Abstract
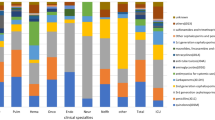
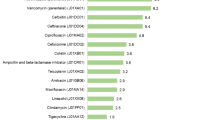
The purpose of this study is to implement point prevalence survey (PPS), assess antimicrobial prescribing and resistance in general hospitals and clinical specialties in China, and compare them with similar data from other parts of the world. Twenty general hospitals in China were surveyed in October or November, 2019. A standardized surveillance protocol was used to collect data on patient demographics, diagnosis of infection, the prevalence and intensity of antimicrobial use, prescribing quality, bacterium type and resistance spectrum, and the prevalence and type of healthcare-associated infections (HAIs). Overall, 10,881 beds and 10,209 inpatients were investigated. The overall prevalence of antibiotic use was 37.00%, the use of antibiotic prophylaxis in surgical patients was high (74.97%). The intensity of antimicrobial use was 61.25 DDDs/100 patient days. Only 11.62% of antimicrobial prescriptions recorded the reason for prescribing. Intravenous or combination treatments comprised 92.02% and 38.07%, respectively, and only 30.65% of prescriptions referred to a microbiological or biomarker tests. The incidence of HAIs in all patients was 3.79%. The main associated factors for HAIs included more frequent invasive procedures (27.34%), longer hospital stay (> 1-week stay accounting for 51.47%), and low use of alcohol hand rubs (only 29.79% placed it bedside). Most of the resistant bacteria declined; only carbapenem-resistant Enterobacter is higher than previously reported. The prevalence of antibiotic use in general hospitals fell significantly, the overall bacterial resistance declined, and the incidence of HAI was low. However, the low quality of antimicrobial use requires urgent attention.


Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 2GC:
-
Second-generation cephalosporins
- 3GC:
-
Third-generation cephalosporins
- AMR:
-
Antimicrobial resistance
- AMS:
-
Antimicrobial stewardship
- CAI:
-
Community-acquired infections
- DDDs:
-
Defined daily dosages
- EARS-net:
-
The European Antimicrobial Resistance Surveillance Network
- GDP:
-
Gross domestic product
- HAI:
-
Healthcare-associated infection
- ICU:
-
Intensive care unit
- MNH:
-
Municipal non–teaching hospital
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MTH:
-
Municipal teaching hospital
- NAUS:
-
National hospital antimicrobial use surveillance network
- NBRS:
-
National hospital bacterial resistance surveillance network
- NCH:
-
The Chinese National Health Commission
- NHAIS:
-
National healthcare-associated infection surveillance network
- PPS:
-
Point prevalence survey
- PVC:
-
Peripheral venous catheter
- RTI:
-
Respiratory tract infection
- UK:
-
The United Kingdom
- USA:
-
The United States of America
- USD:
-
US dollar
- UTH:
-
University teaching hospitals
- UTI:
-
Urinary tract infection
- WHO:
-
The World Health Organization
References
Antimicrobial Resistance Collaborators (2022) Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399:629–655
Declaration of the G7 Health Ministers. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/G/G7/G7_Health_Ministers_Declaration_AMR_and_EBOLA.pdf
G20 leaders’ communique Hangzhou summit. http://www.g20chn.org/English/Dynamic/201609/t20160906_3396.html
WHO. Global action plan on antimicrobial resistance. https://www.who.int/publications/i/item/9789241509763
Xiao Y, Shen P, Zheng B, Zhou K, Luo Q, Li L (2020) Change in antibiotic use in secondary and tertiary hospitals nationwide after a national antimicrobial stewardship campaign was launched in China, 2011-2016: An Observational Study. J Infect Dis 221(Suppl 2):S148–S155
NHC. Notice on issuing the National Action Plan to Contain AMR (2016-2020). http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=f1ed26a0c8774e1c8fc89dd481ec84d7
Xiao Y, Li L (2016) China’s national plan to combat antimicrobial resistance. Lancet Infect Dis 16(11):1216–1218
National Health Commission of China. Report on antimicrobial stewardship and bacterial resistance in China (2016-2018). http://www.nhc.gov.cn/yzygj/s3594/201904/1b5a42f0e326487295b260c813da9b0e.shtml
Ansari F, Erntell M, Goossens H et al (2009) The European surveillance of antimicrobial consumption (ESAC) point-prevalence survey of antibacterial use in 20 European hospitals in 2006. Clin Infect Dis 49:1496–1504
Versporten A, Zarb P, Caniaux I et al (2018) Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: results of an internet-based global point prevalence survey. Lancet Glob Health 6:e619–e629
Magill S, Edwards J, Bamber W et al (2014) Multistate point-prevalence survey of health care–associated infections. N Engl J Med 370:1198–1208. https://doi.org/10.1056/NEJMoa1306801
World Health Organization (2018) WHO methodology for point prevalence survey on antibiotic use in hospitals. WHO, Geneva
European Centre for Disease Prevention and Control (2013) Point prevalence survey of healthcare associated infections and antimicrobial use in European acute care hospitals. ECDC, Stockholm
Plachouras D, Kärki T, Hansen S et al (2018) the Point Prevalence Survey Study Group. Antimicrobial use in European acute care hospitals: results from the second point prevalence survey (PPS) of healthcare-associated infections and antimicrobial use, 2016 to 2017. Euro Surveill 23(46):1800393
Magill SS, O’Leary E, Ray SM et al (2021) Antimicrobial use in US hospitals: comparison of results from emerging infections program prevalence surveys, 2015 and 2011. Clin Infect Dis 72(10):1784–1792
Wu CT, Chen CL, Lee HY et al (2017) Decreased antimicrobial resistance and defined daily doses after implementation of a clinical culture-guided antimicrobial stewardship program in a local hospital. J Microbiol Immunol Infect 50(6):846–856
Hara GL, Rojas-Cortes R, Leon HFM et al (2022) Point prevalence survey of antibiotic use in hospitals in Latin American countries. J Antimicrob Chemother 77:807–815
Magill SS, O’Leary E, Ray SM et al (2021) Assessment of the appropriateness of antimicrobial use in US hospitals. JAMA Netw Open 4(3):e212007. https://doi.org/10.1001/jamanetworkopen.2021.2007
Kim BY, Hwang HJ, Kim J et al (2020) Ten-year trends in antibiotic usage at a tertiary care hospital in Korea, 2004 to 2013. Korean J Intern Med 35:703–713
Komagamine J, Yabuki T, Kobayashi M et al (2019) Prevalence of antimicrobial use and active healthcare-associated infections in acute care hospitals: a multicentre prevalence survey in Japan. BMJ Open 9(6):e027604. https://doi.org/10.1136/bmjopen-2018-027604
Magill SS, O’Leary E, Janelle SJ et al (2018) Changes in prevalence of health care–associated infections in U.S. hospitals. N Engl J Med 379:1732–1744
Kim MJ, Park ES, Jeong JS et al (2000) Multicenter surveillance study for nosocomial infections in major hospitals in Korea. Nosocomial Infection Surveillance Committee of the Korean Society for Nosocomial Infection Control. Am J Infect Control 28(6):454–458
Xiao YH, Giske CG, Wei ZQ, Shen P, Heddini A, Li LJ (2011) Epidemiology and characteristics of antimicrobial resistance in China. Drug Resist Updat 14(4-5):236–250
European Centre for Disease Prevention and Control (2022) Antimicrobial resistance in the EU/EEA (EARS-Net) -Annual Epidemiological Report 2020. ECDC, Stockholm
Kajihara T, Yahara K, Hirabayashi A et al (2021) Japan Nosocomial Infections Surveillance (JANIS): current status, international collaboration, and future directions for a comprehensive antimicrobial resistance surveillance system. Jpn J Infect Dis 74(2):87–96
Sader HS, Castanheira M, Streit JM et al (2020) Frequency and antimicrobial susceptibility of bacteria causing bloodstream infections in pediatric patients from United States (US) medical centers (2014-2018): therapeutic options for multidrug-resistant bacteria. Diagn Microbiol Infect Dis 98(2):115108
Chen Y, Zhao J, Shan X et al (2017) A point-prevalence survey of healthcare-associated infections in 52 Chinese hospitals. J Hospital Infect 95(1):105–111. https://doi.org/10.1016/j.jhin.2016.08.010
Wang J, Hu J, Harbarth S et al (2017) Burden of healthcare-associated infections in China: results of the 2015 point prevalence survey in Dong Guan City. J Hospital Infect 96(2):132–138. https://doi.org/10.1016/j.jhin.2017.02.014
Ren N, Zhou PC, Wen X et al (2016) Point prevalence survey of antimicrobial use in Chinese hospitals in 2012. Am J Infect Control 44(3):332–339
Zhang Y, Zhong ZF, Chen SX et al (2019) Prevalence of healthcare-associated infections and antimicrobial use in China: results from the 2018 point prevalence survey in 189 hospitals in Guangdong Province. Int J Infect Dis 89:179–184
National Health Commission of China. Notice on conducting continually antimicrobial stewardship campaign in hospitals.http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=c79c998bdf8f4744858051cdfd1e6818
Xiao Y (2018) Antimicrobial stewardship in China: systems, actions and future strategies. Clin Infect Dis 67(suppl_2):S135–S141
Acknowledgements
We gratefully acknowledge the contributions of the members of China PPS for collection of the data in this study. We are very grateful to Professor Dilip Nathwani (Ninewells Hospital and Medical School, Dundee) for his critical reading and comment to the manuscript.
Funding
YX was supported by funding from Zhejiang Province (No. 2021C03068).
Author information
Authors and Affiliations
Consortia
Contributions
YX and QY conceived of and designed the study; YX and YC collected the data and interpreted the data; YX, YC, and XX conducted statistical analysis; YX wrote the manuscript; all authors critically reviewed and contributed revisions to the final version of the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The PPS was approved by the ethics committee of the First Affiliated Hospital of Zhejiang University (approval number: 2019-093). The study does not involve the patient’s personal information and is exempt from signing the informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1:
Table S. Hospital name and their locations
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiao, Y., Xin, X., Chen, Y. et al. Antimicrobial use, healthcare-associated infections, and bacterial resistance in general hospitals in China: the first national pilot point prevalence survey report. Eur J Clin Microbiol Infect Dis 42, 715–726 (2023). https://doi.org/10.1007/s10096-023-04602-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04602-z