Summary
Background
Fistula in ano causes significant morbidity and affects patients’ quality of life (QOL). A validated five-point Crohn’s Disease Perianal Activity Index (CDAI) has been reported, but there is no validated QOL/disease activity measure for patients with cryptoglandular sepsis (CS).
Methods
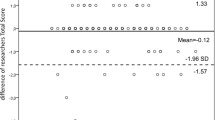
We recruited 20 CS patients with active perianal sepsis requiring surgical intervention, who completed questionnaires of quantitative scores including the CDAI, the Fecal Incontinence Quality of Life (FIQOL), St. Mark’s Incontinence Score, and the 36-Item Short Form Health Survey (SF-36). Qualitatively, patients listed the five most significant impacts of perianal sepsis on their QOL. Disease activity was rated by the treating surgeon. The study also recruited 20 age-matched controls with no perianal disease. After analyzing each CDAI element, and using the patient and surgeon feedback, a simplified Perianal Sepsis Index (PASI) score was created.
Results
Qualitatively, pain (100%), discharge/leakage (80%), sexual function (60%), and depression (45%) were the most commonly stated impacts by patients. There were significant differences between patients and controls in the CDAI (9.8 vs. 0) and St. Mark’s scores (7.7 vs. 0.5), as well as in three domains of the FIQOL and SF-36 (p > 0.0I). After analyzing each CDAI element, patients were inaccurate in coding the type of perianal disease and degree of induration compared with their treating surgeon’s assessment. Removing disease type and degree of induration created a simplified PASI score. There were significant differences between patients and controls regarding CDAI and PASI scores (p < 0.05) but not St. Mark’s, FIQOL or SF-36 scores.
Conclusion
The PASI score offers a method of self-quantifying the impact of perianal sepsis on QOL.




Similar content being viewed by others
References
Eisenhammer S. Long-tract anteroposterior intermuscular fistula. Dis Colon Rectum. 1964;7:438–40.
Parks AG. Royal Society of Medicine, Section of Proctology; Meeting 27 November 1974. President’s Address. Anorectal incontinence. Proc R Soc Med. 1975;68(11):681–90.
Rizzo JA, Naig AL, Johnson EK. Anorectal abscess and fistula-in-ano: evidence-based management. Surg Clin North Am. 2010;90(1):45–68. https://doi.org/10.1016/j.suc.2009.10.001.
Held D, Khubchandani I, Sheets J. Management of anorectal horseshoe abscess and fistula. Dis Colon Rectum. 1986;29(12):793–7.
Sainio P. Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol. 1984;73(4):219–24.
Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976;63(1):1–12.
Hämäläinen K, Sainio AP. Incidence of fistulas after drainage of acute anorectal abscesses. Dis Colon Rectum. 1998;41(11):1357–61. discussion 1361–2.
Ramanujam PS, Prasad ML, Abcarian H, Tan AB. Perianal abscesses and fistulas. A study of 1023 patients. Dis Colon Rectum. 1984;27(9):593–7.
Winslett MC, Allan A, Ambrose NS. Anorectal sepsis as a presentation of occult rectal and systemic disease. Dis Colon Rectum. 1988;31(8):597–600.
Lunniss PJ, Phillips RKS. Surgical assessment of acute anorectal sepsis is a better predictor of fistula than microbiological analysis. BJS. 1994;81(3):368–9.
Garcia-Aguilar J, Belmonte C, Wong DW, Goldberg SM, Madoff RD. Anal fistula surgery. Dis Colon Rectum. 1996;39(7):723–9.
Wong S, Solomon M, Crowe P, Ooi K. Cure, continence and quality of life after treatment for fistula-in-ano. ANZ J Surg. 2008;78(8):675–82.
Irvine EJ. Review article: patients’ fears and unmet needs in inflammatory bowel disease. Aliment Pharmacol Ther. 2004;20(Suppl 4):54–9.
Garcia-Aguilar J, Davey CS, Le CT. Patient satisfaction after surgical treatment for fistula-in-ano. Dis Colon Rectum. 2000;43(9):1206–12.
Damon H, Guye O, Seigneurin A. Prevalence of anal incontinence in adults and impact on quality-of-life. Gastroenterol Clin Biol. 2006;30(1):37–43.
Irvine EJ. Usual therapy improves perianal Crohn’s disease as measured by a new disease activity index. McMaster IBD Study Group. J Clin Gastroenterol. 1995;20(1):27–32.
Sailer M, Bussen D. Quality of life in patients with benign anorectal disorders. BJS. 1998;85:1716–9.
Pescatori M, Anastasio G, Bottini C, Mentasti A. New grading and scoring for anal incontinence. Dis Colon Rectum. 1992;35(5):482–7.
Hüppe D, Enck P, Krüskemper G, May B. Psychosocial aspects of fecal incontinence. Leber Magen Darm. 1992;22(4):138–42.
Rockwood TH, Church JM. Fecal incontinence quality of life scale. Dis Colon Rectum. 2000;43(1):9–16. discussion 16–7.
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44(1):77–80.
McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–63.
Feinstein AR. An additional basic science for clinical medicine: IV. The development of clinimetrics. Ann Intern Med. 1983;99(6):843–8.
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmülling C, Neugebauer E, et al. Gastrointestinal quality of life index: development, validation and application of a new instrument. Br J Surg. 1995;82(2):216–22.
Seneviratne SA, Samarasekera DN, Kotalawala W. Quality of life following surgery for recurrent fistula-in-ano. Tech Coloproctol. 2009;13(3):215–7.
Stremitzer S, Strobl S, Kure V, Bîrsan T, Puhalla H, Herbst F, et al. Treatment of perianal sepsis and long-term outcome of recurrence and continence. Colorectal Dis. 2011;13(6):703–7.
Pescatori M, Ayabaca S, Caputo D. Can anal manometry predict anal incontinence after fistulectomy in males? Colorectal Dis. 2004;6(2):97–102.
Griffin N, Acheson AG, Tung P, et al. Quality of life in patients with chronic anal fissure. Colorectal Dis. 2004;6:39–44.
Williams DR, Coller JA, Corman ML, Nugent WF, Veidenheimer MC. Anal complications in Crohn’s disease. Dis Colon Rectum. 1981;24(1):22–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Tabassum, A. Zahid, C.M. Byrne, and C.J. Young declare that they have no competing interests.
Additional information
Author contribution
All authors contributed to the conception, design, analysis and interpretation of data, as well as drafting and critically revising the manuscript.
Rights and permissions
About this article
Cite this article
Tabassum, A., Zahid, A., Byrne, C.M. et al. Development of Perianal Sepsis Index (PASI) for assessing quality of life in chronic perianal sepsis. Eur Surg 50, 270–277 (2018). https://doi.org/10.1007/s10353-018-0543-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-018-0543-z