Abstract
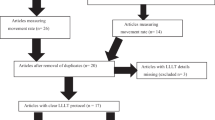
Low-level laser therapy is claimed to accelerate bone remodeling. The aim of this meta-analysis was to critically appraise current evidence and to determine the effectiveness of low-level laser therapy in accelerating orthodontic tooth movement. PubMed, Web of Knowledge, Embase, CENTRAL, ProQuest Dissertations &Theses, and SIGLE were electronically searched from Jan 1990 to Jun 2013. Article screening, data extraction, assessment of risk of bias and evaluation of evidence quality through GRADE were conducted independently and in duplicate by two reviewer authors. Outcome of interest in this meta-analysis was accumulative moved distance (AMD). Meta-analyses were performed in Comprehensive Meta-Analysis Version 2.2.064 (Biostat, Englewood, NJ, USA). Finally, five studies were included in this meta-analysis. The meta-analysis revealed that the pooled difference in mean (DM) was 0.33 [95 % CI: (0.03–0.64)], 0.76 [95 % CI: (−0.14, 1.65)] and 0.43 [95 % CI: (−0.05, 0.91)] for AMD within 1 month, AMD within 2 months and AMD within 3 months, respectively. However, significant heterogeneities and instability of the pooled results were detected. Moreover, publication bias was found for AMD within 3 months. The subgroup analysis on the wavelength of 780 nm revealed that the pooled DM of AMD were 0.54 (95 % CI = 0.18–0.91), 1.11 (95 % CI = 0.91–1.31) and 1.25 (95 % CI = 0.68–1.82) for 1, 2, and 3 months, respectively. For the output power of 20 mW, the subgroup analysis showed that the pooled DM of AMD was 0.45 (95 % CI = 0.26–0.64), 1.11 (95 % CI = 0.91–1.31), and 1.25 (95 % CI = 0.68–1.82) for 1, 2, and 3 months, respectively. Weak evidence suggests that low-level laser irradiations at the wavelength of 780 nm, at the fluence of 5 J/cm2 and/or the output power of 20 mW could accelerate orthodontic tooth movement within 2 months and 3 months. However, we cannot determine its effectiveness within 1 month due to potential measurement errors.





Similar content being viewed by others
References
Fisher MA, Wenger RM, Hans MG (2010) Pretreatment characteristics associated with orthodontic treatment duration. Am J Orthod Dentofac Orthop 137:178–186
Fink DF, Smith RJ (1992) The duration of orthodontic treatment. Am J Orthod Dentofac Orthop 102:45–51
Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ (1992) Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofac Orthop 101:403–407
Bishara SE, Ostby AW (2008) White spot lesions: formation, prevention, and treatment. Semin Orthod 14:174–182
Segal GR, Schiffman PH, Tuncay OC (2004) Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofacial Res 7:71–78
Pandis N, Nasika M, Polychronopoulou A, Eliades T (2008) External apical root resorption in patients treated with conventional and self-ligating brackets. Am J Orthod Dentofac Orthop 134:646–651
Royko A, Denes Z, Razouk G (1999) The relationship between the length of orthodontic treatment and patient compliance. Fogorv Sz 92:79–86
Cafaro A, Arduino PG, Massolini G, Romagnoli E, Broccoletti R (2013) Clinical evaluation of the efficiency of low-level laser therapy for oral lichen planus: a prospective case series. Lasers Med Sci
Ahrari F, Madani AS, Ghafouri ZS, Tuner J (2013) The efficacy of low-level laser therapy for the treatment of myogenous temporomandibular joint disorder. Lasers Med Sci
de Moraes Maia ML, Ribeiro MA, Maia LG, Stuginski-Barbosa J, Costa YM, Porporatti AL, Conti PC, Bonjardim LR (2012) Evaluation of low-level laser therapy effectiveness on the pain and masticatory performance of patients with myofascial pain. Lasers Med Sci
Orhan K, Aksoy U, Can-Karabulut DC, Kalender A (2011) Low-level laser therapy of dentin hypersensitivity: a short-term clinical trial. Lasers Med Sci 26:591–598
McRae E, Boris J (2013) Independent evaluation of low-level laser therapy at 635 nm for non-invasive body contouring of the waist, hips, and thighs. Lasers Surg Med 45:1–7
Chow RT, Barnsley L (2005) Systematic review of the literature of low-level laser therapy (LLLT) in the management of neck pain. Lasers Surg Med 37:46–52
Minatel DG, Frade MA, Franca SC, Enwemeka CS (2009) Phototherapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med 41:433–441
Leal Junior EC, Lopes-Martins RA, Rossi RP, De Marchi T, Baroni BM, de Godoi V, Marcos RL, Ramos L, Bjordal JM (2009) Effect of cluster multi-diode light emitting diode therapy (LEDT) on exercise-induced skeletal muscle fatigue and skeletal muscle recovery in humans. Lasers Surg Med 41:572–577
Eslamian L, Borzabadi-Farahani A, Hassanzadeh-Azhiri A, Badiee MR, Fekrazad R (2013) The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci
Cruz DR, Kohara EK, Ribeiro MS, Wetter NU (2004) Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med 35:117–120
Melsen B (1999) Biological reaction of alveolar bone to orthodontic tooth movement. Angle Orthod 69:151–158
Altan BA, Sokucu O, Ozkut MM, Inan S (2012) Metrical and histological investigation of the effects of low-level laser therapy on orthodontic tooth movement. Lasers Med Sci 27:131–140
Kawasaki K, Shimizu N (2000) Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg Med 26:282–291
Aleksic V, Aoki A, Iwasaki K, Takasaki AA, Wang CY, Abiko Y, Ishikawa I, Izumi Y (2010) Low-level Er:YAG laser irradiation enhances osteoblast proliferation through activation of MAPK/ERK. Lasers Med Sci 25:559–569
Shirazi M, Ahmad Akhoundi MS, Javadi E, Kamali A, Motahhari P, Rashidpour M, Chiniforush N (2013) The effects of diode laser (660 nm) on the rate of tooth movements: an animal study. Lasers Med Sci
Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C (2006) Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofacial Res 9:38–43
Gui L, Qu H (2008) Clinical application of low energy laser in acceleration of orthodontic tooth movement. J Dalian Med Univ 30:155–156
Sousa MV, Scanavini MA, Sannomiya EK, Velasco LG, Angelieri F (2011) Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg 29:191–196
Higgin JPT, Altman DG, Sterne JAC (2011) Chapter 8: Assessing risk of bias in included studies. In: Higgin JPT and Green S (eds) 5.1.0 [updated March 2011]. The Cochrane Collaboration
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ (2011) GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL, Williams JW Jr, Atkins D, Meerpohl J, Schunemann HJ (2011) GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). J Clin Epidemiol 64:407–415
Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, Alonso-Coello P, Djulbegovic B, Atkins D, Falck-Ytter Y, Williams JW Jr, Meerpohl J, Norris SL, Akl EA, Schunemann HJ (2011) GRADE guidelines: 5. Rating the quality of evidence—publication bias. J Clin Epidemiol 64:1277–1282
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schunemann HJ, Group GW (2011) GRADE guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol 64:1294–1302
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Falck-Ytter Y, Jaeschke R, Vist G, Akl EA, Post PN, Norris S, Meerpohl J, Shukla VK, Nasser M, Schunemann HJ, Group GW (2011) GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol 64:1303–1310
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, Devereaux PJ, Montori VM, Freyschuss B, Vist G, Jaeschke R, Williams JW Jr, Murad MH, Sinclair D, Falck-Ytter Y, Meerpohl J, Whittington C, Thorlund K, Andrews J, Schunemann HJ (2011) GRADE guidelines 6. Rating the quality of evidence—imprecision. J Clin Epidemiol 64:1283–1293
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofac Orthop 141:289–297
Ankri R, Lubart R, Taitelbaum H (2010) Estimation of the optimal wavelengths for laser-induced wound healing. Lasers Surg Med 42:760–764
Moore P, Ridgway TD, Higbee RG, Howard EW, Lucroy MD (2005) Effect of wavelength on low-intensity laser irradiation-stimulated cell proliferation in vitro. Lasers Surg Med 36:8–12
Lau J, Schmid CH, Chalmers TC (1995) Cumulative meta-analysis of clinical trials builds evidence for exemplary medical care. J Clin Epidemiol 48:45–57, discussion 59-60
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Long, H., Zhou, Y., Xue, J. et al. The effectiveness of low-level laser therapy in accelerating orthodontic tooth movement: a meta-analysis. Lasers Med Sci 30, 1161–1170 (2015). https://doi.org/10.1007/s10103-013-1507-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1507-y