Abstract
Epstein–Barr virus-associated gastric cancer [EBV-associated GC, EBV( +) GC] is a distinct molecular subtype of gastrointestinal (GI) cancers. It accounts for up to 10% of all molecular subtypes of gastric cancer (GC). It has unique genetic and epigenetic features, which determine its definitive phenotype with male and younger age predominance, proximal stomach localization, and diffuse adenocarcinoma histology. EBV( +) GC also has a unique epigenetic profile and mutational status with frequent mutations of PIK3CA, ARID1A and BCOR, and PD-L1 and PD-L2 amplifications, as well. The aim of this review is to highlight clinical significance of EBV( +) GC and prognostic role of EBV infection, and to determine potentially appropriate drug therapy for this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epstein–Barr virus-associated gastric cancer [EBV-associated GC, EBV( +) GC] is a gastric adenocarcinoma that develops secondary to clonal growth of EBV-infected epithelial cells of the gastric mucosa [1]. This cancer type has unique genetic and epigenetic features, which determine its definitive phenotype [2]. Molecular characterization of EVB-associated GC reveals potential targets for drug treatment [3]. Here, we discuss current data on epidemiology and pathogenesis of EBV-associated GC and describe its unique pathological and molecular features. We pay a special attention to the clinical significance of EBV( +) GC, prognostic role of EBV infection, and potentially appropriate drug therapy.
Molecular subtypes of GC
In 2014, The Cancer Genome Atlas (TCGA) project got us closer to understanding GC biology. A full-scale molecular genetic analysis, published by TCGA, identified four molecular subtypes of GC: (1) Epstein–Barr virus-associated GC, (2) GC with microsatellite instability (MSI GC), (3) GC with chromosomal instability (CIN GC), and (4) genetically stable GC (GS GC) [4]. In 2018, with molecular genetic analysis of 921 primary gastrointestinal (GI) adenocarcinomas (e.g., GC), Hinoue T. et al. isolated the fifth subtype of GI tumors: hypermutated with single-nucleotide variants (hypermutated-SNV, HM-SNV) [3].
Next step towards understanding GC involved a pooled TCGA analysis of GI adenocarcinomas (esophagus, stomach, and colon). TCGA project first determined EBV status of the GI adenocarcinoma samples. Then, they divided EBV-negative GI tumors into two groups due to their mutational load: GI adenocarcinomas with high mutational load and GI adenocarcinomas with low mutational load. Adenocarcinomas with high mutation load (hypermutated: > 10 mutations per million nucleotides) were divided into MSI and SNV subtypes. Hinoue T. et al. considered hypermutated tumors (insertion and deletion density > 1 mutations per million nucleotides and indel/SNV ratio of > 1/150) as MSI phenotype, and others were considered SNV subtype. Adenocarcinomas with low mutational load, in their turn, were divided into two groups according to the presence or absence of somatic copy-number alterations (SCNAs): tumors with chromosomal instability (CIN) and genetically stable subtype (GS).
The pooled TCGA analysis of GI adenocarcinomas indicated that EBV( +) tumors localized only in the stomach and they characterized by the highest degree of genome hypermethylation among all other types of tumors [3].
Characteristics of EBV( +) GC
EBV-associated GC has distinct clinicopathologic characteristics (Table 1). The prevalence of EBV-associated GC among other molecular subtypes is about 10% (1.3–20.1%) [4]. Lee et al. point out that this GC subtype is more common among men than among women and in the younger age group than EBV-negative gastric tumors [5]. Despite endemic areas with a high prevalence of EBV( +) malignant neoplasms (Burkitt's lymphoma and nasopharyngeal carcinoma), EBV-associated GC is widespread [2], but most common for Zambia and Brunei where it reaches up to 23–30% [1].
EBV( +) GC is usually localized in the proximal stomach (the cardial section and body) and has a diffuse histological type according to Lauren classification [2]. Macroscopically, EBV( +) GC is usually ulcerative or saucer-like cancer with significant thickening of the gastric wall [6]. There also could be synchronous multiple EBV( +) gastric carcinomas [2].
Endoscopically, EBV( +) GC tends to appear as superficially depressed lesions with wall thickening in the early stages or ulcerated lesions without definite limits in advanced stages. These endoscopic characteristics, when combined with diffuse-type histology, lymphoid infiltration, and location of the lesion in the proximal stomach, strongly suggest EBV positivity [7]. A distinctive endosonographic finding of GC that also points to EBV positivity is the presence of hypoechoic submucosal nodules (the nodules of lymphoid stroma) [8].
Early EBV( +) GCs are more likely to form well-demarcated, nodular lesions in the submucosa with less fibrosis and no lymph-node metastasis, as opposed to EBV-negative gastric carcinoma, making them more available for endoscopic submucosal resection [9]. Indeed, favorable clinical outcomes in early EBV( +) GC treated with endoscopic submucosal dissection have been reported repeatedly EBV( +) GC [10, 11].
Among all molecular subtypes of GI adenocarcinomas, EBV( +) GC has the greatest immunogenicity [12]. This subtype has high expression of PD-L1 and PD-L2, enriched with CD8 + tumor-infiltrating lymphocytes (TILs), as well as a high level of expression of immunogenic pathway genes, such as the IFN–gamma signaling pathway [3, 12, 13].
Pathogenesis of EBV( +) GC
The mechanism of Epstein–Barr virus invasion of the gastric epithelial cells is still not fully understood. Since gastric epithelial cells do not express CD21, which serves as a B-lymphocyte surface receptor for viral particle penetration, the virus is supposed to invade the epithelial cells of the stomach in some other manner [14]. However, Chesnokova LS et al. estimate that gHgL viral protein forms a complex with integrins αvβ5, αvβ6, or αvβ8, leading to fusion of the virus with the host cell [15]. The virus might transfer to the epithelial cells from EBV-infected gastric mucosal B lymphocytes with reactivation of the infection [2].
EBV( +) GC is characterized by monoclonal growth of virus-infected cells. Clonality of the viral genome indicates that EBV infection is an early stage of carcinogenesis [16]. Fukayama M et al. assume that, initially, one or several virus-infected cells of gastric mucosa undergo malignant transformation and further promote clonal growth of the epithelial cells [17]. Multifunctional viral nuclear protein EBNA-1 is supposed to be responsible for maintaining viral infection in tumor cells. This protein interacts with cell complex that recognizes replication origin, mediating the attachment of this complex to the viral DNA replication origin (OriP). Thus, EBV uses the host cell system for its own reproduction in the S phase of the cell cycle [18].
Epigenetic regulation of viral and cellular gene expression plays an important role in viral oncogenesis in the development of EBV-associated tumors. In case of a latent infection, EBV DNA with lytic phase genes is significantly methylated. When infection is reactivated, the viral transcription factor Zta (ZEBRA, Z, BZLF1) selectively binds to the methylated promoters of the lytic phase genes, and thus, latent infection becomes the lytic one [19]. Methylation of CpG dinucleotides of the gene promotors of the latent phase is essential for maintaining latent infection.
Kang et al. showed that in the presence of EBV infection, the methylation of CpG sites of promoter regions of host cell genes is as common as the methylation of viral DNA [20]. It is important that hypermethylation in EBV infection has not random but naturally determined character instead. However, the regulatory mechanisms of this process have not been studied yet.
Matsusaka et al. analyzed DNA methylation profile of gastric adenocarcinomas and identified three different tumor epigenotypes: EBV(–)/low methylation, EBV(–)/high methylation, and EBV( +)/high methylation. EBV-negative epigenotypes with high methylation are distinguished by methylation of genes that serve as targets of polycomb group proteins (chromatin remodeling complex) in contrast to EBV( +) subtype, when methylation of other genes was detected (e.g., p14, p16, and E-cadherin) [16]. It proves that epigenetic profile of EBV( +) gastric tumors is unique.
Matsusaka et al. also showed that viral DNA methylation preceded host DNA methylation, suggesting that epigenetic inactivation of viral genes could be a protective mechanism of the host cell, which serves to suppress the expression of foreign DNA genes [21]. According to another hypothesis, the virus itself starts methylation [22]. In any case, excessive methylation may lead to negative consequences such as suppression of latent-phase genes, resulting in transition of the infection to the active phase, as well as silencing of tumor suppressor genes [23]. Interestingly, methylation pattern which never includes unpaired base repair genes (MRR) determines the difference between this type of tumor and MSI-H-associated GC [24]. Overall, epigenetic regulation plays an important role in the development of EBV( +) GC.
Malignant transformation of epithelial cells in EBV( +) GC is also likely to be facilitated by microRNAs, which are small non-coding RNAs involved in the regulation of gene expression. MicroRNAs complementarily bind to regions of the target mRNA and inhibit their translation. The Epstein–Barr virus encodes its own microRNAs targeted at the genes responsible for the regulation of apoptosis [25]. Moreover, a viral infection may alter the expression profile of cellular microRNAs [26]. In particular, reducing the expression of cellular microRNAs (hsa-miR-200a and hsa-miR-200b) inhibits the expression of E-cadherin in gastric epithelial cells promoting epithelial–mesenchymal transition [26]. Gu et al. also believed that viral microRNAs as part of the exosomes are likely to play a significant role in modeling tumor microenvironment in EBV( +) GC [27].
Molecular portrait of EBV( +) GC
EBV-associated GC has its own definitive molecular features. TCGA analysis showed that 80% of EBV( +) gastric tumors have PIK3CA mutations, as well as amplifications of the JAK2, CD274 (PD-L1) and PDCD1LG2 (PD-L2) genes. Mutations of the ARID1A (55%) and BCOR (23%) genes are also common, while TP53 defects are not usual for this GC subtype [4] (Table 1).
PIK3CA mutations
As noted above, about 80% of cases of EBV GC are associated with mutations in PIK3CA gene, which encodes phosphatidyl inositol-3-kinase (PIK3) component. Phosphotidylinositol-3-kinases are enzyme family that is key component of PI3K/Akt/mTOR signaling pathway involved in many pro-oncogenic cellular processes such as apoptosis escape, cell growth, and proliferation. PIK3CA gene amplification promotes cell proliferation by activating the PI3K/Akt/mTOR pathway. Mutations of the PIK3CA gene were found in tumors of various sites such as colorectal, breast, ovarian, and endometrial cancer. Moreover, these mutations usually localize in hot spots: exon 9 (E542K and E545K) and exon 20 (H1047R) [28]. However, PIK3CA mutation frequency of EBV( +) GC in hot spots is only 28%, and they can be observed throughout the nucleotide sequence [4]. Hino et al. and Yuen et al. noted that the detection of genetic defects in PIK3CA might precede EBV infection, which then enhances activation of the PI3K/Akt/mTOR pathway. In infected cells, the viral protein LMP2A activates PI3K/Akt/mTOR pathway, so does EBV-mediated methylation of PTEN and INPP4B tumor suppressors, which normally inhibit this signaling pathway [23, 29].
Due to the activation of the PI3K/Akt/mTOR signaling pathway, an approach involving inhibition of mTOR transcriptional factor in patients with EBV-associated GC seemed promising. However, clinical studies on the use of mTOR inhibitors in patients with metastatic GC did not show any antitumor effect of this treatment option. Furthermore, we would like to point out that there was no dedicated analysis of the effectiveness of mTOR inhibitors in EBV-associated gastric tumors [30,31,32].
ARID1A mutations
The ARID1A gene (AT-rich interactive domain 1A) encodes the SWI/SNF chromatin remodeling complex component (SWItch/Sucrose Non-Fermentable) that regulates chromatin structure and gene expression. The protein product of ARID1A has a tumor suppressor activity. Mutations of this gene are found in gastric adenocarcinoma [33]. Missense and nonsense mutations are the most common, and they lead to significant reduction or cessation of protein synthesis [33].
An immunohistochemical study of 857 samples of gastric adenocarcinoma, 67 of which had EBV( +) phenotype, showed that loss of ARID1A expression was observed mainly in the case of EBV( +) (34%) and MLH1-negative GC (29%) [2]. Loss of ARID1A synthesis in EBV( +) phenotype did not correlate with the depth of tumor invasion. This fact points out that this mutation appears in the early stages of carcinogenesis, possibly even before invasion of cells with Epstein–Barr virus. The virus itself does not affect the expression level of ARID1A, while mutation of this gene might mediate the penetration of the virus into cell nucleus and methylation of target genes [34].
BCOR mutations
BCOR gene encodes a protein known as BCL6 corepressor. The corepressor BCL6 is a transcription factor that selectively binds to POZ (Pox virus and Zinc finger) domain of BCL6. This protein is essential to the formation of germinal centers of lymphoid follicles and apoptosis regulation. BCOR gene mutations are also associated with acute myeloblastic leukemia [35].
JAK2 amplification
Janus kinases (JAK) are protein family of non-receptor tyrosine kinases involved in signaling pathways of some cytokines. Activated Janus kinases phosphorylate a variety of cytoplasmic target proteins, including STAT transcription factors (signal transducers and activators of transcription) [36]. Phosphorylated STATs dimerize and enter the nucleus, inducing transcription of the genes necessary for cell proliferation and differentiation [37].
JAK2 is one of this family proteins, which mediates signaling of receptors of various cytokines (e.g., interferons α, β, γ, interleukins IL-6, IL-11, IL-22, etc.) and activates the STAT3 transcription factor [38]. It is widely known that JAK2 mutations are specific for myeloproliferative diseases. Overexpression of this protein due to the amplification of the JAK2 gene is one of molecular hallmarks of EBV( +) GC [1].
The activation of JAK2/STAT3 pathway in GC is supposed to be due to major pathogenicity factor Helicobacter pylori CagA (H. pylori-induced cytotoxin-associated antigen). H. pylori delivers CagA protein to mucocyte using type IV bacterial secretion. CagA protein, in its turn, induces release of various cytokines, such as IL-11 and IL-23, which bind to their receptors on target cells and activate the JAK2/STAT3 pathway. Phosphorylated STAT3 induces transcription of target genes mediating cell proliferation, migration/invasion, and angiogenesis: cyclin D1, matrix metalloproteinase-9, CD44v6, and VEGF [39, 40].
Phase II study, which evaluated the effectiveness of the BBI molecule—STAT3 inhibitor in comparison with placebo in patients with metastatic GC, failed to achieve its primary end-point of overall survival (OS) in the intention-to-treat population [41].
Hypermethylation
According to the TCGA analysis, EBV-associated gastric tumors are characterized by a high frequency of DNA hypermethylation. For instance, hypermethylation of the CDKN2A gene promoter (p16INK4A) was observed in all studied samples of EBV( +) gastric tumors.
This gene inhibits cyclin-dependent kinase 2A which encodes the p16 tumor suppressor involved in cell cycle regulation. The p16 protein inhibits cyclin-dependent kinases 4 and 6 (CDK4 and CDK6), so as another tumor suppressor Rb blocks the transition of the cell cycle from phase G1 to phase S. Inactivating somatic CDKN2A mutations are registered for a wide range of malignant tumors. Specifically, epigenetic inactivation of this gene is responsible for EBV( +) GC, as well as other tumor suppressors like p14, APC, and TFAP2E within CIMP phenotype (CpG island methylation phenotype) [42].
The CIMP phenotype is characterized by simultaneous methylation of multiple genes and plays an important role in the carcinogenesis of GI adenocarcinomas, especially EBV( +) GC and GC with MSI. Moreover, this process is non-causal, because both subtypes have specific differences in the profile of methylated genes. For instance, the MLH1 gene is methylated in MSI-subtype tumors, but is intact in EBV( +) adenocarcinomas [43].
It is important that CIMP status (high CIMP-H, low CIMP-L, and negative CIMP) correlates with the prognosis. Thus, patients with CIMP-H are more likely to have a relatively favorable prognosis, tumors that are more superficial, diffuse histological subtype, and an earlier stage of the disease than patients with CIMP-negative status [44].
CD274 (PD-L1)/PDCD1LG2 (PD-L2) amplification
CD274 and PDCD1LG2 genes encode immunosuppressive molecules PD-L1 and PD-L2 (programmed death ligands), respectively. PD-L1 and PD-L2 are transmembrane proteins that are expressed on the surface of antigen-presenting cells. PD-L1 and PD-L2 bind to the programmed death receptor PD-1 located on the T-lymphocyte membrane, and then, the T-lymphocyte loses its ability to destroy the tumor cell [45].
Some malignant tumors have high level of expression of PD-L1 and/or PD-L2, and that allows them to escape from antitumor immune response [46]. Among four molecular subtypes of GC, only EBV( +) GC has an increased expression of PD-L1 and/or PD-L2 [4, 47]. Increased expression of PD-L1 is also observed in other EBV-associated tumors [48, 49]. Patients with high expression of PD-L1 have a pronounced antitumor effect on treatment with monoclonal antibodies to PD-1 [50].
Methods of molecular diagnosis of Epstein–Barr virus in GC
Methods for Epstein–Barr virus detection include in situ hybridization (ISH), polymerase chain reaction (PCR), enzyme-linked immunosorbent assay (ELISA), and immunofluorescence analysis [51].
Studies of resected tumor tissue and biopsy material samples (for ISH and PCR) require blood samples (for PCR) and plasma samples of the patients (for ELISA). Possible diagnostic markers include viral small RNA EBER1 and EBER2 (for ISH); EBNA-1, Bam-M, BamHI-W viral antigens (for PCR); antibodies to viral antigens EBNA (nuclear antigen), VCA (capsid antigen), EA-D and EA-R (early antigens) (for ELISA) [51].
In situ hybridization of small virus RNA
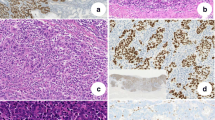
The gold standard for EBV status examination in GC is in situ hybridization of small RNAs localized in the nucleus of EBV-infected cells (EBER1 / EBER2) of tumor tissue samples (EBER-ISH). This is possible due to the small viral RNAs found in the nuclei of the tumor cells in large quantities (106–7 per cell), while underlying healthy epithelium of the stomach is usually negative for EBER-ISH [52].
According to a systematic analysis of 34 studies, the positive results of EBER-ISH were noted in 5–17.9% samples of tumor tissue [51]. In control groups (underlying healthy epithelium, biopsy material from healthy individuals, or patients with benign diseases of the stomach), the percentage of positive results was about zero [51].
To date, EBER-ISH is the most specific, albeit less sensitive, method for detecting EBV status in gastric adenocarcinomas. Disadvantages of this method include invasiveness and relative complexity of implementation [51].
Detection of viral nucleic acids in tumor tissues by PCR
The utility of PCR to diagnose EBV-associated GC remains controversial. Studies show that frequency of detection EBNA-1 and BamHI-W viral nucleic acid fragments in GC tissues with PCR is different, but generally higher than in the underlying healthy tissues [53,54,55,56]. High heterogeneity of the results does not allow for estimation of method’s reliability.
To date, no large-scale studies investigating the effectiveness of PCR diagnostics of EBV-associated GC have been conducted. EBV infection is usually diagnosed with non-polymorphic Epstein–Barr nuclear antigen1 (EBNA-1) gene-based PCR and confirmed by real-time PCR. In some studies, the prevalence of positive EBNA-1 PCR results reaches up to 80% [53, 57]. Compared with in situ hybridization (EBER-ISH), PCR is a more sensitive, but less specific method.
However, it is important to note that viral DNA amplified in PCR can come from the tumor-infiltrating lymphocytes, as well as the tumor cells themselves. The origin of viral genes cannot be established with PCR. This is a significant limitation of the PCR, since approximately 90% of the population carry latent EBV infection, so their lymphocytes contain viral genes [58].
High prevalence of viral DNA in tumor tissues found with PCR might indicate local inflammation and lymphocyte infiltration, but not the viral infection of the tumor cells. Thus, the examination of EBV status of gastric adenocarcinomas with PCR should be conducted with caution.
Serological examination
Serological diagnosis of EBV infection includes detection of immunoglobulins to viral antigens in the blood plasma: e.g., nuclear EBNA, capsid VCA, and early EA-D/EA-R antigens. Single studies have shown that according to enzyme immunoassay antibody, titer values vary significantly among patients with GC and healthy individuals [59,60,61,62].
Shinkura et al. found that antibodies to capsid antigen (VCA IgG) were detected more frequently among the GC patients than in controls, but these differences tend not to have statistical significance [62]. Although, they got rather conflicting data for other immunoglobulins. The study showed a statistically significant increase in seropositivity for VCA IgA and EA IgG immunoglobulins among patients with EBV( +) GC and not in patients with EBV(−) GC [62].
As in the case of PCR diagnostics of EBV( +) GC, clinicians should take into account the extremely low specificity of the serological examination. They should remember that serological markers of Epstein–Barr virus also indicate previous EBV infection or its reactivation. Due to high prevalence of latent EBV infection in the population, the interpretation of the results of serodiagnosis of EBV( +) GC is complex. Thus, antibodies to Epstein–Barr virus cannot be considered specific diagnostic markers, and their use for EBV status examination in GC remains doubtful.
Circulating viral DNA with real-time PCR
Detection of tumor-specific biomarkers in peripheral blood and other biological fluids is the basis of fluid biopsy. This method is an analysis of tumor cells nucleic acids that circulate freely in blood plasma (ctDNAs).
Given the monoclonal nature of cancer cell growth EBV( +) GC, viral genome can serve as reliable tumor biomarker. The possibility of using circulating DNA of Epstein–Barr virus as a marker of EBV( +) GC was shown as recently as in 2001 [63]. The authors revealed a correlation between EBV ctDNA and EBER-ISH status. Shoda et al. evaluated the clinical significance of EBV( +) GC fluid biopsy [64]. The sensitivity of the method was 71.4% (10/14) and the specificity was 97.1% (135/139). False-negative results (EBER-ISH + /EBV(−) ctDNA) were detected in patients whose adenocarcinoma sizes were less than 70 mm. They also found a significant correlation between the size of the tumor and the amount of EBV ctDNA. Consequently, lower sensitivity of the method is likely to be due to the insufficient amount for detection of virus ctDNA with real-time PCR because of small tumor sizes.
Unlike PCR analysis of viral DNA in tumor tissues or serological examination, liquid biopsy does not detect latent EBV infection, since the ctDNA comes from the tumor cells that died from necrosis or apoptosis. This fact explains the high specificity of the method.
An important clinical advantage of fluid biopsy is possibility of non-invasive monitoring of therapy effectiveness and tumor progression. After surgical treatment of EBV-associated GC, no viral DNA was detected in plasma of previously ctDNA-EBV( +) patients [64]. However, the effectiveness of liquid biopsy in the diagnosis and monitoring of EBV( +) GC should be confirmed in prospective studies involving a larger number of patients.
To conclude, the gold standard for detecting EBV in gastric carcinomas is in situ hybridization for EBER, whereas other methods have significant limitations preventing them from being used in clinical practice.
The predictive value of EBV-associated GC
Clinical significance of TCGA classification of GC is actively studied. Based on TCGA data, Sohn et al. developed a first prognostic model that establishes a statistically significant correlation between certain molecular subtypes of GC and patient survival rates, as well as the effectiveness of adjuvant chemotherapy [65]. They discovered that EBV( +) GC had the best prognosis for both relapse-free (RFS) (p = 0.006) and OS (p = 0.004). The worst prognosis was associated with a genetically stable subtype (GS). The other two subtypes (MSI and CIN) showed intermediate survival rates. In addition, they confirmed that EBV( +) GC is more common for men (79%) and younger age than other subtypes (average age 53, p = 0.01).
The greatest benefit from adjuvant chemotherapy was observed in the CIN GC subtype subgroup of patients showing a significant increase in RFS (RR 0.39; 95% CI 0.16–0.94; p = 0.03). In contrast, patients with GS GC had no statistically significant benefit from adjuvant chemotherapy (RR 0.83; 95% CI 0.36–1.89; p = 0.65). Sohn BH et al. failed to evaluate effectiveness of adjuvant chemotherapy in the EBV( +) GC due to the absence of control group. The authors also developed a unified model for relapse risk assessment after treatment (integrated risk assessment model, TRS), which served as a significant predictor of RFS (RR 1.5; 95% CI 1.2–1.9; p = 0.001) [65].
International analysis of 13 large multicenter studies that combined data from 4599 patients with gastric adenocarcinoma also showed that EBV( +) GC has a more favorable prognosis than EBV-negative tumors [66]. The majority of malignant tumors were diagnosed at advanced stages (52% of stage III-IV). Therewith, EBV-positive status showed decrease in the relative risk of death compared to VEB-negative tumors by 28% (RR 0.72; 95% CI 0.61–0.86) [66]. Median survival of patients with EBV( +) GC was 8.5 years, while patients with EBV(−) GC had 5.3 years (p = 0.0006).
Overall, EBV status is an important prognostic factor alongside TNM staging and histological grade. Despite the statistically significant correlation between EBV status and survival rates, all of the mentioned studies were retrospective. This fact did not allow us to assess predictive role of EBV infection in malignant gastric neoplasms. The effect of various chemotherapy regimens on treatment of EBV-associated metastatic GC remains unclear.
Immune checkpoint inhibitors in EBV-associated GC
Immunotherapy with inhibitors of the PD-1 receptor and its ligand (PD-L1), inhibitors of CTLA-4 made good progress in the treatment of different solid tumors, e.g., melanoma and lung cancer. PD-L1 overexpression in gastric tumor cells statistically significantly correlates with such adverse clinical parameters as large tumor size, distant metastases, and low survival rates [67]. Among all molecular subtypes of GC, immunotherapy is of the greatest clinical interest for EBV( +) GC due to increased expression of PD-L1.
The efficacy and safety of anti-PD-1 antibody pembrolizumab in the treatment of recurrent or metastatic PD-L1-positive gastric adenocarcinoma were studied in a phase I clinical trial KEYNOTE-012 [68]. The overall response rate was 22%, progression-free survival (PFS), and OS were 1.9 and 11.4 months, respectively. Pembrolizumab showed a generally acceptable profile of toxicity and promising antitumor activity. However, randomized phase 3 study KEYNOTE-061 did not show significant benefit of pembrolizumab over paclitaxel in the second-line therapy in patients with advanced gastric or gastroesophageal junction cancer. At the same time, subset analysis identified the following groups of patients that benefited more from pembrolizumab: patients with ECOG 0 (RR 0.69), patients with gastroesophageal junction cancer (RR 0.61), and patients with Combined Positive Score (CPS) ≥ 5 (RR 0.73) and ≥ 10 (RR 0.64). The Combined Positive Score is used to measure PD-L1 expression. It is the number of PD-L1 staining cells (tumor cells, lymphocytes, and macrophages) divided by the total number of viable tumor cells, multiplied by 100. The specimen should be considered to have PD-L1 expression if CPS ≥ 1. Patients with CPS < 1 had better response to paclitaxel (RR 1.20) [69].
Another phase 3 study KEYNOTE-062 showed that OS and PFS for the combination of pembrolizumab plus chemotherapy (cisplatin with fluoropyrimidine) in the first-line treatment are comparable to those for chemotherapy alone regardless of the CPS value [70]. Studies of anti-CTLA-4 and anti-PD-L1 antibodies in metastatic GC also failed [71, 72].
These contradictory results of the effect of immune checkpoint inhibitors in GC highlight the unmet need to search biomarkers of effectiveness of immunotherapy in GC. A recently published prospective phase II study was the first to show a very high response rate to pembrolizumab among patients with metastatic EBV( +) GC and MSI-GC (total response rate was 100 and 85.7%, respectively) [73]. Sixty-one patients were enrolled in this study. Thirty-two (52.5%) patients received pembrolizumab as second-line therapy, and 29 (47.5%) received pembrolizumab as third-line treatment for metastatic disease. Six (9.8%) patients were confirmed to be EBV( +) and seven (11.5%) had confirmed MSI-H gastric cancer. These data were available to the clinicians before study enrollment as MSI and EBV in situ testing is part of routine clinical practice at the institution where the trial was performed. All patients underwent pretreatment tissue biopsy with WES to infer TCGA subtype and mutational load, RNA sequencing to categorize patients according to molecular signatures previously evaluated in the context of gastric cancer, and EBV testing of the primary tumor with EBV DNA sequence profiling. The authors concluded that EBV( +) status and MSI-H could serve as additional reliable predictors of response to immunotherapy, as well as high expression of PD-L1 in the tumor detected with IHC. They proposed to bring routine EBV status examination into clinical practice to identify patients with gastric adenocarcinomas who could benefit from immunotherapy [73].
The ongoing clinical trials of immune checkpoint inhibitors in EBV-associated GC were listed in Table 2.
Conclusion
EBV-associated GC is an independent subtype of GI tumors. In addition to the special clinical and pathological phenotype, it also has the best prognosis among all five GI adenocarcinomas molecular subtypes. EBV( +) gastric adenocarcinomas have the highest immunogenicity among all GI tumors. These characteristics as well as disappointing results of immunotherapy in GC point out that EBV( +) GC could be an applicable candidate for further immunotherapy investigation in GC. Furthermore, identification of other molecular characteristics of EBV( +) GC could reveal new potential therapeutic targets for the personalized treatment of this pathology.
References
Naseem M, Barzi A1, Brezden-Masley C, Puccini A, Berger MD, Tokunaga R, et al. Outlooks on Epstein-Barr virus associated gastric cancer. Cancer Treat Rev. 2018;66:15–22.
Akiba S, Koriyama C, Herrera-Goepfert R, Eizuru Y. Epstein-Barr virus associated gastric carcinoma: epidemiological and clinicopathological features. Cancer Sci. 2008;99:195–201. https://doi.org/10.1111/j.1349-7006.2007.00674.x.
Hinoue T, Bass AJ, Laird PW. Comparative molecular analysis of gastrointestinal comparative molecular analysis of gastrointestinal adenocarcinomas. Cancer Cell. 2018;33(4):721–735.e8. https://doi.org/10.1016/j.ccell.2018.03.010.
Bass A, Thorsson V, Shmulevich I, et al. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–9. https://doi.org/10.1038/nature13480.
Lee JH, Kim SH, Han SH, An JS, Lee ES, Kim YS. Clinicopathological and molecular characteristics of Epstein-Barr virus-associated gastric carcinoma: a meta-analysis. J Gastroenterol Hepatol. 2009;24:354–65.
Fukayama M. Epstein-Barr virus and gastric carcinoma. Pathol Int. 2010;60:337–50. https://doi.org/10.1111/j.1440-1827.2010.02533.x.
Yanai H, Nishikawa J, Mizugaki Y, Shimizu N, Takada K, Matsusaki K, Toda T, Matsumoto Y, Tada M, Okita K. Endoscopic and pathologic features of Epstein-Barr virus-associated gastric carcinoma. Gastrointest Endosc. 1997;45:236–42. https://doi.org/10.1016/S0016-5107(97)70265-7].
Nishikawa J, Yanai H, Mizugaki Y, Takada K, Tada M, Okita K. Case report: hypoechoic submucosal nodules: a sign of Epstein-Barr virus-associated early gastric cancer. J Gastroenterol Hepatol. 1998;13:585–90. https://doi.org/10.1111/j.1440-1746.1998.tb00694.x.
Park JH, Kim EK, Kim YH, et al. Epstein-Bar virus positivity, not mismatch repair-deficiency, is a favorable risk factor for lymph node metastasis in submucosa-invasive early gastric cancer. Gastric Cancer. 2016;19:1041–51.
Lee JY, Kim KM, Min BH, Lee JH, Rhee PL, Kim JJ. Epstein-Barr virus-associated lymphoepithelioma-like early gastric carcinomas and endoscopic submucosal dissection: case series. World J Gastroenterol. 2014;20:1365–70.
Yanai H, Chihara D, Harano M, Sakaguchi E, Murakami T, Nishikawa J. Epstein-Barr Virus-associated early gastric cancer treated with endoscopic submucosal dissection: a possible candidate for extended criteria of endoscopic submucosal dissection. Intern Med. 2019;58(22):3247–50. https://doi.org/10.2169/internalmedicine.3055-19.
Koh J, Ock CY, Kim JW, Nam SK, Kwak Y, Yun S, Ahn SH, Park DJ, Kim HH, Kim WH, Lee HS. Clinicopathologic implications of immune classification by PD-L1 expression and CD8-positive tumor-infiltrating lymphocytes in stage II and III gastric cancer patients. Oncotarget. 2017;8(16):26356–67. https://doi.org/10.18632/oncotarget.15465.
Derks S, Liao X, Chiaravalli AM, Xu X, Camargo MC, Solcia E, Sessa F, Fleitas T, Freeman GJ, Rodig SJ, Rabkin CS, Bass AJ. Abundant PD-L1 expression in Epstein-Barr virus-infected gastric cancers. Oncotarget. 2016;7(22):32925–322. https://doi.org/10.18632/oncotarget.9076.
Spear PG, Longnecker R. Herpesvirus entry: an update. J Virol. 2003;77(19):10179–85. https://doi.org/10.1128/jvi.77.19.10179-10185.2003.
Chesnokova LS, Hutt-Fletcher LM. Epstein-Barr virus infection mechanisms. Chin J Cancer. 2014;33(11):545–8. https://doi.org/10.5732/cjc.014.10168(Epub 2014 Oct 17).
Matsusaka K, Kaneda A, Nagae G, Ushiku T, Kikuchi Y, Hino R, Uozaki H, Seto Y, Takada K, Aburatani H, Fukayama M. Classification of Epstein-Barr virus-positive gastric cancers by definition of DNA methylation epigenotypes. Cancer Res. 2011;71:7187–97.
Fukayama M, Hayashi Y, Iwasaki Y, Chong J, Ooba T, Takizawa T, Koike M, Mizutani S, Miyaki M, Hirai K. Epstein-Barr virus-associated gastric carcinoma and Epstein-Barr virus infection of the stomach. Lab Invest. 1994;71:73–81.
Frappier L. Contributions of Epstein-Barr nuclear antigen 1 (EBNA1) to cell immortalization and survival. Viruses. 2012;4(9):1537–47. https://doi.org/10.3390/v4091537(Epub 2012 Sep 13).
Chen C, Li D, Guo N. Regulation of cellular and viral protein expression by the Epstein-Barr virus transcriptional regulator Zta: implications for therapy of EBV associated tumors. Cancer Biol Ther. 2009;8(11):987–95. https://doi.org/10.4161/cbt.8.11.8369.
Kang GH, Lee S, Kim WH, Lee HW, Kim JC, Rhyu M, et al. Demonstrates frequent aberrant methylation of multiple genes and constitutes CpG island methylator phenotype-positive gastric carcinoma. Am J Pathol. 2002;160(3):787–94.
Matsusaka K, Funata S, Fukuyo M, Seto Y, Aburatani H, Fukayama M, Kaneda A. Epstein-Barr virus infection induces genome-wide de novo DNA methylation in non-neoplastic gastric epithelial cells. J Pathol. 2017;242:391–9. https://doi.org/10.1002/path.4909.
Fernandez AF, Rosales C, Lopez-Nieva P, Graña O, Ballestar E, Ropero S, et al. The dynamic DNA methylomes of double-stranded DNA viruses associated with human cancer. Genome Res. 2009;19(3):438–51. https://doi.org/10.1101/gr.083550.108(Epub 2009 Feb 10).
Hino R, Uozaki H, Murakami N, Ushiku T, Shinozaki A, Ishikawa S, et al. Activation of DNA methyltransferase 1 by EBV latent membrane protein 2A leads to promoter hypermethylation of PTEN gene in gastric carcinoma. Cancer Res. 2009;69(7):2766–74. https://doi.org/10.1158/0008-5472.CAN-08-3070.
Shinozaki-Ushiku A, Kunita A, Fukayama M. Update on Epstein-Barr virus and gastric cancer (review). Int J Oncol. 2015;46(4):1421–34.
Shinozaki-Ushiku A, Kunita A, Isogai M, Hibiya T, Ushiku T, Takada K, Fukayama M. Profiling of virus-encoded microRNAs in Epstein-Barr virus-associated gastric carcinoma and their roles in gastric carcinogenesis. J Virol. 2015;89(10):5581–91. https://doi.org/10.1128/JVI.03639-14(Epub 2015 Mar 4).
Shinozaki A, Sakatani T, Ushiku T, Hino R, Isogai M, Ishikawa S, Uozaki H, Takada K, Fukayama M. Downregulation of microRNA-200 in EBV-associated gastric carcinoma. Cancer Res. 2010;70:4719–27.
Gu J, Qian H, Shen L, Zhang X, Zhu W, Huang L, et al. Gastric cancer exosomes trigger differentiation of umbilical cord derived mesenchymal stem cells to carcinoma-associated fibroblasts through TGF-β/Smad pathway. PLoS ONE. 2012;7(12):e52465. https://doi.org/10.1371/journal.pone.0052465.
Samuels Y, Waldman T. Oncogenic mutations of PIK3CA in human cancers. Curr Top Microbiol Immunol. 2010;347:21–41. https://doi.org/10.1007/82_2010_68.
Yuen JW, Chung GT, Lun SW, Cheung CC, To KF, Lo KW. Epigenetic inactivation of inositol polyphosphate 4-phosphatase B (INPP4B), a regulator of PI3K/AKT signaling pathway in EBV-associated nasopharyngeal carcinoma. PLoS ONE. 2014;9(8):e105163. https://doi.org/10.1371/journal.pone.0105163.
Ohtsu A, Ajani JA, Bai YX, Bang YJ, Chung HC, Pan HM, et al. Everolimus for previously treated advanced gastric cancer: results of the randomized, double-blind, phase III GRANITE-1 study. J Clin Oncol. 2013;31(31):3935–43. https://doi.org/10.1200/JCO.2012.48.3552(Epub 2013 Sep 16).
Al-Batran SE, Riera-Knorrenschild J, Pauligk C, Goetze TO, Hegewisch-Becker S, Seraphin J, et al. A randomized, double-blind, multicenter phase III study evaluating paclitaxel with and without RAD001 in patients with gastric cancer who have progressed after therapy with a fluoropyrimidine/platinum-containing regimen (RADPAC). J Clin Oncol. 2017;35(4_suppl):4–4.
Ramanathan RK, McDonough SL, Kennecke HF, Iqbal S, Baranda JC, Seery TE, et al. Phase 2 study of MK-2206, an allosteric inhibitor of AKT, as second-line therapy for advanced gastric and gastroesophageal junction cancer: a SWOG cooperative group trial (S1005). Cancer. 2015;121(13):2193–7. https://doi.org/10.1002/cncr.29363(Epub 2015 Mar 30).
Wang K, Law S, Wang K, Kan J, Yuen ST, Shi ST, et al. Exome sequencing identifies frequent mutation of ARID1A in molecular subtypes of gastric cancer Exome sequencing identifies frequent mutation of ARID1A in molecular subtypes of gastric cancer. Nat Genet. 2011;43(12):1219–23.
Day L, Chau CM, Nebozhyn M, Rennekamp AJ, Showe M, Lieberman PM. Chromatin profiling of Epstein-Barr virus latency control region. J Virol. 2007;81(12):6389–401. https://doi.org/10.1128/JVI.02172-06(Epub 2007 Apr 4).
Grossmann V, Tiacci E, Holmes AB, Kohlmann A, Martelli MP, Kern W, et al. Whole-exome sequencing identifies somatic mutations of BCOR in acute myeloid leukemia with normal karyotype. Blood. 2011;118(23):6153–63. https://doi.org/10.1182/blood-2011-07-365320(Epub 2011 Oct 19).
Darnell JE, Kerr IM, Stark GR. Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science. 1994;264(5164):1415–21.
Kortylewski M, Yu H. Role of Stat3 in suppressing anti-tumor immunity. Curr Opin Immunol. 2008;20(2):228–33. https://doi.org/10.1016/j.coi.2008.03.010(Epub 2008 May 12).
Yu H, Lee H, Herrmann A, Buettner R, Jove R. Revisiting STAT3 signalling in cancer: new and unexpected biological functions. Nat Rev Cancer. 2014;14(11):736–46. https://doi.org/10.1038/nrc3818.
Jackson CB, Giraud AS, Bp S, Kh W, Jackson CB, Giraud AS. STAT3 as a prognostic marker in human gastric cancer. J Gastroenterol Hepatol. 2009;24(4):646–51. https://doi.org/10.1111/j.1440-1746.2008.05671.x(Epub 2008 Nov 3).
Han J, Zhang K, Chen X, Jiang H, Kong Q. Expression of seven gastric cancer-associated genes and its relevance for Wnt, NF-k B and Stat3 signaling. APMIS. 2007;115(12):1331–433. https://doi.org/10.1111/j.1600-0643.2007.00695.x.
Sonbol MB, Bekaii-Saab T. A clinical trial protocol paper discussing the BRIGHTER study. Future Oncol. 2018;14:901–6.
Geddert H, Zur Hausen A, Gabbert HE, Sarbia M. EBV-infection in cardiac and non-cardiac gastric adenocarcinomas is associated with promoter methylation of p16, p14 and APC, but not hMLH1. Anal Cell Pathol (Amst). 2010;33(3):143–9. https://doi.org/10.3233/ACP-CLO-2010-0540.
Chang M, Uozaki H, Chong J, Ushiku T, Sakuma K, Ishikawa S, et al. Human cancer biology CpG island methylation status in gastric carcinoma with and without infection of Epstein-Barr virus. Clin Cancer Res. 2006;12(10):2995–3002.
dos Jácome AAA, de Lima EM, Kazzi AI, Chaves GF, de Mendonça DC, Maciel MM, de Santos JS. Epstein-Barr virus-positive gastric cancer: a distinct molecular subtype of the disease? Rev Soc Bras Med Trop. 2016;49(2):150–7. https://doi.org/10.1590/0037-8682-0270-2015.
Li Y, Liang Z, Tian Y, Cai W, Weng Z, Chen L, Zhang H, Bao Y, Zheng H, Zeng S, Bei C, Li Y, et al. High-affinity PD-1 molecules deliver improved interaction with PD-L1 and PD-L2. Cancer Sci. 2018;109(8):2435–45.
Dong H, Strome S, Salomao D, et al. Tumor-associated B7–H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med. 2002;8:793–800. https://doi.org/10.1038/nm730.
Pereira MA, Ramos MF, Faraj SF, et al. Clinicopathological and prognostic features of Epstein-Barr virus infection, microsatellite instability, and PD-L1 expression in gastric cancer. J Surg Oncol. 2018;117:829–39. https://doi.org/10.1002/jso.25022.
Chen BJ, Chapuy B, Ouyang J, Sun HH, Roemer MG, Xu ML, Yu H, Fletcher CD, Freeman GJ, Shipp MA, Rodig SJ. PD-L1 expression is characteristic of a subset of aggressive B-cell lymphomas and virus-associated malignancies. Clin Cancer Res. 2013;19(13):3462–73. https://doi.org/10.1158/1078-0432.CCR-13-0855(Epub 2013 May 14).
Green MR, Rodig S, Juszczynski P, Ouyang J, Sinha P, O'Donnell E, et al. Constitutive AP-1 activity and EBV infection induce PD-L1 in Hodgkin lymphomas and posttransplant lymphoproliferative disorders: implications for targeted therapy. Clin Cancer Res. 2012;18(6):1611–8. https://doi.org/10.1158/1078-0432(CCR-11-1942. Epub 2012 Jan 23. Erratum in: Clin Cancer Res. 2012 Apr 1;18(7):2117).
Ohaegbulam KC, Assal A, Lazar-Molnar E, Yao Y, Zang X. Human cancer immunotherapy with antibodies to the PD-1 and PD-L1 pathway. Trends Mol Med. 2015;21(1):24–33. https://doi.org/10.1016/j.molmed.2014.10.009(Epub 2014 Oct 30).
Chen XZ, Chen H, Castro FA, Hu JK, Brenner H. Epstein-Barr virus infection and gastric cancer: a systematic review. Medicine (Baltimore). 2015;94(20):e792. https://doi.org/10.1097/MD.0000000000000792.
Tokunaga M, Land CE, Uemura Y, Tokudome T, Tanaka S, Sato E. Epstein-Barr virus in gastric carcinoma. Am J Pathol. 1993;143:1250–4.
Shukla SK, Prasad KN, Tripathi A, Singh A, Saxena A, Ghoshal UC, Krishnani N, Husain N. Epstein-Barr virus DNA load and its association with Helicobacter pylori infection in gastroduodenal diseases. Braz J Infect Dis. 2011;15(6):583–90.
Martínez-López JL, Torres J, Camorlinga-Ponce M, Mantilla A, Leal YA, Fuentes-Pananá EM. Evidence of Epstein-Barr virus association with gastric cancer and non-atrophic gastritis. Viruses. 2014;6(1):301–18. https://doi.org/10.3390/v6010301.
Lee MA, Hong YS, Kang JH, Lee KS, You JY, Lee KY, Park CH. Detection of Epstein-Barr virus by PCR and expression of LMP1, p53, CD44 in gastric cancer. Korean J Intern Med. 2004;19(1):43–7. https://doi.org/10.3904/kjim.2004.19.1.43.
Oda K, Koda K. Original article Detection of Epstein-Barr virus in gastric carcinoma cells and surrounding lymphocytes. Gastric Cancer. 2003;6(3):173–8.
Shukla S, Prasad K, Tripathi A, Ghoshal U, Krishnani N, Husain N. Expression profile of latent and lytic transcripts of epstein–barr virus in patients with gastroduodenal diseases: a study from northern India. J Med Virol. 2012;84(8):1289–97. https://doi.org/10.1002/jmv.23322.
Rowlands DC, Ito M, Mangham DC, Reynolds G, Herbst H, Hallissey MT, et al. Epstein-Barr virus and carcinomas: rare association of the virus with gastric adenocarcinomas. Br J Cancer. 2016;114(12):e15. https://doi.org/10.1038/bjc.2016.156.
Kim Y, Shin A, Gwack J, Ko KP, Kim CS, Park SK, Hong YC, Kang D, Yoo KY. Epstein-Barr virus antibody level and gastric cancer risk in Korea: a nested case-control study. Br J Cancer. 2009;101(3):526–9. https://doi.org/10.1038/sj.bjc.6605146(Epub 2009 Jun 23).
Koshiol J, Qiao Y, Kamangar F. Epstein-Barr virus serology and gastric cancer incidence and survival. Br J Cancer. 2007;97(11):1567–9 (Epub 2007 Nov 6).
Levine PH, Lennelte ET, Hildesheim A, Shibata D, Nomura A. Elevated antibody titers to Epstein-Barr virus prior to the diagnosis of Epstein-Barr-virus-associated gastric adenocarcinoma. Int J Cancer. 1995;60(5):642–4.
Shinkura R, Yamamoto N, Koriyama C, Shinmura Y, Eizuru Y, Tokunaga M. Epstein-Barr virus-specific antibodies in Epstein-Barr virus-positive and-negative gastric carcinoma cases in Japan. J Med Virol. 2000;60(4):411–6.
Lo YMD, Chan WY, Ng EKW, Chan LYS, Lai PBS, Tam JS, et al. Circulating Epstein-Barr virus DNA in the serum of patients with gastric carcinoma. Clin Cancer Res. 2001;7(7):1856–9.
Shoda K, Ichikawa D, Fujita Y, Masuda K, Hiramoto H, Hamada J, Arita T, Konishi H, Kosuga T, Komatsu S, Shiozaki A, Okamoto K, Imoto I, Otsuji E. Clinical utility of circulating cell-free Epstein-Barr virus DNA in patients with gastric cancer. Oncotarget. 2017;8(17):28796–804. https://doi.org/10.18632/oncotarget.15675.
Sohn BH, Hwang JE, Jang HJ, Lee HS, Oh SC, Shim JJ, et al. Clinical significance of four molecular subtypes of gastric cancer identified by the cancer genome atlas project. Clin Cancer Res. 2017. https://doi.org/10.1158/1078-0432.CCR-16-2211(Epub ahead of print).
Camargo MC, Kim WH, Chiaravalli AM, Kim KM, Corvalan AH, Matsuo K, et al. Improved survival of gastric cancer with tumour Epstein-Barr virus positivity: an international pooled analysis. Gut. 2014;63(2):236–43. https://doi.org/10.1136/gutjnl-2013-304531(Epub 2013 Apr 12).
Qing Y, Li Q, Ren T, Xia W, Peng Y, Liu GL, et al. Upregulation of PD-L1 and APE1 is associated with tumorigenesis and poor prognosis of gastric cancer. Drug Des Devel Ther. 2015;16(9):901–9. https://doi.org/10.2147/DDDT.S75152.
Muro K, Bang Y-J, Shankaran V, Geva R, Catenacci DVT, Gupta S, et al. Relationship between PD-L1 expression and clinical outcomes in patients (Pts) with advanced gastric cancer treated with the anti-PD-1 monoclonal antibody pembrolizumab (Pembro; MK-3475) in KEYNOTE-012. J Clin Oncol. 2015;33(3_suppl):3.
Shitara K, Özgüroğlu M, Bang YJ, Di Bartolomeo M, Mandalà M, Ryu MH, et al. Pembrolizumab versus paclitaxel for previously treated, advanced gastric or gastro-oesophageal junction cancer (KEYNOTE-061): a randomised, open-label, controlled, phase 3 trial. Lancet. 2018;392(10142):123–33.
Tabernero J, Van Cutsem E, Bang Y.-J, Fuchs CS, Wyrwicz L, Lee KW, Kudaba I, Garrido M, Chung HC, Salguero HRC, et al. Pembrolizumab with or without chemotherapy versus chemotherapy for advanced gastric or gastroesophageal junction (G/GEJ) adenocarcinoma: The phase III KEYNOTE-062 study. J Clin Oncol 2019:37(18). https://doi.org/10.1200/JCO.2019.37.18_suppl.LBA4007.
Bang YJ, Cho JY, Kim YH, et al. Efficacy of sequential ipilimumab monotherapy versus best supportive care for unresectable locally advanced/metastatic gastric or gastroesophageal junction cancer. Clin Cancer Res. 2017;23(19):5671–8. https://doi.org/10.1158/1078-0432.CCR-17-0025(Epub 2017 Jun 27).
Bang YJ, Ruiz EY2, Van Cutsem E. Phase III, randomised trial of avelumab versus physician's choice of chemotherapy as third-line treatment of patients with advanced gastric or gastro-oesophageal junction cancer: primary analysis of JAVELIN Gastric 300. Ann Oncol. 2018;29(10):2052–60.
Kim ST, Cristescu R, Bass AJ, Kim K, Odegaard JI, Kim K, et al. Comprehensive molecular characterization of clinical responses to PD-1 inhibition in metastatic gastric cancer. Nat Med. 2018;24(9):1449–588. https://doi.org/10.1038/s41591-018-0101-z(Epub 2018 Jul 16).
Funding
The authors declare that they have no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ignatova, E., Seriak, D., Fedyanin, M. et al. Epstein–Barr virus-associated gastric cancer: disease that requires special approach. Gastric Cancer 23, 951–960 (2020). https://doi.org/10.1007/s10120-020-01095-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-020-01095-z