Abstract
Glioblastoma is the most malignant and most common primary brain tumour and is treated with resection followed by post-operative radiotherapy and chemotherapy. However, a significant amount of patients are older than 80 years, and such an approach may not be appropriate. Data on patients aged 80 or older with glioblastoma from two hospitals was collected using the CNS Tumour Database on the Australian Comprehensive Cancer Outcomes and Research Database (ACCORD) system operated by BioGrid. Between 2008 and July 2011, 40 patients aged 80 years or older were diagnosed with glioblastoma. The median ECOG PS was 2 and the ASA score was 3. All 40 patients underwent surgery and 33 % had a gross total resection. Only six patients (15 %) had either post-operative radiotherapy or chemotherapy. The overall median survival was 4 months (range 0–18 months) and 28 % of patients lived between 6 and 24 months. This is the largest reported cohort of very elderly patients with glioblastoma. Patients tolerated surgery but few went on to receive post-operative radiotherapy or chemotherapy. This patient population requires special attention and in particular would benefit from participation in suitable clinical trials to determine the best care regime.
Similar content being viewed by others
References
Chaichana KL, Chaichana KK, Olivi A et al (2011) Surgical outcomes for older patients with glioblastoma multiforme: pre-operative factors associated with decreased survival. J Neurosurg 114:587–594
Nghiemphu P, Cloughesy T (2012) Glioblastoma therapy in the elderly: one age does not fit all. Lancet Oncol 13(9):857–858
Keime-Guibert F, Chinot O, Taillandier L et al (2007) Radiotherapy for glioblastoma in the elderly. NEJM 356:1527–1535
Minitti G, Muni R, Lanzetta G et al (2009) Chemotherapy for glioblastoma: current treatment and future perspectives for cytotoxic and targeted agents. Anticancer Res 29(12):5171–5184
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomized phase II study: 5 year analysis of the EORTC-NCIC trial. Lancet 10:459–466
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. NEJM 352(10):987–996
Laperriere N, O’Callaghan C, Ding K et al (2008) Rationale and design for a phase III randomized controlled trial in elderly patients with glioblastoma multiforme: NCIC CTG CE Canadian Neuro-oncology Annual Scientific Meeting
Scott JG, Suh JH, Elson P et al (2011) Aggressive treatment is appropriate for glioblastoma multiforme patients 70 years or older: a retrospective review of 206 cases. Neuro-Oncology 13(4):428–436
Balducci L (2000) Geriatric oncology: challenges for the new century. Eur J Cancer 36:1741–1754
Brandes A, Vastola F, Basso U et al (2003) A prospective study of glioblastoma in the elderly. Cancer 97(3):657–662
Iwamoto FM, Reiner A, Panageas KS, Elkin EB, Abrey LE (2008) Patterns of care in elderly glioblastoma. Ann Neurol 64:628–634
Kita D, Ciernik F, Vaccarella S et al (2009) Age as a predictive factor in glioblastomas: population based study. Neuroepidemiology 33:17–22
Bauchet L, Zouaoui S, Darlix A et al (2014) Assessment and treatment relevance in elderly glioblastoma patients. Neuro-Oncol 16: 1459−1468
Organisation: BioGrid Australia https://www.biogrid.org.au
Reifenberger G, Hentschel B, Felsberg J et al (2012) Predictive impact of MGMT promoter methylation in glioblastoma of the elderly. Int J Cancer 131(6):1342–1350
Cancer Council Australia/Australian Cancer Network/Clinical Oncological Society of Australia Inc. (2009) Clinical practice guidelines for the treatment of adult gliomas: astrocytomas and oligodendromas
Scott JG, Bauchet L, Fraum TJ et al (2012) Recursive partitioning analysis of prognostic factors for glioblastoma patients aged 70 years or older. Cancer 118(22):5595–5600
Malmstrom A, Gronbberg BH, Marosi C et al (2012) Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol 13:916–926
Wick W, Platten M, Mmeisnner C et al (2012) Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomized, phase 3 trial. Lancet Oncol 13:707–715
Paszat L, Laperriere N, Groome et al (2001) A population based study of glioblastoma multiforme. Int J Radiat Oncol Biol Phys 51:100–107
Hartmann C, Hentschel B, Wick W et al (2010) Patients with IDH1 wildtype anaplastic astrocytomas exhibit worse prognosis than IDH1-mutated glioblastomas and IDH1 mutation status accounts for the unfavourable prognostic effect of higher age: implications for classification of gliomas. Acta Neuropathol 120:707–718
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Luc Bauchet, Montpellier, France
Glioblastoma (GBM) is the most common malignant primary brain tumor. Its incidence continues to increase in the elderly group because the older segment of the population is growing faster than any other age group. In the USA for the 2007–2011 period, GBM incidence-adjusted rates for patients aged 65–74 and 75–84 years were 13.1 and 15 per 100,000 person-years, respectively (Ostrom et al. 2014), and these incidences will keep increasing in the near future. Most clinical studies exclude elderly patients, “standards of care” do not exist for GBM patients aged >70 years (Bauchet et al. 2014), and very rare studies have described oncological care management for “very elderly” GBM patients.
Of course, age is one of the most important prognostic factors in GBM patients, but three important papers about elderly GBM patients showed first that resection was the preliminary node in a Recursive Partitioning Analysis (RPA) of prognostic factors for GBM patients aged 70 years or older (Scott et al. 2012). Secondly, the most relevant clinical predictive factor in elderly GBM patients was the Karnofsky Performance Status (KPS) (Zouaoui et al. 2014), and thirdly, comorbidity and geriatric evaluation were important for therapeutic decision (Bauchet et al. 2014). Furthermore, in the absence of clinical trials, database and population studies are very important and complementary sources for evaluating oncological results in “real life.”
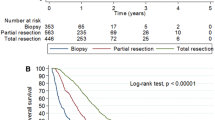
Here, Felicity V Connon and co-workers present the largest reported cohort of “very elderly” GBM patients, including data of the American Society of Anesthesiologists (ASA) score and Eastern Cooperative Oncology Group (ECOG) score at diagnosis (40 patients aged 80 years or older, from the Australian Comprehensive Cancer Outcomes and Research Database—ACCORD). This paper describes epidemiological data, medical and surgical postoperative complications, and therapeutics for GBM patients aged 80 years or older. The authors confirmed that the prognosis is globally very poor (median overall survival, 4.7 months), but survival ranged between 0.3 and 30 months. They showed in this “very elderly” population that regardless of age, there is a survival benefit for surgical resection over biopsy alone, and some patients benefited from oncological treatment after the surgery.
The number of patients is not enough to provide sufficient clinical statistical data to give specific cutoff about performance status and comorbidity in this frail population. In very elderly patient, optimal treatment must be carefully considered to ensure quality of life is not compromised for small survival gains. However, the fact that a perfect setting is not available at the moment should not discourage teams to intensively develop tumor networks and databases.
References
Bauchet L, Zouaoui S, Darlix A, Menjot de Champfleur N, Ferreira E, Fabbro M, Kerr C, Taillandier L. Assessment and treatment relevance in elderly glioblastoma patients. Neuro Oncol. 2014 Nov;16(11):1459–68.
Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, Wolinsky Y, Kruchko C, Barnholtz-Sloan J. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol. 2014 Oct;16 Suppl 4:iv1-63.
Scott JG, Bauchet L, Fraum TJ, Nayak L, Cooper AR, Chao ST, Suh JH, Vogelbaum MA, Peereboom DM, Zouaoui S, Mathieu-Daudé H, Fabbro-Peray P, Rigau V, Taillandier L, Abrey LE, DeAngelis LM, Shih JH, Iwamoto FM. Recursive partitioning analysis of prognostic factors for glioblastoma patients aged 70 years or older. Cancer. 2012 Nov 15;118(22):5595–600.
Zouaoui S, Darlix A, Fabbro-Peray P, Mathieu-Daudé H, Rigau V, Fabbro M, Bessaoud F, Taillandier L, Ducray F, Bauchet F, Wager M, Faillot T, Capelle L, Loiseau H, Kerr C, Menei P, Duffau H, Figarella-Branger D, Chinot O, Trétarre B, Bauchet L. Oncological patterns of care and outcomes for 265 elderly patients with newly diagnosed glioblastoma in France. Neurosurg Rev. 2014 Jul;37(3):415–23; discussion 423–4.
Lennea E Coombs, Renato V LaRocca, Louisville, USA
In the context of the aging population of the Western world, this study serves as an initial benchmark for treatment outcome of patients over age 80 diagnosed with glioblastoma (GBM). While the treatment received may not be considered state of the art for the newly diagnosed GBM population in general, this retrospective analysis is an important first step in determining appropriate intervention for this elderly patient cohort. Therapy for glioblastoma has evolved over the last decade, in no small measure as a result of our improved understanding of the molecular and biologic intricacies of the neoplastic process. For younger patients with an acceptable performance status, it is clear that some form of treatment for GBM appears to be better than supportive care alone. This elderly population however, often presents with significant comorbidities and it is unfortunate that to date they have been severely underrepresented in clinical trials. Considering their limited life expectancy, it is meaningful to be able to consider palliative treatment options with a clear understanding of their impact not only on outcome but also on quality of life. Additional focused prospective trials are needed to assist these elderly patients and their families to make informed decisions regarding their care.
Fumio Yamaguchi, Tokyo, Japan
The authors reported and discussed very elderly glioblastoma (GBM) patients. The right treatment for very elderly patients must be discussed for many diseases especially which are not curable with simple therapies. The GBM is one of such disease. Since the perisurgical complications are often experienced in the very elderly patients, the non-surgical therapies may be considered with qualitative image and molecular diagnosis or minimally invasive biopsy in the future, even though there are patients who can tolerate surgery and postop treatments. The issue that is reported in this paper is essentially very important when we consider patients’ quality of life in our super-aging society. The accurate evaluations of individual patient to predict complications are the issues that have to be fixed.
Synopsis: The clinical experience and treatment outcomes of the largest reported cohort of elderly patients (>80 years old) with glioblastoma. Can the current gold standard treatment be applied to the very elderly safely and appropriately?
Rights and permissions
About this article
Cite this article
Connon, F.V., Rosenthal, M.A. & Drummond, K. Glioblastoma multiforme in the very elderly. Neurosurg Rev 39, 55–61 (2016). https://doi.org/10.1007/s10143-015-0652-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0652-0