Abstract
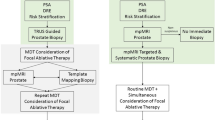
Multiparametric magnetic resonance imaging (mpMRI) has been increasingly used to diagnose clinically significant prostate cancer (csPC) because of its usefulness in combination with anatomic and functional data. MRI-targeted biopsy, such as MRI-transrectal ultrasound (TRUS) fusion image-guided prostate biopsy, has high accuracy in the detection and localization of csPC. This novel diagnostic technique contributes to the development of tailor-made medicine as focal therapy, which cures the csPC while preserving the anatomical structures related to urinary and sexual function. In the early days of focal therapy, TRUS-guided systematic biopsy was used for patient selection, and treatment was performed for patients with low-risk PC. With the introduction of mpMRI and mapping biopsy, the treatment range is now determined based on individualized cancer localization. In recent prospective studies, 87.4% of treated patients had intermediate- and high-risk PC. However, focal therapy has two main limitations. First, a randomized controlled trial would be difficult to design because of the differences in pathological features between patients undergoing focal therapy and radical treatment. Therefore, pair-matched studies and/or historical controlled studies have been performed to compare focal therapy and radical treatment. Second, no long-term (≥ 10-year) follow-up study has been performed. However, recent prospective studies have encouraged the use of focal therapy as a treatment strategy for localized PC because it contributes to high preservation of continence and erectile function.



Similar content being viewed by others
References
Barret E, Turkbey B, Puech P et al (2019) Update on the ICUD-SIU consultation on multi-parametric magnetic resonance imaging in localised prostate cancer. World J Urol 37:429–436
Onik G, Miessau M, Bostwick DG (2009) Three-dimensional prostate mapping biopsy has a potentially significant impact on prostate cancer management. J Clin Oncol 27:4321–4326
Shoji S, Hiraiwa S, Ogawa T et al (2017) Accuracy of real-time magnetic resonance imaging-transrectal ultrasound fusion image-guided transperineal target biopsy with needle tracking with a mechanical position-encoded stepper in detecting significant prostate cancer in biopsy-naive men. Int J Urol 24:288–294
Shoji S (2019) Magnetic resonance imaging-transrectal ultrasound fusion image-guided prostate biopsy: current status of the cancer detection and the prospects of tailor-made medicine of the prostate cancer. Investig Clin Urol 60:4–13
Shoji S, Ukimura O, de Castro Abreu AL et al (2016) Image-based monitoring of targeted biopsy-proven prostate cancer on active surveillance: 11-year experience. World J Urol 34:221–227
Stavrinides V, Giganti F, Emberton M et al (2019) MRI in active surveillance: a critical review. Prostate Cancer Prostatic Dis 22:5–15
Hung AJ, Abreu AL, Shoji S et al (2012) Robotic transrectal ultrasonography during robot-assisted radical prostatectomy. Eur Urol 62:341–348
van der Poel HG, van den Bergh RCN, Briers E et al (2018) Focal therapy in primary localised prostate cancer: the European Association of Urology Position in 2018. Eur Urol 74:84–91
Vilanova JC, Barcelo-Vidal C, Comet J et al (2011) Usefulness of prebiopsy multifunctional and morphologic MRI combined with free-to-total prostate-specific antigen ratio in the detection of prostate cancer. AJR Am J Roentgenol 196:W715–W722
Delongchamps NB, Rouanne M, Flam T et al (2011) Multiparametric magnetic resonance imaging for the detection and localization of prostate cancer: combination of T2-weighted, dynamic contrast-enhanced and diffusion-weighted imaging. BJU Int 107:1411–1418
Weinreb JC, Barentsz JO, Choyke PL et al (2016) PI-RADS prostate Imaging—reporting and data system: 2015, Version 2. Eur Urol 69:16–40
Barentsz JO, Richenberg J, Clements R et al (2012) ESUR prostate MR guidelines 2012. Eur Radiol 22:746–757
Collins DJ, Padhani AR (2004) Dynamic magnetic resonance imaging of tumor perfusion. Approaches and biomedical challenges. IEEE Eng Med Biol Mag 23:65–83
Gibbs P, Liney GP, Pickles MD et al (2009) Correlation of ADC and T2 measurements with cell density in prostate cancer at 3.0 Tesla. Invest Radiol 44:572–576
van As NJ, de Souza NM, Riches SF et al (2009) A study of diffusion-weighted magnetic resonance imaging in men with untreated localised prostate cancer on active surveillance. Eur Urol 56:981–987
Zelhof B, Pickles M, Liney G et al (2009) Correlation of diffusion-weighted magnetic resonance data with cellularity in prostate cancer. BJU Int 103:883–888
Turkbey B, Shah VP, Pang Y et al (2011) Is apparent diffusion coefficient associated with clinical risk scores for prostate cancers that are visible on 3-T MR images? Radiology 258:488–495
Rud E, Klotz D, Rennesund K et al (2014) Detection of the index tumour and tumour volume in prostate cancer using T2-weighted and diffusion-weighted magnetic resonance imaging (MRI) alone. BJU Int 114:E32–E42
Baco E, Ukimura O, Rud E et al (2015) Magnetic resonance imaging-transrectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol 67:787–794
Johnson DC, Raman SS, Mirak SA et al (2019) Detection of individual prostate cancer foci via multiparametric magnetic resonance imaging. Eur Urol 75:712–720
Rosenkrantz AB, Mendrinos S, Babb JS et al (2012) Prostate cancer foci detected on multiparametric magnetic resonance imaging are histologically distinct from those not detected. J Urol 187:2032–2038
Hamoen EH, de Rooij M, Witjes JA et al (2015) Use of the Prostate Imaging Reporting and Data System (PI-RADS) for prostate cancer detection with multiparametric magnetic resonance imaging: a diagnostic meta-analysis. Eur Urol 67:1112–1121
Steiger P, Thoeny HC (2016) Prostate MRI based on PI-RADS version 2: how we review and report. Cancer Imaging 16:9
Transin S, Souchon R, Gonindard-Melodelima C et al (2019) Computer-aided diagnosis system for characterizing ISUP grade≥2 prostate cancers at multiparametric MRI: a cross-vendor evaluation. Diagn Interv Imaging 100:801–811
Wegelin O, van Melick HHE, Hooft L et al (2017) Comparing three different techniques for magnetic resonance imaging-targeted prostate biopsies: a systematic review of in-bore versus magnetic resonance imaging-transrectal ultrasound fusion versus cognitive registration. Is there a preferred technique? Eur Urol 71:517–531
Schoots IG, Roobol MJ, Nieboer D et al (2015) Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol 68:438–450
Humphrey PA (1993) Complete histologic serial sectioning of a prostate gland with adenocarcinoma. Am J Surg Pathol 17:468–472
Mouraviev V, Villers A, Bostwick DG et al (2011) Understanding the pathological features of focality, grade and tumour volume of early-stage prostate cancer as a foundation for parenchyma-sparing prostate cancer therapies: active surveillance and focal targeted therapy. BJU Int 108:1074–1085
Nassiri N, Chang E, Lieu P et al (2018) Focal therapy eligibility determined by magnetic resonance imaging/ultrasound fusion biopsy. J Urol 199:453–458
Scheltema MJ, Tay KJ, Postema AW et al (2017) Utilization of multiparametric prostate magnetic resonance imaging in clinical practice and focal therapy: report from a Delphi consensus project. World J Urol 35:695–701
Onik G, Narayan P, Vaughan D et al (2002) Focal “nerve-sparing” cryosurgery for treatment of primary prostate cancer: a new approach to preserving potency. Urology 60:109–114
Bahn DK, Silverman P, Lee F Sr et al (2006) Focal prostate cryoablation: initial results show cancer control and potency preservation. J Endourol 20:688–692
Muto S, Yoshii T, Saito K et al (2008) Focal therapy with high-intensity-focused ultrasound in the treatment of localized prostate cancer. Jpn J Clin Oncol 38:192–199
Shoji S, Nakano M, Fujikawa H et al (2015) Urethra-sparing high-intensity focused ultrasound for localized prostate cancer: functional and oncological outcomes. Int J Urol 22:1043–1049
Ahmed HU, Freeman A, Kirkham A et al (2011) Focal therapy for localized prostate cancer: a phase I/II trial. J Urol 185:1246–1254
Ahmed HU, Hindley RG, Dickinson L et al (2012) Focal therapy for localised unifocal and multifocal prostate cancer: a prospective development study. Lancet Oncol 13:622–632
Uchida T, Tomonaga T, Kim H et al (2015) Improved outcomes with advancements in high intensity focused ultrasound devices for the treatment of localized prostate cancer. J Urol 193:103–110
Shoji S, Nakano M, Nagata Y et al (2010) Quality of life following high-intensity focused ultrasound for the treatment of localized prostate cancer: a prospective study. Int J Urol 17:715–719
Crouzet S, Chapelon JY, Rouviere O et al (2014) Whole-gland ablation of localized prostate cancer with high-intensity focused ultrasound: oncologic outcomes and morbidity in 1002 patients. Eur Urol 65:907–914
Dhar N, Ward JF, Cher ML et al (2011) Primary full-gland prostate cryoablation in older men (> age of 75 years): results from 860 patients tracked with the COLD Registry. BJU Int 108:508–512
Peinemann F, Grouven U, Bartel C et al (2011) Permanent interstitial low-dose-rate brachytherapy for patients with localised prostate cancer: a systematic review of randomised and nonrandomised controlled clinical trials. Eur Urol 60:881–893
Chin J, Rumble RB, Kollmeier M et al (2017) Brachytherapy for patients with prostate cancer: American Society of Clinical Oncology/Cancer Care Ontario Joint Guideline Update. J Clin Oncol 35:1737–1743
Fry WJ, Barnard JW, Fry EJ et al (1955) Ultrasonic lesions in the mammalian central nervous system. Science 122:517–518
Madersbacher S, Pedevilla M, Vingers L et al (1995) Effect of high-intensity focused ultrasound on human prostate cancer in vivo. Cancer Res 55:3346–3351
Chapelon JY, Ribault M, Vernier F et al (1999) Treatment of localised prostate cancer with transrectal high intensity focused ultrasound. Eur J Ultrasound 9:31–38
Shoji S, Mouraviev V, Scionti S (2016) High intensity focused ultrasound (HIFU) treatment of prostate cancer. In: Bjerklund Johansen TE, Greene D, Breen DJ, Mouraviev V (eds) Handbook of focal therapy for prostate and renal cancer. JP Medical Ltd., London, pp 241–254
Valerio M, Ahmed HU, Emberton M (2015) Focal therapy of prostate cancer using irreversible electroporation. Tech Vasc Interv Radiol 18:147–152
American Society for Therapeutic Radiology and Oncology Consensus Panel (1997) Consensus statement: guidelines for PSA following radiation therapy. Int J Radiat Oncol Biol Phys 37:1035–1041
Roach M 3rd, Hanks G, Thames H Jr et al (2006) Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys 65:965–974
Ahmed HU, Dickinson L, Charman S et al (2015) Focal ablation targeted to the index lesion in multifocal localised prostate cancer: a prospective development study. Eur Urol 68:927–936
Feijoo ER, Sivaraman A, Barret E et al (2016) Focal high-intensity focused ultrasound targeted hemiablation for unilateral prostate cancer: a prospective evaluation of oncologic and functional outcomes. Eur Urol 69:214–220
Guillaumier S, Peters M, Arya M et al (2018) A multicentre study of 5-year outcomes following focal therapy in treating clinically significant nonmetastatic prostate cancer. Eur Urol 74:422–429
Ganzer R, Hadaschik B, Pahernik S et al (2018) Prospective multicenter phase II study on focal therapy (hemiablation) of the prostate with high intensity focused ultrasound. J Urol 199:983–989
Johnston MJ, Emara A, Noureldin M et al (2019) Focal high-intensity focused ultrasound partial gland ablation for the treatment of localised prostate cancer: a report of medium-term outcomes from a single-center in the United Kingdom. Urology 133:175–181
Stabile A, Orczyk C, Hosking-Jervis F et al (2019) Medium-term oncological outcomes in a large cohort of men treated with either focal or hemi-ablation using high-intensity focused ultrasonography for primary localized prostate cancer. BJU Int 124:431–440
Shah TT, Peters M, Eldred-Evans D et al (2019) Early-medium-term outcomes of primary focal cryotherapy to treat nonmetastatic clinically significant prostate cancer from a prospective multicentre registry. Eur Urol 76:98–105
Maenhout M, Peters M, Moerland MA et al (2018) MRI guided focal HDR brachytherapy for localized prostate cancer: toxicity, biochemical outcome and quality of life. Radiother Oncol 129:554–560
Peters M, van Son MJ, Moerland MA et al (2019) MRI-guided ultrafocal HDR brachytherapy for localized prostate cancer: median 4-year results of a feasibility study. Int J Radiat Oncol Biol Phys 104:1045–1053
Azzouzi AR, Emberton M, PCM301 study investigators (2017) Padeliporfin vascular-targeted photodynamic therapy versus active surveillance in men with low-risk prostate cancer—authors’ reply. Lancet Oncol 18:e188
van den Bos W, Scheltema MJ, Siriwardana AR et al (2018) Focal irreversible electroporation as primary treatment for localized prostate cancer. BJU Int 121:716–724
Donaldson IA, Alonzi R, Barratt D et al (2015) Focal therapy: patients, interventions, and outcomes–a report from a consensus meeting. Eur Urol 67:771–777
Scheltema MJ, Chang JI, Bohm M et al (2018) Pair-matched patient-reported quality of life and early oncological control following focal irreversible electroporation versus robot-assisted radical prostatectomy. World J Urol 36:1383–1389
Zheng X, Jin K, Qiu S et al (2019) Focal laser ablation versus radical prostatectomy for localized prostate cancer: survival outcomes from a matched cohort. Clin Genitourin Cancer 17:464–469.e3
Marconi L, Stonier T, Tourinho-Barbosa R et al (2019) Robot-assisted Radical prostatectomy after focal therapy: oncological, functional outcomes and predictors of recurrence. Eur Urol 76:27–30
Acknowledgements
The present study was supported by the Takeda Science Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Shoji, S., Hiraiwa, S., Hanada, I. et al. Current status and future prospective of focal therapy for localized prostate cancer: development of multiparametric MRI, MRI-TRUS fusion image-guided biopsy, and treatment modalities. Int J Clin Oncol 25, 509–520 (2020). https://doi.org/10.1007/s10147-020-01627-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01627-8