Abstract
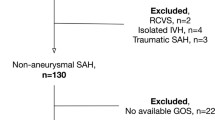
The aim of this study was to investigate the long-term natural history of nontraumatic angiogram-negative subarachnoid hemorrhage with typical pretruncal (P-SAH) and diffuse (D-SAH) pattern of hemorrhage. A retrospective review of 102 patients who experienced angiographically negative SAH at our institution was undertaken (11.6% of 882 spontaneous SAH). Follow-ups were obtained at 7.9 to 16 years. In the D-SAH group, 11 patients (13.9%) out of 79 had an aneurysm, and four (5.1%) had rebleeding episodes. In the P-SAH group, the second angiography was negative in all of the 23 cases, and no rebleeding episodes were recorded. The long-term follow-up confirms that P-SAH is a benign disease. A second angiography could not be necessary. D-SAH is probably due to an aneurysm that thrombose early after the bleeding. At short-term follow-up, the sack could frequently recanalize and rebleed, whereas a late follow-up shows that rebleeding is very rare.

Similar content being viewed by others
References
Alén JF, Lagares A, Lobato RD, Gómez PA, Rivas JJ, Ramos A (2003) Comparison between perimesencephalic nonaneurysmal subarachnoid hemorrhage and subarachnoid hemorrhage caused by posterior circulation aneurysms. J Neurosurg 98:529–535
Alexander MS, Dias PS, Uttley D (1986) Spontaneous subarachnoid hemorrhage and negative cerebral panangiography. Review of 140 cases. J Neurosurg 64:537–542
Bradac GB, Bergui M, Ferrio M, Fontanella M, Stura G (1997) False-negative angiograms in subarachnoid haemorrhage due to intracranial aneurysms. Neuroradiology 39:772–776
Cioffi F, Pasqualin A, Cavazzani P, Da Pian R (1989) Subarachnoid haemorrhage of unknown origin: clinical and tomographical aspects. Acta Neurochir 97:31–39
Cossandi C, Griva F, Fontanella M, Zullo N, Bergui M, Bradac GB, Pagni CA (2000) Calloso-marginal artery aneurysm missed by three angiographic studies. Acta Neurochir 142:1315–1316
Duong H, Melancon D, Tampieri D, Ethier R (1996) The negative angiogram in subarachnoid haemorrhage. Neuroradiology 38:15–19
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 16:1–9
Fontanella M, Perozzo P, Ursone R, Garbossa D, Bergui M (2003) Neuropsychological assessment after microsurgical cliping or endovascular treatment for anterior communicating artery aneurysm. Acta Neurochir 145:867–872
Fontanella M, Valfrè W, Benech F, Carlino C, Garbossa D, Ferrio M, Perez R, Berardino M, Bradac GB, Ducati A (2008) Vasospasm after SAH due to aneurysm rupture of the anterior circle of Willis: value of TCD monitoring. Neurol Res 30:256–261
Forster DM, Steiner L, Hakanson S, Bergvall U (1978) The value of repeat pan-angiography in cases of unexplained subarachnoid haemorrhage. J Neurosurg 48:712–716
Gascón P, Ley TJ, Toltzis RJ, Bonow RO (1983) Spontaneous subarachnoid hemorrhage simulating acute transmural myocardial infarction. Am Heart J 105:511–513
Giombini S, Bruzzone MG, Pluchino F (1988) Subarachnoid hemorrhage of unexplained cause. Neurosurgery 22:313–316
Hui FK, Tumialán LM, Tanaka T, Cawley CM, Zhang YJ (2009) Clinical differences between angiographically negative, diffuse subarachnoid hemorrhage and perimesencephalic subarachnoid hemorrhage. Neurocrit Care 11:64–70
Hunt WE, Hess RM (1968) Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 28:14–20
Hurley TR, Balandrin J (1997) Perimesencephalic nonaneurysmal subarachnoid hemorrhage: review of the literature. Neurosurgery 40:885
Iwanaga H, Wakai S, Ochiai C, Narita J, Inoh S, Nagai M (1990) Ruptured cerebral aneurysm missed by initial angiographic study. Neurosurgery 27:45–51
Jafar JJ, Weiner HL (1993) Surgery for angiographically occult cerebral aneurysms. J Neurosurg 79:674–679
Jung JY, Kim YB, Lee JW, Huh SK, Lee KC (2006) Spontaneous subarachnoid haemorrhage with negative initial angiography: a review of 143 cases. J Clin Neurosci 13:1011–1017
Kitahara T, Ohwada T, Tokiwa K, Kurata A, Miyasaka Y, Yada K, Kan S (1993) Clinical study in patients with perimesenscephalic subarachnoid haemorrhage of unknown etiology. No Shinkei Geka 21:903–908
Pinto AN, Ferro JM, Canhao P, Campos J (1993) How often is a perimesencephalic subarachnoid haemorrhage CT pattern caused by ruptured aneurysms? Acta Neurochir 124:79–81
Rijnkel GJ, van Gijn J, Wijdicks EF (1993) Subarachnoid hemorrhage without detectable aneurysm. A review of the causes. Stroke 24:1403–1409
Rijnkel GJ, Wijdicks EF, Vermeulen M, Hageman LM, Tans JT, van Gijn J (1990) Outcome in perimesencephalic (nonaneurysmal) subarachnoid hemorrhage: a follow-up study in 37 patients. Neurology 40:1130–1132
Rijnkel GJ, Wijdicks EF, Vermeulen M, Hasan D, Brouwers PJ, van Gijn J (1991) The clinical course of perimesencephalic nonaneurysmal subarachnoid hemorrhage. Ann Neurol 29:463–468
Rijnkel GJ, Wijdicks EF, Vermeulen M, Ramos LM, Tanghe HL, Hasan D, Meiners LC, van Gijn J (1991) Nonaneurysmal perimesencephalic subarachnoid hemorrhage: CT and MR patterns that differ from aneurysmal rupture. AJNR Am J Neuroradiol 12:829–834
Ronkanien A, Hernesniemi J (1992) Subarachnoid haemorrhage of unknown aetiology. Acta Neurochir 119:29–34
Rogg JM, Smeaton S, Doberstein C, Goldstein JH, Tung GA, Haas RA (1999) Assesment of the value of MR imaging for examining patients with angiographically negative subarachnoid hemorrhage. Am J Roentgenol 172:201–206
Schievnik WI, Wijdicks EF (1997) Pretruncal subarachnoid hemorrhage: an anatomically correct description of the perimesencephalic subarachnoid hemorrhage. Stroke 28:2572
Schievnik WI, Wijdicks EF, Piepgras DG, Nichols DA, Ebersold MJ (1994) Perimesencephalic subarachnoid hemorrhage. Additional perspectives from four cases. Stroke 25:1507–1511
Schwartz TH, Mayer SA (2000) Quadrigeminal variant of perimesencephalic nonaneurysmal subarachnoid hemorrhage. Neurosurgery 46:584–588
Schwartz TH, Solomon RA (1996) Perimesencephalic nonaneurysmal subarachnoid hemorrhage: review of the literature. Neurosurgery 39:433–440
Tatter SB, Crowell RM, Ogilvy CS (1995) Aneurysmal and microaneurysmal “angiogram-negative” subarachnoid hemorrhage. Neurosurgery 37:48–55
Topcuoglu MA, Ogilvy CS, Carter BS, Buonanno FS, Koroshetz WJ, Singhal AB (2003) Subarachnoid hemorrhage without evident cause on initial angiography studies: diagnostic yield of subsequent angiography and other neuroimaging tests. J Neurosurg 98:1235–1240
van der Worp HB, Fonville S, Ramos LM, Rinkel GJ (2009) Recurrent perimesencephalic subarachnoid hemorrhage during antitrombotic therapy. Neurocrit Care 10:209–212
Velthuis BK, Rinkel GJ, Ramos LM, Witkamp TD, van Leeuwen MS (1999) Perimesencephalic hemorrhage. Exclusion of vertebrobasilar aneurysms with CT angiography. Stroke 30:1103–1109
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Deanna Sasaki-Adams, Saint Louis, USA
The manuscript entitled, “Subarachnoid Hemorrhage and Negative Angiography: Clinical Course and Long-term Follow-up” submitted by Dr. Fontanella et al. seeks to evaluate radiographic and clinical characteristics that differentiate between diffuse and perimesencephalic angiographically negative subarachnoid hemorrhage. It has been customary in many institutions to perform two to three angiograms in these patients to confirm no aneurysmal origin of the subarachnoid hemorrhage. Fontanella et al. have demonstrated that a second angiogram may not be necessary in those patients whose initial CT scan shows blood limited to the area just anterior to the midbrain without significant extension into the interhemispheric fissures or ambient cisterns. In a retrospective review of 79 patients with angiogram negative for underlying aneurysm, 23 patients were defined as having a characteristic pattern in the perimesencephalic region as opposed to a more diffuse pattern of hemorrhage. None of those patients labeled with perimesencephalic hemorrhage alone were found to have a lesion upon repeat angiography, and all demonstrated a benign clinical course. The data suggest that a repeat arteriogram in a select group of patients may not be necessary. The present study supports what many neurosurgeons have found to be true anecdotally and will add to our armamentarium when dealing with these often challenging scenarios in an evidence-driven and cost-effective manner.
Giuseppe Lanzino, Emanuela Crobeddu, Rochester, MN, USA
Fontanella and coworkers retrospectively analyzed a consecutive series of patients with subarachnoid hemorrhage (SAH) and no evidence of aneurysm on first catheter angiography. Patients were followed for a mean of 10.6 years. Two groups are considered: patients with “classic” pretruncal SAH (23 patients) and those with a diffuse pattern suggestive of aneurysm rupture (72 patients). Patients underwent a “second look” angiography between day 11 and day 20 after SAH. In patients with diffuse SAH, the second angiogram revealed an aneurysm in nine out of 72 (12.5%), and four patients in this group suffered a rebleeding before a definitive diagnosis of the aneurysm. Angiography-negative SAH continues to be not an uncommon diagnosis among patients with nontraumatic SAH despite sophisticated and ever improving diagnostic imaging.
Patients with a classic pattern of pretruncal hemorrhage share other clinical characteristics, namely good clinical “appearance” on presentation, a relatively benign course (even though they can occasionally suffer from vasospasm and hydrocephalus), and a uniformly good outcome. We agree with the authors that in patients with a “classic” pattern a high-quality six-vessel angiogram suffices and no repeat imaging studies are necessary. Patients with a diffuse, “true” aneurysmal pattern continue to represent a challenge. It has been our experience that with modern 3D angiography capabilities, these patients are less common than a few decades ago. In these patients, careful search of an offending underlying vascular cause is imperative given the risk of rebleeding. We routinely perform a “second look” catheter angiography in this group. The timing of the repeat angiogram in this situation is controversial. However, this study suggests that another catheter angiography should probably be performed 1 week after presentation since the four rebleedings observed occurred between days 3 and 17.
We have noticed that more and more patients with angiography-negative SAH fall within a third category: the “pretruncal plus” pattern. In this category, the epicenter of the bleeding is still in the area of the interpeduncular cistern, but the subarachnoid blood extends beyond the confines considered “classic” for the pretruncal type such as the distal sylvian fissure and the distal two thirds of the interhemispheric fissure. We have noted (a finding corroborated by others) that often these patients are on antiplatelet or anticoagulation therapy. Therefore, it is conceiveable that in some of these cases, the bleeding originates from the same source which gives rise to the “classic” pretruncal pattern, but the blood burden may be increased by the pharmacological effects of the antiplatelet/anticoagulant treatment allowing for extension beyond the boundaries of the pretruncal type. In these patients, we perform a “second look” catheter angiography only selectively and often consider a noninvasive method instead. Future research will likely further characterize this specific subgroup.
One final word about the use of axial imaging studies such as MRI of the brain and cervical spine. These have been traditionally recommended to rule out possible, less common causes of SAH such as cavernous malformations or the sporadic tumor (usually ependymoma or schwannoma). For the past 9 years, we have been doing axial imaging of the brain and the cervical spine routinely in patients with angiography-negative SAH, but in accordance with Fontanella and coworkers’ findings, we have not found these studies useful. We now consider MRI of the brain and cervical spine only selectively in those patients with atypical features or when symptom onset clearly suggests a possible upper spinal origin of the bleed (i.e., sudden, severe pain starting in the spine, and then migrating upward).
Rights and permissions
About this article
Cite this article
Fontanella, M., Rainero, I., Panciani, P.P. et al. Subarachnoid hemorrhage and negative angiography: clinical course and long-term follow-up. Neurosurg Rev 34, 477–484 (2011). https://doi.org/10.1007/s10143-011-0323-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0323-8