Abstract
Purpose
To determine whether dysautonomia can stratify individuals with other prodromal markers of Parkinson’s disease (PD) for risk of phenoconversion and functional decline, which may help identify subpopulations appropriate for experimental studies.
Methods
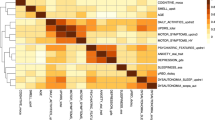
Data were obtained from Parkinson’s Progression Markers Initiative. Cohorts without PD but with at-risk features were included (hyposmia and/or rapid-eye-movement-sleep behavior disorder, LRRK2 gene mutation, GBA gene mutation). Dysautonomia measures included Scales-for-Outcomes-in-Parkinson’s-Disease Autonomic (SCOPA-AUT), seven SCOPA-AUT subscales, and cardiovascular dysfunction (supine hypertension, low pulse pressure, neurogenic orthostatic hypotension). Outcome measures were phenoconversion and Schwab-and-England Activities-of-Daily-Living (SE-ADL) ≤ 70, which indicates functional dependence. Cox proportional-hazards regression was used to evaluate survival to phenoconversion/SE-ADL ≤ 70 for each dysautonomia measure. If a significant association was identified, a likelihood-ratio test was employed to evaluate whether a significant interaction existed between the measure and cohort. If so, regression analysis was repeated stratified by cohort.
Results
Median follow-up was 30 months. On multivariable analysis, gastrointestinal and female sexual dysfunction subscales were associated with increased risk of phenoconversion, while the cardiovascular subscale and neurogenic orthostatic hypotension were associated with increased risk of SE-ADL ≤ 70; respective hazard ratios (95% confidence intervals) were 1.13 (1.01–1.27), 3.26 (1.39–7.61), 1.87 (1.16–2.99), 5.45 (1.40–21.25). Only the association between the cardiovascular subscale and SE-ADL ≤ 70 was modified by cohort.
Conclusions
Symptoms of gastrointestinal and female sexual dysfunction predict phenoconversion in individuals with other risk markers for PD, while signs and symptoms of cardiovascular dysfunction may be associated with functional decline.

Similar content being viewed by others
References
Devos D, Hirsch E, Wyse R (2021) Seven solutions for neuroprotection in Parkinson’s disease. Mov Disord 36(2):306–316
Berg D, Postuma RB, Adler CH, Bloem BR, Chan P, Dubois B, Gasser T, Goetz CG, Halliday G, Joseph L et al (2015) MDS research criteria for prodromal Parkinson’s disease. Mov Disord 30(12):1600–1611
Heinzel S, Berg D, Gasser T, Chen H, Yao C, Postuma RB (2019) Disease MDSTFotDoPs: update of the MDS research criteria for prodromal Parkinson’s disease. Mov Disord 34(10):1464–1470
Fereshtehnejad SM, Montplaisir JY, Pelletier A, Gagnon JF, Berg D, Postuma RB (2017) Validation of the MDS research criteria for prodromal Parkinson’s disease: Longitudinal assessment in a REM sleep behavior disorder (RBD) cohort. Mov Disord 32(6):865–873
Pilotto A, Heinzel S, Suenkel U, Lerche S, Brockmann K, Roeben B, Schaeffer E, Wurster I, Yilmaz R, Liepelt-Scarfone I et al (2017) Application of the Movement Disorder Society prodromal Parkinson’s disease research criteria in 2 independent prospective cohorts. Mov Disord 32(7):1025–1034
Mahlknecht P, Gasperi A, Djamshidian A, Kiechl S, Stockner H, Willeit P, Willeit J, Rungger G, Poewe W, Seppi K (2018) Performance of the movement disorders society criteria for prodromal Parkinson’s disease: a population-based 10-year study. Mov Disord 33(3):405–413
Mirelman A, Saunders-Pullman R, Alcalay RN, Shustak S, Thaler A, Gurevich T, Raymond D, Mejia-Santana H, Orbe Reilly M, Ozelius L et al (2018) Application of the Movement Disorder Society prodromal criteria in healthy G2019S-LRRK2 carriers. Mov Disord 33(6):966–973
Kulcsarova K, Ventosa JR, Feketeova E, Maretta M, Lesko N, Benca M, Han V, Gombosova L, Baloghova J, Slavkovska M et al (2021) Comparison in detection of prodromal Parkinson’s disease patients using original and updated MDS research criteria in two independent cohorts. Parkinsonism Relat Disord 87:48–55
Marini K, Seppi K, Tschiderer L, Kiechl S, Stockner H, Willeit P, Willeit J, Djamshidian A, Rungger G, Poewe W et al (2021) Application of the updated Movement Disorder Society criteria for prodromal Parkinson’s disease to a population-based 10-year study. Mov Disord 36(6):1464–1466
Postuma RB, Gagnon JF, Pelletier A, Montplaisir J (2013) Prodromal autonomic symptoms and signs in Parkinson’s disease and dementia with Lewy bodies. Mov Disord 28(5):597–604
Gao X, Chen H, Schwarzschild MA, Glasser DB, Logroscino G, Rimm EB, Ascherio A (2007) Erectile function and risk of Parkinson’s disease. Am J Epidemiol 166(12):1446–1450
Gao X, Chen H, Schwarzschild MA, Ascherio A (2011) A prospective study of bowel movement frequency and risk of Parkinson’s disease. Am J Epidemiol 174(5):546–551
Lin CH, Lin JW, Liu YC, Chang CH, Wu RM (2014) Risk of Parkinson’s disease following severe constipation: a nationwide population-based cohort study. Parkinsonism Relat Disord 20(12):1371–1375
Schrag A, Horsfall L, Walters K, Noyce A, Petersen I (2015) Prediagnostic presentations of Parkinson’s disease in primary care: a case-control study. Lancet Neurol 14(1):57–64
Kaufmann H, Norcliffe-Kaufmann L, Palma JA, Biaggioni I, Low PA, Singer W, Goldstein DS, Peltier AC, Shibao CA, Gibbons CH et al (2017) Natural history of pure autonomic failure: a United States prospective cohort. Ann Neurol 81(2):287–297
Singer W, Berini SE, Sandroni P, Fealey RD, Coon EA, Suarez MD, Benarroch EE, Low PA (2017) Pure autonomic failure: predictors of conversion to clinical CNS involvement. Neurology 88(12):1129–1136
Coon EA, Mandrekar JN, Berini SE, Benarroch EE, Sandroni P, Low PA, Singer W (2020) Predicting phenoconversion in pure autonomic failure. Neurology 95(7):e889–e897
Postuma RB, Iranzo A, Hu M, Hogl B, Boeve BF, Manni R, Oertel WH, Arnulf I, Ferini-Strambi L, Puligheddu M et al (2019) Risk and predictors of dementia and parkinsonism in idiopathic REM sleep behaviour disorder: a multicentre study. Brain 142(3):744–759
Parkinson Progression Marker I: The Parkinson Progression Marker Initiative (PPMI). Prog Neurobiol (2011), 95(4):629–635
Mollenhauer B, Caspell-Garcia CJ, Coffey CS, Taylor P, Singleton A, Shaw LM, Trojanowski JQ, Frasier M, Simuni T, Iranzo A et al (2019) Longitudinal analyses of cerebrospinal fluid alpha-synuclein in prodromal and early Parkinson’s disease. Mov Disord 34(9):1354–1364
Simuni T, Uribe L, Cho HR, Caspell-Garcia C, Coffey CS, Siderowf A, Trojanowski JQ, Shaw LM, Seibyl J, Singleton A et al (2020) Clinical and dopamine transporter imaging characteristics of non-manifest LRRK2 and GBA mutation carriers in the Parkinson’s progression markers initiative (PPMI): a cross-sectional study. Lancet Neurol 19(1):71–80
Darweesh SK, Verlinden VJ, Stricker BH, Hofman A, Koudstaal PJ, Ikram MA (2017) Trajectories of prediagnostic functioning in Parkinson’s disease. Brain 140(2):429–441
Chahine LM, Iranzo A, Fernandez-Arcos A, Simuni T, Seedorff N, Caspell-Garcia C, Amara AW, Comella C, Hogl B, Hamilton J et al (2019) Basic clinical features do not predict dopamine transporter binding in idiopathic REM behavior disorder. NPJ Parkinsons Dis 5:2
Visser M, Marinus J, Stiggelbout AM, Van Hilten JJ (2004) Assessment of autonomic dysfunction in Parkinson’s disease: the SCOPA-AUT. Mov Disord 19(11):1306–1312
Gibbons CH, Freeman R (2015) Clinical implications of delayed orthostatic hypotension: a 10-year follow-up study. Neurology 85(16):1362–1367
Umehara T, Matsuno H, Toyoda C, Oka H (2016) Clinical characteristics of supine hypertension in de novo Parkinson disease. Clin Auton Res 26(1):15–21
Park JH, Han SW, Baik JS (2017) A comparative study of central hemodynamics in Parkinson’s disease. J Mov Disord 10(3):135–139
McRae C, Diem G, Vo A, O’Brien C, Seeberger L (2000) Schwab & England: standardization of administration. Mov Disord 15(2):335–336
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Fox GN, Moawad N (2003) UpToDate: a comprehensive clinical database. J Fam Pract 52(9):706–710
Boston RC, Sumner AE (2003) STATA: a statistical analysis system for examining biomedical data. Adv Exp Med Biol 537:353–369
Glynn RJ, Chae CU, Guralnik JM, Taylor JO, Hennekens CH (2000) Pulse pressure and mortality in older people. Arch Intern Med 160(18):2765–2772
Hinkle JT, Perepezko K, Mills KA, Mari Z, Butala A, Dawson TM, Pantelyat A, Rosenthal LS, Pontone GM (2018) Dopamine transporter availability reflects gastrointestinal dysautonomia in early Parkinson disease. Parkinsonism Relat Disord 55:8–14
Kim R, Jun JS (2019) Association of autonomic symptoms with presynaptic striatal dopamine depletion in drug-naive Parkinson’s disease: an analysis of the PPMI data. Auton Neurosci 216:59–62
van Deursen DN, van den Heuvel OA, Booij J, Berendse HW, Vriend C (2020) Autonomic failure in Parkinson’s disease is associated with striatal dopamine deficiencies. J Neurol 267(7):1922–1930
Anang JB, Gagnon JF, Bertrand JA, Romenets SR, Latreille V, Panisset M, Montplaisir J, Postuma RB (2014) Predictors of dementia in Parkinson disease: a prospective cohort study. Neurology 83(14):1253–1260
Kim JS, Park HE, Park IS, Oh YS, Ryu DW, Song IU, Jung YA, Yoo IR, Choi HS, Lee PH et al (2017) Normal ‘heart’ in Parkinson’s disease: is this a distinct clinical phenotype? Eur J Neurol 24(2):349–356
Varanda S, da Ribeiro SJ, Costa AS, de Amorim CC, Alves JN, Rodrigues M, Carneiro G (2016) Sexual dysfunction in women with Parkinson’s disease. Mov Disord 31(11):1685–1693
Vela-Desojo L, Urso D, Kurtis-Urra M, Garcia-Ruiz PJ, Perez-Fernandez E, Lopez-Valdes E, Posada-Rodriguez I, Ybot-Gorrin I, Lopez-Manzanares L, Mata M et al (2020) Sexual dysfunction in early-onset Parkinson’s disease: a cross-sectional multicenter study. J Parkinsons Dis 10(4):1621–1629
Fereshtehnejad SM, Romenets SR, Anang JB, Latreille V, Gagnon JF, Postuma RB (2015) New clinical subtypes of Parkinson disease and their longitudinal progression: a prospective cohort comparison with other phenotypes. JAMA Neurol 72(8):863–873
Plouvier AO, Hameleers RJ, van den Heuvel EA, Bor HH, Olde Hartman TC, Bloem BR, van Weel C, Lagro-Janssen AL (2014) Prodromal symptoms and early detection of Parkinson’s disease in general practice: a nested case-control study. Fam Pract 31(4):373–378
Jennings D, Siderowf A, Stern M, Seibyl J, Eberly S, Oakes D, Marek K, Investigators P (2017) Conversion to Parkinson disease in the PARS hyposmic and dopamine transporter-deficit prodromal cohort. JAMA Neurol 74(8):933–940
Acknowledgements
Data used in the preparation of this article were obtained from the Parkinson’s Progression Markers Initiative (PPMI) database (www.ppmi-info.org/data). PPMI—a public–private partnership—is funded by the Michael J. Fox Foundation and funding partners 4D Pharma, AbbVie, AcureX Therapeutics, Allergan, Amathus Therapeutics, ASAP, Avid Radiopharmaceuticals, BIAL Biotech, Biogen, BioLegend, Bristol-Myers Squibb, Calico, Celgene, DaCapo Brain Science, Denali, The Edmond J. Safra Foundation, GE Healthcare, Genentech, GlaxoSmithKline, Golub Capital, Handl Therapeutics, Insitro, Janssen Neuroscience, Lilly, Lundbeck, Merck, Meso Scale Discovery, Neurocrine Biosciences, Pfizer, Piramal, Prevail, Roche, Sanofi Genzyme, Servier, Takeda, Teva, UCB, Verily, and Voyager Therapeutics. For up-to-date information on the study, visit www.ppmi-info.org.
Funding
This work was supported by the National Institutes of Health Pharmacoepidemiology T32 Grant GM075766, provided by the Perelman School of Medicine at the University of Pennsylvania.
Author information
Authors and Affiliations
Contributions
CMP developed the hypothesis, designed and performed the analysis, and prepared the manuscript. JYH provided guidance on statistical analysis and revisions for the manuscript. LMC, JFM, and AWW provided guidance on the analysis plan and revisions for the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Miller-Patterson has nothing to disclose. Dr. Hsu has received personal compensation in the range of $10,000–$49,999 for serving as Editor, Associate Editor, or Editorial Advisory Board Member for National Kidney Foundation and Public Library of Science. Dr. Chahine has received personal compensation in the range of $500–$4,999 for serving as a consultant for Gray Matters Technology. Dr. Chahine has received research support from University of Pittsburgh Medical Center, Michael J. Fox Foundation, and Biogen/Parkinson Study Group. Dr. Chahine has received publishing royalties from a publication relating to health care. Dr. Morley has nothing to disclose. Dr. Willis has received personal compensation in the range of $0–$499 for serving as an Editor, Associate Editor, or Editorial Advisory Board Member for Pharmacoepidemiology and Drug Safety. Dr. Willis has received research support from National Institutes of Health, National Institute on Aging, Biogen, Parkinson Foundation, and Arcadia.
Ethical approval
Each Parkinson’s Progression Markers Initiative site received approval from an ethics committee on human experimentation in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments before study initiation and obtained written informed consent from each study participant.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miller-Patterson, C., Hsu, J.Y., Chahine, L.M. et al. Selected autonomic signs and symptoms as risk markers for phenoconversion and functional dependence in prodromal Parkinson’s disease. Clin Auton Res 32, 463–476 (2022). https://doi.org/10.1007/s10286-022-00889-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-022-00889-8