Abstract
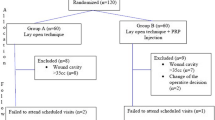
The aim of this study was to evaluate the effects of application of platelet-rich plasma in addition to laser pilonidoplasty for the treatment of pilonidal sinus. Twenty-five patients who were treated by laser pilonidoplasty for pilonidal sinus (group 1) and 25 patients who were treated by platelet-rich plasma in addition to laser pilonidoplasty (group 2) at this clinic were included in the study. Patients were classified according to the Irkorucu and Adana Numune’s classification and treatment concept. Duration of stay of the patients in the hospital, time to start daily activities, duration of wound healing, recurrence, and complications were evaluated. Among the 50 patients included in the study, 41 (%82) were males and 9 (%18) were females. The mean age was 25.6 ± 2.4 years and 24.8 ± 3.8 years in groups 1 and 2, respectively. The locations of the pilonidal sinus were similar in the two groups. No statistically significant differences were found in the duration of hospital stay, duration of the procedure, time to return to work, and complication rates between the two groups. Nevertheless, duration of wound healing was 6.1 ± 2.3 and 4.1 ± 0.9 weeks in groups 1 and 2, respectively, and was shorter in group 2. Duration of wound healing was statistically significantly different in the two groups. We concluded in this study that application of platelet-rich plasma in addition to laser pilonidoplasty significantly shortens the time of wound healing.



Similar content being viewed by others
References
Badawy EA, Kanawati (2009) Effect of hair removal by Nd:YAG laser on the recurrence of pilonidal sinus. J Eur Acad Dermatol Venerol 23(8):883–866
Hodges RM (1880) Pilo-nidal sinus. Boston Med Surg J 103:485–486
Poulsen IM, Bisgaard T (2008) Treatment of pilonidal cysts. Ugeskr Laeger 170:2963–2968
Humphries AE, Duncan JE (2010) Evaluation and management of pilonidal diasease. Surg Clin 90:113–124
Loganathan A, Zadeh RA, Hartley J (2012) Pilonidal disease: time to reevaluate a common pain in the rear. Dis Colon Rectum 55:491–493
Kabiri A, Esfandaiari E, Esmaeili A, Hshemibeni B, Pourazar A, Mardani M (2014) Platelet-rich plasma application in chondrogenesis. Adv Biomed Res 3:138
Efron J (2009) Role of platelet-rich plasma in accelerating the wound-healing process and recovery in patients undergoing operation for pilonidal sinus disease: preliminary results. World J Surg 33:1770–1771
Martinez-Zapata MJ, Marti-Carvajal A, Sola I et al (2009) Efficacy and safety of the use of autologous plasma rich in platelets for tissue regeneration : a systematic review. Transfusion 49:44–56
Mostafaei S, Norooznezhad F, Mohammadi S, Norooznezhad AH (2017) Effectiveness of platelet-rich plasma therapy in wound healing of pilonidal sinus surgery: a comprehensive systematic review and meta-analysis. Wound Repair Regen. https://doi.org/10.1111/wrr.12597
Georgiou GK (2016) Outpatient treatment of pilonidal disease with a 1470 nm diode laser; initial experience. Int J Surg Surgical Porced 1:103. https://doi.org/10.15344/ijssp/2016/103
Patil AM (2019) Pilonidal sinus destruction with a laser probe: technique. J Evid Based Med Healthc 6(7):468–470. https://doi.org/10.18410/jebmh/2019/98
Albahadili MA, Majeed AW (2016) Pilonidal sinus management using 980 nm diode laser. J Health Med Nurs 33(33):106–111
Dessily M, Charara F, Ralea S, Allé JL (2017) Pilonidal sinus destruction with a radial laser probe: technique and first Belgian experience. Acta Chir Belg 117:164–168
Porwal A, Gandhi P, Kulkarni D (2020) Laser pilonidotomy-a new approach in management of complex pilonidal sinus disease: an exploratory study. J Coloproctol (Rio J) 40(1):24–30
Pappas AF, Christodoulou DK (2018) A new minimally invasive treatment of pilonidal sinus disease with the use of diode laser: a prospective large series of patients. Color Dis 20(8):0207–0214. https://doi.org/10.1111/codi.14285
Oram Y, Kahraman F, Karıncaoğlu Y, Koyuncu (2010) Evaluation of patients with pilonidal sinus treated with laser epilation after surgery. Surg 36(1):88–91
Irkörücü O, Erdem H, Reyhan E (2012) Th e best therapy for pilonidal disease: which management for which type? World J Surg 36:691–692
McCallum IJ, King PM, Bruce J (2008) Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ 336:868–871
Da Silva JH (2000) Pilonidal cyst: cause and treatment. Dis Colon Rectum 43(8):1146-1156
Khan A (2006) Prognostic factors of pilonidal sinus. J Med Sci 14:40–43
Priyadarshi S, Dogra BB, Nagare K, Rana KV, Sunkara R, Kandari A (2014) A comparative study of open technique and Z-plasty in management of pilonidal sinus. Med J DY PatilUniv 7:574–578
Kement M, Oncel M, Kurt N, Kaptanoglu L (2006) Sinus excision for the treatment of limited chronic pilonidal disease: results after a medium-term follow-up. Dis Colon Rectum 49:1758–1762
Lindholt-Jensen CS, Lindholt JS, Beyer M et al (2012) Nd –YAG laser treatment of primary and recurrent pilonidal sinus. Lasers Med Sci 27:505–508
Spyridakis M, Christodoulidis G, Chatzitheofilou C (2009) Role of platelet-rich plasma in accelerating the wound-healing process and recovery in patients undergoing operation for pilonidal sinus disease: preliminary results. World J Surg. https://doi.org/10.1007/s00268-009-0046-y
Albahadili MA, Majeed AW (2016) Pilonidal sinus management using 980 nm diode laser. J Health Med Nurs 33:106–111
L’ Esperance FA (1989) chapter 1. In: Ophthalmic lasers, Third edn. Churchill Livingston, Edinburgh, pp 1–10
Soliman M, Kharbotly AEL, Saafan A (2005) Management of oral lichen planus using diode laser (980nm). A clinical study. Egyptian Dermatol Online J 1(1):3
Grabowski J, Oyetunji TA, Goldin AB, Baird R, Gosain A, Lal DR et al (2019) The management of pilonidal disease: a systematic review. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2019.02.055
Porwal A, Gandhi P, Kulkarni D (2020) Laser pilonidotomy-a new approach in management of complex pilonidal sinus disease: an exploratory study. J Coloproctol (Rio J) 40(1):24–30
Alferink M, Atmowihardjo L, Smeenk R, Cadanova D, Schouten R (2019) Pilonidal disease laser therapy: short term results of an observational cohort study. World J Surg Surgical Res 2:1143
Sadick NS, Yee-Levin (2006) Laser and light treatments for pilonidal cysts. Cutis. 78:125–128
Solomon MP (1998) Hair removal using the long-pulsed ruby laser. Ann Plast Surg 41:1–6
Conroy FJ, Kandamanay N, Mahaffey PJ (2008) Laser depilation and hygiene: preventing recurrent pilonidal sinus disease. J Plast Reconstr Aesthet Surg 61:1069–1072
Stauffer VK et al (2018) Common surgical procedures in pilonidal sinus disease: a metaanalysis, merged data analysis, and comprehensive study on recurrence. Sci Rep 8:3058
Odili J, Gault D (2002) Laser depilation of the natal cleft an aid to healing the pilonidal sinus. Ann R Coll Surg Engl 6:84(1):29–32
İesalnieks İ, Ommer A (2019) The management of pilonidal sinus. Dtsch Arztebl Int 6:116(1–2):12–21
Conroy FJ, Kandamany N, Mahaffey PJ (2008) Laser depilation and hygiene: preventing recurrent pilonidal sinus disease. J Plast Reconstruct Aesthetic Surg 61(9):1069–1072
Kabiri A, Esfandiari E, Esmaeili A, Hashemibeni B, Pourazar A, Mardani M (2014) Platelet-rich plasma application in chondrogenesis. Adv Biomed Res 3:138
Sakata J, Sasaki S, Handa K, Uchino T, Sasaki T, Higashita RA (2012) Retrospective, longitudinal study to evaluate healing lower extremity wounds in patients with diabetes mellitus and ischemia using standard protocols of care and platelet –rich plasma gel in a Japanese wound care program. Ostomy/Wound Manag 58:36–49
Casati L, Celotti F, Negri-Cesi P, Sacchi MC, Castano P, Colciago A (2014) Platelet derived growth factor (PDGF) contained in platelet rich plasma(PRP) stimulates migration os osteoblasts by reorganizing actin cytoskeleton. Cell Adhes Migr 8:595–602
Lacci KM, Dardik A (2010) Platelet-rich plasma: support for its use in wound healing. Yale J Biol Med 83:1–9
Norooznezhad AH, Norooznez F, Ahmadi K (2014) Next target of tranilast: inhibition of corneal neovascularization. Med Hypotheses 82:700–702
Karahan Ö, Sevinç B, Şimşek G, Demirgül R (2016) Minimally invasive treatment of pilonidal sinus disease using platelet-rich plasma. Trans Surg 1:14–17
Mohammadi S, Nasiri S, Mohammadi MH et al (2017) Evaluation of platelet –rich plasma gel potential in acceleration of wound healing duration in patients underwent pilonidal sinus surgery: a randomized controlled parallel clinical trial. Transfus Apher Sci 56(2):226–232
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical board approval
The necessary ethics approval for all applications used in this study was obtained from the Ethics Committee of the Adana City Education and Research Hospital. The patients were informed of the PRP and laser pilonidoplasty procedures and consents were obtained prior to the procedure.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kurt, F., Sözen, S., Kanat, B.H. et al. Effect of platelet-rich plasma on healing in laser pilonidoplasty for pilonidal sinus disease. Lasers Med Sci 36, 1015–1021 (2021). https://doi.org/10.1007/s10103-020-03137-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03137-5