stage and provide appropriate treatment.
References
Porcu P, Chavanon O, Sessa C, et al. Esophageal fistula after endovascular treatment in a type B aortic dissection of the descending thoracic aorta. J Vasc Surg. 2005;41:708–11.
De Praetere H, Lerut P, Johan M, et al. Esophageal necrosis after endoprosthesis for ruptured thoracoabdominal aneurysm type I: can long-segment stent grafting of the thoracoabdominal aorta induce transmural necrosis? Ann Vasc Surg. 2010;24:1137.e7–12.
Tobisch A, Ittrich H, Izbicki JR, et al. Successful management of esophageal necrosis after endovascular repair of chronic type B aortic dissection. Ann Thorac Surg. 2014;98:2209–11.
Dake MD, Miller DC, Semba CP, et al. Transluminal placement of endovascular stent-grafts for the treatment of descending thoracic aortic aneurysms. N Engl J Med. 1994;331:1729–34.
Hoffer EK, Forauer AR, Silas AM, et al. Endovascular stent-graft or open surgical repair for blunt thoracic aortic trauma: systematic review. J Vasc Interv Radiol. 2008;19:1153–64.
Czerny M, Eggebrecht H, Sodeck G, et al. New insights regarding the incidence, presentation and treatment options of aorto-oesophageal fistulation after thoracic endovascular aortic repair: the European Registry of endovascular aortic repair complications. Eur J Cardiothorac Surg. 2014;45:452–7.
Okten I, Cangir AK, Ozdemir N, et al. Management of esophageal perforation. Surg Today. 2001;31:36–9.
Huber-Lang M, Henne-Bruns D, Schmitz B, et al. Esophageal perforation: principles of diagnosis and surgical management. Surg Today. 2006;36:332–40.
Kubota S, Shiiya N, Shingu Y, et al. Surgical strategy for aortoesophageal fistula in the endovascular era. Gen Thorac Cardiovasc Surg. 2013;61:560–4.
Saito A, Motomura N, Hattori O, et al. Outcome of surgical repair of aorto-eosophageal fistulas with cryopreserved aortic allografts. Interact CardioVasc Thorac Surg. 2012;14:532–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
This article contains no studies involving human or animal subjects.
Conflict of interest
All authors declare no financial or commercial conflicts of interest.
Rights and permissions
About this article
Cite this article
Miura, S., Kanaya, S., Kawada, H. et al. Successful management of esophageal necrosis after thoracic endovascular aortic repair for ruptured traumatic aortic aneurysm. Esophagus 13, 386–390 (2016). https://doi.org/10.1007/s10388-016-0544-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-016-0544-6