Abstract
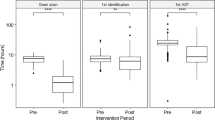
The implications of the variables within the pre-analytical phase of blood culture processing are poorly understood. This study aims to explore the effect of transit times (TT) and culture volume, on time to microbiological diagnosis and patient outcomes. Blood cultures received between 1st March and 31st July 2020/21 were identified. TT, time in incubator (TII), and for positive samples, request to positivity times (RPT) were calculated. Demographic details were recorded for all samples, and culture volume, length of stay (LoS), and 30-day mortality for patients with positive samples. Statistical analysis examined how culture volume and TT effected culture positivity and outcome; in the context of the 4-h national TT target. Totally, 14,375 blood culture bottles were received from 7367 patients; 988 (13.4%) were positive for organisms. There was no significant difference between TT of negative and positive samples. The RPT was significantly lower for samples with TT < 4 h (p < 0.001). Culture bottle volume did not affect RPT (p = 0.482) or TII (p = 0.367). A prolonged TT was associated with a longer length-of-stay in those with a bacteraemia with a significant organism (p = 0.001). We found shorter blood culture transportation time was associated with a significantly faster time of positive culture reporting, while optimal blood culture volume did not make a significant impact. Delays in reporting for significant organisms correspond to a prolonged LoS. Laboratory centralisation makes achieving the 4-h target a logistical challenge; however, this data suggests such targets have significant microbiological and clinical impacts.


Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Public Health England (2019) UK Standards for Microbiology Investigations Investigation of blood cultures (for organisms other than Mycobacterium species). Standards Unit NIS (ed). Available online at: https://www.gov.uk/government/publications/smi-b-37-investigation-of-blood-cultures-fororganisms-other-than-mycobacterium-species
Kadri SS, Lai YL, Warner S, Strich JR, Babiker A, Ricotta EE, Demirkale CY, Dekker JP, Palmore TN, Rhee C, Klompas M, Hooper DC, Powers JH 3rd, Srinivasan A, Danner RL, Adjemian J (2021) Inappropriate empirical antibiotic therapy for bloodstream infections based on discordant in-vitro susceptibilities: a retrospective cohort analysis of prevalence, predictors, and mortality risk in US hospitals. Lancet Infect Dis 21(2):241–251
Sakata RAP, Cayô da Silva R, Gales AC, Cuba GT, Pignatari ACC, Kiffer CRV (2022) Broad-spectrum antimicrobial consumption trends and correlation with bacterial infections and antimicrobial resistance over 5 years. Journal of Global Antimicrobial Resistance 28:115–119
Aliabadi S, Anyanwu P, Beech E, Jauneikaite E, Wilson P, Hope R, Majeed A, Muller-Pebody B, Costelloe C (2021) Effect of antibiotic stewardship interventions in primary care on antimicrobial resistance of Escherichia coli bacteraemia in England: a quasi-experimental, ecological, data linkage study. Lancet Infect Dis 21(12):1689–1700
Barenfanger J, Drake C, Kacich G (1999) Clinical and financial benefits of rapid bacterial identification and antimicrobial susceptibility testing. J Clin Microbiol 37(5):1415–1418
Buehler SS, Madison B, Snyder SR, Derzon JH, Cornish NE, Saubolle MA, Weissfeld AS, Weinstein MP, Liebow EB, Wolk DM (2016) Effectiveness of practices to increase timeliness of providing targeted therapy for inpatients with bloodstream infections: a laboratory medicine best practices systematic review and meta-analysis. Clin Microbiol Rev 29(1):59–103
Venturelli C, Righi E, Borsari L, Aggazzotti G, Busani S, Mussini C, Rumpianesi F, Rossolini GM, Girardis M (2017) Impact of pre-analytical time on the recovery of pathogens from blood cultures: results from a large retrospective survey. PLoS ONE 12(1):e0169466
Ling CL, Roberts T, Soeng S, Cusack T-P, Dance DAB, Lee SJ, Reed TAN, Hinfonthong P, Sihalath S, Sengduangphachanh A, Watthanaworawit W, Wangrangsimakul T, Newton PN, Nosten FH, Turner P, Ashley EA (2021) Impact of delays to incubation and storage temperature on blood culture results: a multi-centre study. BMC Infect Dis 21(1):173
Lambregts MMC, Bernards AT, van der Beek MT, Visser LG, de Boer MG (2019) Time to positivity of blood cultures supports early re-evaluation of empiric broad-spectrum antimicrobial therapy. PLoS ONE 14(1):e0208819
Saito T, Iinuma Y, Takakura S, Nagao M, Matsushima A, Shirano M, Ichiyama S (2009) Delayed insertion of blood culture bottles into automated continuously monitoring blood culture systems increases the time from blood sample collection to the detection of microorganisms in bacteremic patients. J Infect Chemother 15(1):49–53
van der Velden LB, Vos FJ, Mouton JW, Sturm PD (2011) Clinical impact of preincubation of blood cultures at 37°C. J Clin Microbiol 49(1):275–280
Morton B, Nagaraja S, Collins A, Pennington SH, Blakey JD (2015) A retrospective evaluation of critical care blood culture yield — do support services contribute to the “weekend effect”? PLoS ONE 10(10):e0141361
Schwarzenbacher J, Kuhn SO, Vollmer M, Scheer C, Fuchs C, Rehberg S, Balau V, Hahnenkamp K, Bohnert JA, Gründling M (2019) On-site blood culture incubation shortens the time to knowledge of positivity and microbiological results in septic patients. PLoS ONE 14(12):e0225999
Deslandes V, Rafipour D, Gorn I, Sabri E, Sant N, Desjardins M (2022) Effect of delayed entry of blood culture bottles in BACTEC automated blood culture system in the context of laboratory consolidation. Sci Rep 12(1):1337
Rönnberg C, Mildh M, Ullberg M, Özenci V (2013) Transport time for blood culture bottles: underlying factors and its consequences. Diagn Microbiol Infect Dis 76(3):286–290
Hall MM, Ilstrup DM, Washington JA 2nd (1976) Effect of volume of blood cultured on detection of bacteremia. J Clin Microbiol 3(6):643–645
Kim SC, Kim S, Lee DH, Choi SR, Kim JS (2015) Effect of blood volume in standard anaerobic blood culture bottles of the BacT/ALERT 3D system used for the detection of pathogens and time to detection. PLoS ONE 10(2):e0116728
Sastry A, Binu N, Anitha GAG, Deepashree SS (2020) Effect of blood volume in automated blood culture of the BACT/ALERT 3D system on isolation rate and time to positivity of pathogens, in a tertiary care hospital, South India. IP Int J Med Microbiol Trop Dis 5:176–180
Davies PMM (2021) Streamlining the transport pathway has significantly reduced the pre-analytical phase of blood cultures in two regional hospitals. Federation of Infectious Societies Annual Conference Manchester Central, UK. Poster 175: Federation of Infectious Diseases Annual Conference. Available online at: https://az659834.vo.msecnd.net/eventsairwesteuprod/production-fitwisepublic/c73ca41748814cf78bc73fab15f5c5d2
McGregor C (2014) Improving time to antibiotics and implementing the ”Sepsis 6”. BMJ Qual Improv Rep 2(2):u202548.w201443. https://doi.org/10.1136/bmjquality.u202548.w1443
Kerremans JJ, van der Bij AK, Goessens W, Verbrugh HA, Vos MC (2009) Immediate incubation of blood cultures outside routine laboratory hours of operation accelerates antibiotic switching. J Clin Microbiol 47(11):3520–3523
Péan de Ponfilly G, Benmansour H, Manda V, Lecorche E, Mougari F, Munier AL, Temim S, Amarsy R, Jacquier H, Cambau E (2021) Impact of 24/7 loading of blood culture bottles in a new automated incubator on the diagnosis of bloodstream infections. Eur J Clin Microbiol Infect Dis 40(12):2639–2643
Bruins MJ, Egbers MJ, Israel TM, Diepeveen SH, Wolfhagen MJ (2017) Reduced length of hospital stay through a point of care placed automated blood culture instrument. Eur J Clin Microbiol Infect Dis 36(4):619–623
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Peter Davies and Timothy Jones. The first draft of the manuscript was written by Peter Davies and Timothy Jones, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is a retrospective observational study, and ethical approval was not required. The Caldicott Guardian consented to data access for the study.
Consent to participate and to publication
As this was a retrospective observational study, consent was not possible.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Davies, P.J.B., Jones, T.P.W. & Macleod, M. An assessment of the downstream implications of blood culture collection and transit. Eur J Clin Microbiol Infect Dis 42, 835–842 (2023). https://doi.org/10.1007/s10096-023-04610-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04610-z