Abstract
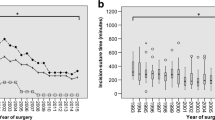
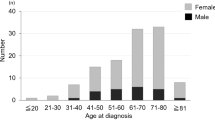
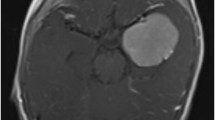
Radical excision of meningioma is suggested to provide for the best tumor control rates. However, aggressive surgery for meningiomas located at the posterior cranial fossa may lead to elevated postoperative morbidity of adjacent cranial nerves which in turn worsens patients’ postoperative quality of life. Therefore, we analyzed our institutional database with regard to new cranial nerve dysfunction as well as postoperative cerebrospinal fluid (CSF) leakage depending on the extent of tumor resection. Between 2009 and 2017, 89 patients were surgically treated for posterior fossa meningioma at the authors’ institution. Postoperative new cranial nerve dysfunction as well as CSF leakage were stratified into Simpson grade I resections with excision of the adjacent dura as an aggressive resection regime versus Simpson grade II–IV tumor removal. Simpson grade I resections revealed a significantly higher percentage of new cranial nerve dysfunction immediately after surgery (39%) compared with Simpson grade II (11%, p = 0.01) and Simpson grade II–IV resections (14%, p = 0.02). These observed differences were also present for the 12-month follow-up (27% Simpson grade I, 3% Simpson grade II (p = 0.004), 7% Simpson grades II–IV (p = 0.01)). Postoperative CSF leakage was present in 21% of Simpson grade I and 3% of Simpson grade II resections (p = 0.04). Retreatment rates did not significantly differ between these two groups (6% versus 8% (p = 1.0)). Elevated levels of postoperative new cranial nerve deficits as well as CSF leakage following radical tumor removal strongly suggest a less aggressive resection policy to constitute the surgical modality of choice for posterior cranial fossa meningiomas.

Similar content being viewed by others
References
Topsakal C, Al-Mefty O, Bulsara KR, Williford VS (2008) Intraoperative monitoring of lower cranial nerves in skull base surgery: technical report and review of 123 monitored cases. Neurosurg Rev 31(1):45–53. https://doi.org/10.1007/s10143-007-0105-5
Bassiouni H, Asgari S, Sandalcioglu IE, Seifert V, Stolke D, Marquardt G (2009) Anterior clinoidal meningiomas: functional outcome after microsurgical resection in a consecutive series of 106 patients. Clinical article. J Neurosurg 111(5):1078–1090. https://doi.org/10.3171/2009.3.17685
Turgut M, Ozcan OE, Benli K, Ozgen T, Gurcay O, Bertan V, Erbengi A, Saglam S (1996) Factors affecting morbidity and mortality following surgical intervention in patients with intracranial meningioma. Aust N Z J Surg 66(3):144–150. https://doi.org/10.1111/j.1445-2197.1996.tb01143.x
Chen CM, Huang AP, Kuo LT, Tu YK (2011) Contemporary surgical outcome for skull base meningiomas. Neurosurg Rev 34(3):281–296; discussion 296. https://doi.org/10.1007/s10143-011-0321-x
Neil-Dwyer G, Lang DA, Davis A (2000) Outcome from complex neurosurgery: an evidence based approach. Acta Neurochir 142(4):367–371
Schneider M, Schuss P, Güresir Á, Wach J, Hamed M, Vatter H, Güresir E (2019) Cranial nerve outcomes after surgery for frontal skull base meningiomas: the eternal quest of the maximum-safe resection with the lowest morbidity. World Neurosurg. https://doi.org/10.1016/j.wneu.2019.01.171
Castellano F, Ruggiero G (1953) Meningiomas of the posterior fossa. Acta Radiol Suppl 104:1–177
Goto T, Ohata K (2016) Surgical resectability of skull base meningiomas. Neurol Med Chir (Tokyo) 56(7):372–378. https://doi.org/10.2176/nmc.ra.2015-0354
Hye RJ, Mackey A, Hill MD, Voeks JH, Cohen DJ, Wang K, Tom M, Brott TG (2015) Incidence, outcomes, and effect on quality of life of cranial nerve injury in the Carotid Revascularization Endarterectomy versus Stenting Trial. J Vasc Surg 61(5):1208–1214. https://doi.org/10.1016/j.jvs.2014.12.039
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20(1):22–39. https://doi.org/10.1136/jnnp.20.1.22
Jaaskelainen J (1986) Seemingly complete removal of histologically benign intracranial meningioma: late recurrence rate and factors predicting recurrence in 657 patients. A multivariate analysis. Surg Neurol 26(5):461–469
Sughrue ME, Kane AJ, Shangari G, Rutkowski MJ, McDermott MW, Berger MS, Parsa AT (2010) The relevance of Simpson Grade I and II resection in modern neurosurgical treatment of World Health Organization Grade I meningiomas. J Neurosurg 113(5):1029–1035. https://doi.org/10.3171/2010.3.JNS091971
Couldwell WT, Heros R, Dolenc V (2011) Skull base meningiomas. Neurosurg Focus 30(5):1p prior to E1. https://doi.org/10.3171/2011.3.FOCUS1185
Seifert V (2010) Clinical management of petroclival meningiomas and the eternal quest for preservation of quality of life: personal experiences over a period of 20 years. Acta Neurochir 152(7):1099–1116. https://doi.org/10.1007/s00701-010-0633-6
Combs SE, Ganswindt U, Foote RL, Kondziolka D, Tonn JC (2012) State-of-the-art treatment alternatives for base of skull meningiomas: complementing and controversial indications for neurosurgery, stereotactic and robotic based radiosurgery or modern fractionated radiation techniques. Radiat Oncol 7:226. https://doi.org/10.1186/1748-717X-7-226
Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH (2012) Endoscopic endonasal versus open transcranial resection of anterior midline skull base meningiomas. World Neurosurg 77(5–6):713–724. https://doi.org/10.1016/j.wneu.2011.08.025
Faramand A, Kano H, Niranjan A, Johnson SA, Hassib M, Park KJ, Arai Y, Flickinger JC, Lunsford LD (2018) Cranial nerve outcomes after primary stereotactic radiosurgery for symptomatic skull base meningiomas. J Neuro-Oncol 139(2):341–348. https://doi.org/10.1007/s11060-018-2866-9
Kondziolka D, Flickinger JC, Perez B (1998) Judicious resection and/or radiosurgery for parasagittal meningiomas: outcomes from a multicenter review. Gamma Knife Meningioma Study Group. Neurosurgery 43(3):405–413; discussion 413–404. https://doi.org/10.1097/00006123-199,809,000-00001
Kondziolka D, Levy EI, Niranjan A, Flickinger JC, Lunsford LD (1999) Long-term outcomes after meningioma radiosurgery: physician and patient perspectives. J Neurosurg 91(1):44–50. https://doi.org/10.3171/jns.1999.91.1.0044
Chuang CC, Chang CN, Tsang NM, Wei KC, Tseng CK, Chang JT, Pai PC (2004) Linear accelerator-based radiosurgery in the management of skull base meningiomas. J Neuro-Oncol 66(1–2):241–249
Hasegawa T, Kida Y, Yoshimoto M, Koike J, Iizuka H, Ishii D (2007) Long-term outcomes of Gamma Knife surgery for cavernous sinus meningioma. J Neurosurg 107(4):745–751. https://doi.org/10.3171/JNS-07/10/0745
Iwai Y, Yamanaka K, Ikeda H (2008) Gamma Knife radiosurgery for skull base meningioma: long-term results of low-dose treatment. J Neurosurg 109(5):804–810. https://doi.org/10.3171/JNS/2008/109/11/0804
Mendenhall WM, Morris CG, Amdur RJ, Foote KD, Friedman WA (2003) Radiotherapy alone or after subtotal resection for benign skull base meningiomas. Cancer 98(7):1473–1482. https://doi.org/10.1002/cncr.11645
Samii M, Tatagiba M (1992) Experience with 36 surgical cases of petroclival meningiomas. Acta Neurochir 118(1–2):27–32
Al-Mefty O, Fox JL, Smith RR (1988) Petrosal approach for petroclival meningiomas. Neurosurgery 22(3):510–517. https://doi.org/10.1227/00006123-198,803,000-00010
Samii M, Ammirati M, Mahran A, Bini W, Sepehrnia A (1989) Surgery of petroclival meningiomas: report of 24 cases. Neurosurgery 24(1):12–17. https://doi.org/10.1227/00006123-198,901,000-00003
Spetzler RF, Daspit CP, Pappas CT (1992) The combined supra- and infratentorial approach for lesions of the petrous and clival regions: experience with 46 cases. J Neurosurg 76(4):588–599. https://doi.org/10.3171/jns.1992.76.4.0588
Zentner J, Meyer B, Vieweg U, Herberhold C, Schramm J (1997) Petroclival meningiomas: is radical resection always the best option? J Neurol Neurosurg Psychiatry 62(4):341–345. https://doi.org/10.1136/jnnp.62.4.341
Roberti F, Sekhar LN, Kalavakonda C, Wright DC (2001) Posterior fossa meningiomas: surgical experience in 161 cases. Surg Neurol 56(1):8–20 discussion 20–21
Javalkar V, Banerjee AD, Nanda A (2012) Posterior cranial fossa meningiomas. J Neurol Surg B Skull Base 73(1):1–10. https://doi.org/10.1055/s-0032-1,304,835
D’Amico RS, Banu MA, Petridis P, Bercow AS, Malone H, Praver M, Wang TJC, Isaacson SR, Sisti MB (2017) Efficacy and outcomes of facial nerve-sparing treatment approach to cerebellopontine angle meningiomas. J Neurosurg 127(6):1231–1241. https://doi.org/10.3171/2016.10.JNS161982
Mariniello G, Maiuri F, Strianese D, Donzelli R, Iuliano A, Tranfa F, de Divitiis E, Bonavolonta G (2008) Spheno-orbital meningiomas: surgical approaches and outcome according to the intraorbital tumor extent. Zentralbl Neurochir 69(4):175–181. https://doi.org/10.1055/s-2008-1,077,077
de Divitiis E, Esposito F, Cappabianca P, Cavallo LM, de Divitiis O (2008) Tuberculum sellae meningiomas: high route or low route? A series of 51 consecutive cases. Neurosurgery 62(3):556–563; discussion 556–563. https://doi.org/10.1227/01.neu.0000317303.93460.24
Lobato RD, Gonzaaez P, Alday R, Ramos A, Lagares A, Alen JF, Palomino JC, Miranda P, Perez-Nunez A, Arrese I (2004) Meningiomas of the basal posterior fossa. Surgical experience in 80 cases. Neurocirugia (Astur) 15(6):525–542
Saleh EA, Taibah AK, Achilli V, Aristegui M, Mazzoni A, Sanna M (1994) Posterior fossa meningioma: surgical strategy. Skull Base Surg 4(4):202–212. https://doi.org/10.1055/s-2008-1,058,956
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The present study was approved by the local ethics committee at the University of Bonn.
Informed consent
Informed consent was not sought as a retrospective design was used.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schneider, M., Schuss, P., Güresir, Á. et al. Surgery for posterior fossa meningioma: elevated postoperative cranial nerve morbidity discards aggressive tumor resection policy. Neurosurg Rev 44, 953–959 (2021). https://doi.org/10.1007/s10143-020-01275-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01275-6