Abstract
Breast cancer is one of the most prevailing forms of cancer globally. Immunotherapy has demonstrated efficacy in improving the overall survival of breast cancer. The aim of us was to formulate a novel signature predicated on immune checkpoint-related genes (ICGs) that could anticipate the prognosis and further analyze the immune status of patients with breast cancer. After acquiring data, we pinpointed the definitive ICGs for constructing the prognostic model of breast cancer. We constructed a novel prognostic model and created a fresh risk score called Immune Checkpoint-related Risk Score in breast cancer (ICRSBC). The nomogram was constructed to evaluate the accuracy of the model, and the new web-based tool was created to be more intuitive for predicting prognosis. We also investigated immunotherapy responsiveness and analyzed the tumor mutational burden (TMB) in ICRSBC subgroups. The ICRSBC was found to have significant correlations with the immune environment, immunotherapy responsiveness, and TMB. The expression levels of the 9 ICGs that construct the prognostic model and their promoter methylation levels are significantly different between breast cancer and normal tissues. Furthermore, the mutation profiles, the copy number alterations, and the levels of protein expression also exhibit marked disparities among the 9 ICGs. We have identified and validated a novel signature related to ICGs that is strongly associated with breast cancer progression. This signature enables us to create a risk score for prognosticating the survival and assessing the immune status of individuals affected by breast cancer.









Similar content being viewed by others
Data availability
The raw data utilized in this study are obtainable through the Gene Expression Omnibus (GEO) under accession number GSE42568 (https://www.ncbi.nlm.nih.gov/geo/). Additional data and materials are available from the University of California, Santa Cruz (UCSC), Xena browser (https://xenabrowser.net/). Access to the data is subject to any restrictions required by the relevant ethics committees, and requests will be assessed on an individual basis. Code used for analysis is available upon request from the corresponding author.
Abbreviations
- ICGs:
-
Immune checkpoint-related genes
- TCGA:
-
The Cancer Genome Atlas
- GEO:
-
Gene Expression Omnibus
- ICRSBC:
-
Immune checkpoint-related risk score in breast cancer
- IPS:
-
Immune phenotype score
- TMB:
-
Tumor mutational burden
- TME:
-
Tumor microenvironment
- IARC:
-
International Agency for Research on Cancer
- DCA:
-
Decision curve analysis
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- PD-1:
-
Programmed death 1
- PD-L1:
-
Programmed death-ligand 1
- CTLA-4:
-
Cytotoxic T lymphocyte-associated antigen 4
- LASSO:
-
Least absolute shrinkage selection operator
- KM:
-
Kaplan–Meier
- RECIST:
-
Response evaluation criteria in solid tumors
- irRC:
-
Immune-related response criteria
- irRECIST:
-
Immune-related response evaluation criteria in solid tumors
- iRECIST:
-
Immune response evaluation criteria in solid tumors
- WGCNA:
-
Weighted gene co-expression network analysis
- GO:
-
Gene ontology
- KEGG:
-
Kyoto encyclopedia of genes and genomes
- DO:
-
Disease ontology
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- RMS:
-
Root mean square
- GSVA:
-
Gene set variation analysis
- GSEA:
-
Gene set enrichment analysis
- SNP:
-
Single-nucleotide polymorphism
- SNV:
-
Single-nucleotide variant
- AMPK:
-
Adenosine 5′-monophosphate (AMP)-activated protein kinase
- FOX:
-
Forkhead box
- CPTAC:
-
Clinical proteomic tumor analysis consortium
- AAT:
-
Alpha 1-antitrypsin
- ACT:
-
Alpha 1-antichymotrypsin
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
McDonald ES, Clark AS, Tchou J, Zhang P, Freedman GM. Clinical diagnosis and management of breast cancer. J Nucl Med. 2016;57 Suppl 1(1535–5667 (Electronic)):9S-16S.
Condorelli R, Vaz-Luis I. Managing side effects in adjuvant endocrine therapy for breast cancer. Expert Rev Anticancer Ther. 2018;18(11):1101–12.
Tan S, Li D, Zhu X. Cancer immunotherapy: pros, cons and beyond. Biomed Pharmacother. 2020;124(1950–6007 (Electronic)):109821.
O’Donnell JS, Teng MWL, Smyth MJ. Cancer immunoediting and resistance to T cell-based immunotherapy. Nat Rev Clin Oncol. 2019;16(3):151–67.
Lei X, Lei Y, Li JK, et al. Immune cells within the tumor microenvironment: biological functions and roles in cancer immunotherapy. Cancer Lett. 2020;470(1872-7980 (Electronic)):126–33.
Bates JP, Derakhshandeh R, Jones L, Webb TJ. Mechanisms of immune evasion in breast cancer. BMC Cancer. 2018;18(1):556.
Barzaman K, Moradi-Kalbolandi S, Hosseinzadeh A, et al. Breast cancer immunotherapy: current and novel approaches. Int Immunopharmacol. 2021;98(1878–1705 (Electronic)):107886.
Binnewies M, Roberts EW, Kersten K, et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med. 2018;24(5):541–50.
Alsaab HO, Sau S, Alzhrani R, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8(1663–9812 (Print)):561.
Frelaut M, du Rusquec P, de Moura A, Le Tourneau C, Borcoman E. Pseudoprogression and hyperprogression as new forms of response to immunotherapy. BioDrugs. 2020;34(4):463–76.
Seymour L, Bogaerts J, Perrone A, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017;18(3):e143–52.
Li L, Li L, Liu M, Li Y, Sun Q. Novel immune-related prognostic model and nomogram for breast cancer based on ssGSEA. Front Genet. 2022;13(1664–8021 (Print)):957675.
Lv LH, Lu JR, Zhao T, Liu JL, Liang HQ. A CD8(+) T Cell-related genes expression signature predicts prognosis and the efficacy of immunotherapy in breast cancer. J Mammary Gland Biol Neoplasia. 2022;27(1):53–65.
Yao Y, Kong X, Liu R, Xu F, Liu G, Sun C. Development of a novel immune-related gene prognostic index for breast cancer. Front Immunol. 2022;13(1664–3224 (Electronic)):845093.
Chandrashekar DS, Karthikeyan SK, Korla PK, et al. UALCAN: an update to the integrated cancer data analysis platform. Neoplasia. 2022;25(1476–5586 (Electronic)):18–27.
Ferris RL. Immunology and immunotherapy of head and neck cancer. J Clin Oncol. 2015;33(29):3293–304.
Pfail JL, Katims AB, Alerasool P, Sfakianos JP. Immunotherapy in non-muscle-invasive bladder cancer: current status and future directions. World J Urol. 2021;39(5):1319–29.
Cha JH, Chan LC, Song MS, Hung MC. New approaches on cancer immunotherapy. Cold Spring Harb Perspect Med. 2020;10(8):a036863.
Coutzac C, Pernot S, Chaput N, Zaanan A. Immunotherapy in advanced gastric cancer, is it the future? Crit Rev Oncol/Hematol. 2019;133(1879-0461 (Electronic)):25–32.
Keenan TE, Tolaney SM. Role of immunotherapy in triple-negative breast cancer. J Natl Compr Canc Netw. 2020;18(4):479–89.
Li Y, Zhang H, Merkher Y, et al. Recent advances in therapeutic strategies for triple-negative breast cancer. J Hematol Oncol. 2022;15(1):121.
Bernard V, Young J, Binart N. Prolactin: a pleiotropic factor in health and disease. Nat Rev Endocrinol. 2019;15(6):356–65.
Karayazi Atici O, Govindrajan N, Lopetegui-Gonzalez I, Shemanko CS. Prolactin: a hormone with diverse functions from mammary gland development to cancer metastasis. Semin Cell Dev Biol. 2021;114(1096–3634 (Electronic)):159–70.
Tabibzadeh S. Signaling pathways and effectors of aging. Front Biosci (Landmark Ed). 2021;26(1):50–96.
Soria-Bretones I, Saez C, Ruiz-Borrego M, Japon MA, Huertas P. Prognostic value of CtIP/RBBP8 expression in breast cancer. Cancer Med. 2013;2(6):774–83.
Ashour N, Angulo JC, Gonzalez-Corpas A, et al. Epigenetic regulation of gfi1 in endocrine-related cancers: a role regulating tumor growth. Int J Mol Sci. 2020;21(13):4687.
Downs-Canner SM, Meier J, Vincent BG, Serody JS. B cell function in the tumor microenvironment. Annu Rev Immunol. 2022;40(1545–3278 (Electronic)):169–93.
Pan Y, Yu Y, Wang X, Zhang T. Tumor-associated macrophages in tumor immunity. Front Immunol. 2020;11(1664–3224 (Electronic)):583084.
Lee YS, Radford KJ. The role of dendritic cells in cancer. Int Rev Cell Mol Biol. 2019;348(1937–6448 (Print)):123–78.
Silwal-Pandit L, Langerod A, Borresen-Dale AL. TP53 mutations in breast and ovarian cancer. Cold Spring Harb Perspect Med. 2017;7(1):a026252.
Schon K, Tischkowitz M. Clinical implications of germline mutations in breast cancer: TP53. Breast Cancer Res Treat. 2018;167(2):417–23.
Pollock NC, Ramroop JR, Hampel H, et al. Differences in somatic TP53 mutation type in breast tumors by race and receptor status. Breast Cancer Res Treat. 2022;192(3):639–48.
Liu CL, Cheng SP, Huang WC, et al. Aberrant expression of solute carrier family 35 member A2 correlates with tumor progression in breast cancer. In Vivo. 2023;37(1):262–9.
Kabakov AE, Gabai VL. HSP70s in breast cancer: promoters of tumorigenesis and potential targets/tools for therapy. Cells. 2021;10(12):3446.
Na Y, Kaul SC, Ryu J, et al. Stress chaperone mortalin contributes to epithelial-mesenchymal transition and cancer metastasis. Cancer Res. 2016;76(9):2754–65.
Stephens PJ, Tarpey PS, Davies H, et al. The landscape of cancer genes and mutational processes in breast cancer. Nature. 2012;486(7403):400–4.
Jeong YJ, Oh HK, Choi HR, Park SH. Methylation of the NT5E gene is associated with poor prognostic factors in breast cancer. Diagnostics (Basel). 2020;10(11):939.
Godbole M, Togar T, Patel K, et al. Up-regulation of the kinase gene SGK1 by progesterone activates the AP-1-NDRG1 axis in both PR-positive and -negative breast cancer cells. J Biol Chem. 2018;293(50):19263–76.
Acknowledgements
We extend our heartfelt appreciation to home-for-researchers (https://www.home-for-researchers.com) for providing a valuable resource for data analysis.
Funding
This study received funding from the National Natural Science Foundation of China (Grant Number 82003802), the Science and Technology Program of Hunan Health Commission (Grant Number 20201978), the China Scholarship Council (Grant Number 201808430085) and Clinical Research 4310 Program of the First Affiliated Hospital of the University of South China (Grant Number 20224310NHYCG04), Science and technology innovation Program of Hengyang City (Grant Number 202250045223), and the Natural Science Foundation of Hunan Province (Grant Numbers 2019JJ50542 and 2023JJ50156).
Author information
Authors and Affiliations
Contributions
TLZ and HHH conceived and designed the study. TY and HHH drafted the manuscript and conducted data analysis. TLZ, LXJ, and DE strictly revised the manuscript. HXZ, WDZ, JDZ, and SYW contributed to write figure legends. The final manuscript was reviewed and approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have disclosed that they have no conflicts of interest.
Ethics approval and consent to participate
There are no ethical considerations applicable to our article.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10238_2023_1247_MOESM1_ESM.tif
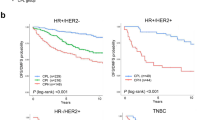
Relationship between ICRSBC and tumor progression. (A) Heatmap showing the relationship between ICRSBC and multiple clinical variables (*P < 0.05; **P < 0.01; ***P < 0.001). Correlation between ICRSBC and N stage (B), T stage (C), Age (D), stage (E), PAM50 subtypes (F). (TIF 28184 KB)
10238_2023_1247_MOESM2_ESM.jpg
Comparison between ICRSBC and other prognostic signatures for breast cancer. Survival analysis of distinct risk groups in breast cancer using ICRSBC (A), Li-signature (B), Lv-signature (C), and Yao-signature (D). The ROC curves for 1-, 3-, and 5-year survival prediction using ICRSBC (E), Li-signature (F), Lv-signature (G), and Yao-signature (H) in breast cancer. The ROC curves for 5-year survival prediction employing ICRSBC, Nomogram, and 3 other signatures in breast cancer (I). The C-index (J), RMS (K), and DCA (L) for the evaluation of 4 prognostic signatures in breast cancer. (JPG 3496 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, H., Yan, T., Zhu, H. et al. A novel immune checkpoint-related signature for prognosis and immune analysis in breast cancer. Clin Exp Med 23, 5139–5159 (2023). https://doi.org/10.1007/s10238-023-01247-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01247-2