Abstract
Purpose
The purpose of this study was to investigate the predictive value of advanced lung cancer inflammation index (ALI) for short-term outcomes and prognosis of colorectal cancer (CRC) patients who underwent radical surgery.
Methods
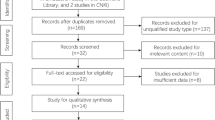
CRC patients who underwent radical resection were included from Jan 2011 to Jan 2020 in our single clinical centre. Short-term outcomes, overall survival (OS), and disease-free survival (DFS) were compared in different groups. Cox analysis was conducted to identify independent risk factors for OS and DFS.
Results
A total of 4010 patients who underwent radical CRC surgery were enrolled in the current study. As a result, the low ALI group had longer operation time (p = 0.02), more intra-operative blood loss (p < 0.01), longer postoperative hospital stay (p < 0.01), and more overall complications (p < 0.01). Moreover, ALI (p < 0.01, OR = 0.679, 95% CI = 0.578–0.798) was an independent risk factor for overall complications. As for survival, the low ALI group had worse OS in all TNM stages (p < 0.01), stage II (p < 0.01) and stage III (p < 0.01). Similarly, the low ALI group had worse DFS in all TNM stages (p < 0.01), stage II (p < 0.01), and stage III (p < 0.01). In Cox analysis, ALI was an independent risk factors for OS (p < 0.01, HR = 0.707, 95% CI = 0.589–0.849) and DFS (p < 0.01, HR = 0.732, 95% CI = 0.622–0.861).
Conclusion
Lower ALI was associated with more postoperative complications, worse OS, and DFS for CRC patients who underwent radical surgery. Furthermore, ALI was an independent risk factor for overall complications, OS, and DFS. Surgeons should pay close attention to patients with low ALI before surgery and make clinical strategies cautiously.



Similar content being viewed by others
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCA estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Hossain MS, Karuniawati H, Jairoun AA et al (2022) Colorectal cancer: a review of carcinogenesis, global epidemiology, current challenges, risk factors, preventive and treatment strategies. Cancers (Basel) 14(7):1732. https://doi.org/10.3390/cancers14071732
Liu XY, Kang B, Cheng YX et al (2022) Higher body mass index was associated with better prognosis in diabetic patients with stage II colorectal cancer. BMC Cancer 22(1):596. https://doi.org/10.1186/s12885-022-09691-1
Cheng YX, Liu XY, Kang B et al (2022) Comparison of surgical and oncologic outcomes in very elderly patients (≥ 80 years old) and elderly (65–79 years old) colorectal cancer patients: a propensity score matching. BMC Gastroenterol 22(1):205. https://doi.org/10.1186/s12876-022-02277-y
Tanis PJ, Buskens CJ, Bemelman WA (2014) Laparoscopy for colorectal cancer. Best Pract Res Clin Gastroenterol 28(1):29–39. https://doi.org/10.1016/j.bpg.2013.11.017
Liu XY, Yuan C, Kang B et al (2022) Predictors associated with planned and unplanned admission to intensive care units after colorectal cancer surgery: a retrospective study. Support Care Cancer 30(6):5099–5105. https://doi.org/10.1007/s00520-022-06939-1
Liu XY, Li ZW, Kang B et al (2022) Does preoperative waiting time affect the short-term outcomes and prognosis of colorectal cancer patients? A retrospective study from the west of China. Can J Gastroenterol Hepatol 30(2022):8235736. https://doi.org/10.1155/2022/8235736
Doleman B, Mills KT, Lim S et al (2016) Body mass index and colorectal cancer prognosis: a systematic review and meta-analysis. Tech Coloproctol 20(8):517–535. https://doi.org/10.1007/s10151-016-1498-3
Adachi T, Hinoi T, Kinugawa Y et al (2016) Lower body mass index predicts worse cancer-specific prognosis in octogenarians with colorectal cancer. J Gastroenterol 51(8):779–787. https://doi.org/10.1007/s00535-015-1147-z
Lai CC (2011) Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Colorectal Dis 26:473–481. https://doi.org/10.1007/s00384-010-1113-4
Chandrasinghe PC, Ediriweera DS, Sumudu K et al (2013) Pre-operative hypoalbuminaemia predicts poor overall survival in rectal cancer: a retrospective cohort analysis. BMC Clin Pathol 13:12. https://doi.org/10.1186/1472-6890-13-12
Kubo H, Murayama Y, Arita T et al (2016) The prognostic value of preoperative neutrophil-to-lymphocyte ratio in colorectal cancer. World J Surg 40(11):2796–2802. https://doi.org/10.1007/s00268-016-3595-x
Cui M, Xu R, Yan B (2020) A persistent high neutrophil-to-lymphocyte ratio predicts poor prognosis in patients with colorectal cancer undergoing resection. Mol Clin Oncol 13(5):63. https://doi.org/10.3892/mco.2020.2133
Jafri SH, Shi R, Mills G (2013) Advance lung cancer inflammation index (ALI) at diagnosis is a prognostic marker in patients with metastatic non-small cell lung cancer (NSCLC): a retrospective review. BMC Cancer 27(13):158. https://doi.org/10.1186/1471-2407-13-158
Mandaliya H, Jones M, Oldmeadow C et al (2019) Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Transl Lung Cancer Res 8(6):886–894. https://doi.org/10.21037/tlcr.2019.11.16
Hu Z, Wu W, Zhang X et al (2021) Advanced lung cancer inflammation index is a prognostic factor of patients with small-cell lung cancer following surgical resection. Cancer Manag Res 26(13):2047–2055. https://doi.org/10.2147/CMAR.S295952
Zhang X, Wang D, Sun T et al (2022) Advanced lung cancer inflammation index (ALI) predicts prognosis of patients with gastric cancer after surgical resection. BMC Cancer 22(1):684. https://doi.org/10.1186/s12885-022-09774-z
Yin C, Toiyama Y, Okugawa Y et al (2021) Clinical significance of advanced lung cancer inflammation index, a nutritional and inflammation index, in gastric cancer patients after surgical resection: A propensity score matching analysis. Clin Nutr 40(3):1130–1136. https://doi.org/10.1016/j.clnu.2020.07.018
Tan X, Peng H, Gu P et al (2021) Prognostic significance of the L3 skeletal muscle index and advanced lung cancer inflammation index in elderly patients with esophageal cancer. Cancer Manag Res 9(13):3133–3143. https://doi.org/10.2147/CMAR.S304996
Feng JF, Huang Y, Chen QX (2014) A new inflammation index is useful for patients with esophageal squamous cell carcinoma. Onco Targets Ther 30(7):1811–1815. https://doi.org/10.2147/OTT.S68084
Barth DA, Brenner C, Riedl JM et al (2020) External validation of the prognostic relevance of the advanced lung cancer inflammation index (ALI) in pancreatic cancer patients. Cancer Med 9(15):5473–5479. https://doi.org/10.1002/cam4.3233
Topkan E, Mertsoylu H, Ozdemir Y et al (2019) Prognostic usefulness of advanced lung cancer inflammation index in locally-advanced pancreatic carcinoma patients treated with radical chemoradiotherapy. Cancer Manag Res 7(11):8807–8815. https://doi.org/10.2147/CMAR.S222297
Horino T, Tokunaga R, Miyamoto Y et al (2021) The advanced lung cancer inflammation index is a novel independent prognosticator in colorectal cancer patients after curative resection. Ann Gastroenterol Surg 6(1):83–91. https://doi.org/10.1002/ags3.12499
Kusunoki K, Toiyama Y, Okugawa Y et al (2020) Advanced lung cancer inflammation index predicts outcomes of patients with colorectal cancer after surgical resection. Dis Colon Rectum 63(9):1242–1250. https://doi.org/10.1097/DCR.0000000000001658
Xie H, Huang S, Yuan G et al (2020) The advanced lung cancer inflammation index predicts short and long-term outcomes in patients with colorectal cancer following surgical resection: a retrospective study. PeerJ 8:e10100. https://doi.org/10.7717/peerj.10100
Pian G, Hong SY, Oh SY (2022) Prognostic value of advanced lung cancer inflammation index in patients with colorectal cancer liver metastases undergoing surgery. Tumori 108(1):56–62. https://doi.org/10.1177/0300891620983465
Shibutani M, Maeda K, Nagahara H et al (2019) The prognostic significance of the advanced lung cancer inflammation index in patients with unresectable metastatic colorectal cancer: a retrospective study. BMC Cancer 19(1):241. https://doi.org/10.1186/s12885-019-5468-9
Weiser MR (2018) AJCC 8th edition: colorectal cancer. Ann Surg Oncol 25(6):1454–1455. https://doi.org/10.1245/s10434-018-6462-1
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Almasaudi AS, Dolan RD, Edwards CA et al (2020) Hypoalbuminemia reflects nutritional risk, body composition and systemic inflammation and is independently associated with survival in patients with colorectal cancer. Cancers (Basel) 12(7):1986. https://doi.org/10.3390/cancers12071986
Garth AK, Newsome CM, Simmance N et al (2010) Nutritional status, nutrition practices and post-operative complications in patients with gastrointestinal cancer. J Hum Nutr Diet 23(4):393–401. https://doi.org/10.1111/j.1365-277X.2010.01058.x
Hu WH, Eisenstein S, Parry L et al (2019) Preoperative malnutrition with mild hypoalbuminemia associated with postoperative mortality and morbidity of colorectal cancer: a propensity score matching study. Nutr J 18(1):33. https://doi.org/10.1186/s12937-019-0458-y
Hu WH, Cajas-Monson LC, Eisenstein S et al (2015) Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 7(14):91. https://doi.org/10.1186/s12937-015-0081-5
Kwag SJ, Kim JG, Kang WK et al (2014) The nutritional risk is an independent factor for postoperative morbidity in surgery for colorectal cancer. Ann Surg Treat Res 86(4):206–211. https://doi.org/10.4174/astr.2014.86.4.206
Cavagnari MAV, Silva TD, Pereira MAH et al (2019) Impact of genetic mutations and nutritional status on the survival of patients with colorectal cancer. BMC Cancer 19(1):644. https://doi.org/10.1186/s12885-019-5837-4.PMID:31255173
Barao K, Abe VCM, Silva FP et al (2017) Association between nutrition status and survival in elderly patients with colorectal cancer. Nutr Clin Pract 32(5):658–663. https://doi.org/10.1177/0884533617706894
Karabulut S, Dogan I, Usul Afsar C et al (2021) Does nutritional status affect treatment tolarability, response and survival in metastatic colorectal cancer patients? Results of a prospective multicenter study. J Oncol Pharm Pract 27(6):1357–1363. https://doi.org/10.1177/1078155220959427
Nakamura Y, Imada A, Fukugaki A et al (2022) Association of nutritional risk and systemic inflammation with survival in patients with colorectal cancer who underwent curative surgery. Clin Nutr ESPEN 49:417–424. https://doi.org/10.1016/j.clnesp.2022.03.011
Chen JH, Zhai ET, Yuan YJ et al (2017) Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol 23(34):6261–6272. https://doi.org/10.3748/wjg.v23.i34.6261
Song Y, Yang Y, Gao P et al (2017) The preoperative neutrophil to lymphocyte ratio is a superior indicator of prognosis compared with other inflammatory biomarkers in resectable colorectal cancer. BMC Cancer 17(1):744. https://doi.org/10.1186/s12885-017-3752-0
Acknowledgements
We acknowledge all the authors whose publications are referred in our article.
Funding
This study is supported by CQMU Program for Youth Innovation in Future Medicine (W0190).
Author information
Authors and Affiliations
Contributions
All authors contributed to data collection, data analysis, write the original draft. All authors have agreed on the journal to which the manuscript will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval and informed consent
The study was approved by the ethics committee of our institution (The First Affiliated Hospital of Chongqing Medical University, 2022-135-2), and all patients signed informed consent. This study was conducted in accordance with the World Medical Association Declaration of Helsinki as well.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Zhang, B., Li, ZW., Tong, Y. et al. The predictive value of advanced lung cancer inflammation index for short-term outcomes and prognosis of colorectal cancer patients who underwent radical surgery. Int J Clin Oncol 28, 1616–1624 (2023). https://doi.org/10.1007/s10147-023-02410-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-023-02410-1