Abstract
Studies of the incidence of pertussis in adults have shown that it accounts for only 5–15% cases of prolonged coughing. We assessed the burden of suffering related to prolonged coughing and tried to identify further causative agents. Based on a sentinel study with 35 general practitioners in two German cities (Krefeld, Rostock), with 3,946 patients fulfilling the inclusion criteria, we estimated the incidence of prolonged coughing in adults. In 975 of these outpatients, PCR and/or serology for adenovirus, Bordetella pertussis and B. parapertussis, human metapneumovirus, influenza virus A and rhinovirus, parainfluenza virus, Mycoplasma pneumonia, and respiratory syncytial virus (RSV) were performed. Treatment data were extracted for a subgroup of 138 patients. Descriptive statistics, including Kaplan–Maier curves were generated. Yearly incidence ranged between 1.4 and 2.1% per population in the two cities. Adult patients sought medical attention only after a median of 3 weeks of coughing. Irrespective of smoking and unrelated to the identified pathogens, the median duration of coughing was 6 weeks, with an interquartile range of 4–11 weeks. In 48.3% of patients, possible pathogens were identified, among which adenovirus (15.1%), RSV (7.5%), B. pertussis (5.6%), and influenza viruses (4.0%) were most often found. Symptoms were not indicative of a specific agent and a total of 64% of patients received antibiotics. Prolonged adult coughing requiring medical attention prompts substantial healthcare use. Apart from B. pertussis, a broad range of pathogens was associated with the symptoms. However, patients sought medical attention too late to guide efficacious therapeutic interventions using the diagnostic tests.
Similar content being viewed by others
Introduction
Studies of the incidence of infections with Bordetella pertussis in adults presenting with prolonged dry coughing spells without much malaise and mostly without fever [1, 2] have reproducibly shown that pertussis accounts for only 5–15% of these cases. Even in a vaccine trial of an acellular pertussis vaccine in adults with active surveillance of all coughing episodes lasting more than 1 week, only around 5% were caused by B. pertussis [3]. We therefore wondered, which other agents might be responsible for prolonged coughing in nonpertussis cases. We had the opportunity to address this question in a data set originally collected to generate estimates about the population incidence of adult pertussis in Germany [4]. In this dataset, the available biological samples allowed us to extend the diagnostic tests to various pathogens known to be related to acute respiratory infections (ARI) [5].
In contrast to pediatric infections caused by the same microorganisms, adult disease is usually no primary infection, and the symptoms of re-infections may be different. Almost all adult outpatients with respiratory symptoms are seen by general practitioners (GP) and internists. Most of the diseases do not require antibiotic treatment, whereas those caused by Bordetella spp. or Mycoplasma spp. might.
The objective of this study was to describe the overall burden of disease of prolonged coughing in adults, to find out which microorganisms contributed to prolonged coughing, and to assess whether specific clinical symptoms could distinguish between different agents.
Patients and methods
Patients
Patients were recruited by GPs and internists, who were working in general internal medicine (summarized as GPs) in Krefeld (KR) and Rostock (HRO), Germany. The study was recruiting patients between October 2001 and December 2004 in Krefeld, and between October 2002 and December 2004 in HRO. During this time, a total of 3,946 patients fulfilled the inclusion criteria. The study had 21 sentinels in HRO and 14 in KR. This study was approved by the ethical committees of the Medical Boards in KR (Ethikkommission bei der Ärztekammer Nordrhein, Lfd. Nr.: 2,000,269) and HRO (Ethikkommission bei der Ärztekammer Mecklenburg-Vorpommern, Reg. Nr.: I42/01. Arzneimittelüberwachung MV: Lfd. Nr. AMÜSt 20a/610.1).
Inclusion criteria
Adult patients (≥18 years), who coughed for 7 days or more and who sought medical attention could be included. Patients, who were treated for chronic respiratory diseases, such as COPD, were excluded. Patients participating in other studies were also excluded upon request by the ethical committees. Clinical data about symptoms, contacts, and duration of coughing were collected by two questionnaires, the second to be sent back when symptoms had subsided.
To estimate the population-based incidence, all sentinels individually reported the overall numbers of patients treated during the observation period. From a total of 138 randomly selected patients in practices with an electronic database and willing to contribute to this subset, all relevant treatment data were collected individually by analyzing all available medical records in the respective sentinels by three of the authors (ML, MR, CHWvK).
Incidence estimates
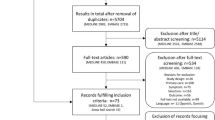
The city of HRO in former East Germany had a mean adult (>18 years) population of 170,067 during the study period, and KR in former West Germany had a mean adult population of 195,361. Consultation numbers for statutorily insured patients were made available from the “Kassenärztliche Vereinigungen” in HRO and KR. The proportion of privately insured patients was estimated to be 5.0% in HRO and 7.7% in KR. During the study period, we estimated 1,104,461 consultations (1,051,868 statutory insurance, 52,593 private insurance) in HRO, and 1,857,640 in KR (1,726,431 statutory insurance, 131,209 private insurance; Fig. 1).
Algorithm according to Strebel et al. [6] extrapolating the number of patients in sentinels to overall estimates of population-based incidences of longer lasting coughs in German adults
To estimate the population-based incidence, we made the following assumptions:
-
1.
The frequency of patients with longer lasting coughs in sentinels would be the same as in all GPs’ offices.
-
2.
The distribution of patients with prolonged coughs would not differ between GPs and internists.
-
3.
The relationship between patients with social medical insurance patients and those with private medical insurance would be similar between sentinel physicians and all physicians.
-
4.
The number of patients leaving and entering the catchment area would be the same.
The conversion of sentinel data into population-based incidence estimates was carried out according to a method suggested by Strebel et al. [6]. Briefly, as shown in Fig. 1, we extrapolated the overall study population from individual data from physicians in conjunction with population and consultation data.
Diagnostic procedures
We received diagnostic samples from a total of 975 patients (24.7%). Other patients fulfilling the inclusion criteria were not included owing to work overload in the physician’s office or lack of consent of the patients. A nasopharyngeal swab, pharyngeal washings, and a peripheral blood sample were taken from the patients, when they first presented at the sentinels. We were able to perform PCRs from 974 samples and serology from 965 samples. Nasopharyngeal swabs were immersed into modified AMIES medium with charcoal. Pharyngeal washings were collected into a sterile tube. All samples were transported at an ambient temperature to the laboratory. For tests not immediately performed, samples were frozen at −80 °C.
Laboratory tests
Nasopharyngeal swabs were tested for Bordetella-DNA by real-time PCR targeting IS 481 (B. pertussis) and IS1001 (B. parapertussis) [7]. Pharyngeal washings were tested for adenovirus DNA, influenza viruses A and B, human metapneumovirus and rhinovirus RNA by in-house real-time PCRs. In the throat washings, PCR was inhibited in 0.8%. For adenovirus DNA, a 131-base pair (bp) fragment of the hexon gene of human adenovirus type 2 was amplified [8]. For influenza A virus RNA, a 101-bp fragment from the M gene was amplified, and the reverse primer was degenerate. For influenza B virus RNA, an 89-nucleotide fragment from the M gene was amplified [9]. For detection of human rhinovirus RNA, a 67-nucleotide fragment from the 5′-UTR region of the genome was amplified. A second primer pair was added to detect an additional 13 subtypes [10]. For human metapneumovirus RNA, a 200-bp fragment from the N gene was used [11]. Primer and probes for rhinovirus and human metapneumovirus were adapted according to sequence alignment. All real-time PCRs with Ct values of >40 were regarded as negative. Samples with Ct values between 36 and 40 were re-analyzed and regarded as positive, when Ct values were reproducible. PCR-positive samples were regarded as indicative of any agent, irrespective of serological results.
Serology
Serum samples were tested for IgG and IgA antibodies to adenovirus, for IgG and IgA antibodies to influenza virus A and B, for IgG and IgM antibodies to Mycoplasma pneumoniae, for IgA antibodies to human parainfluenza viruses 1–3, and for IgG and IgA antibodies to respiratory syncytial virus (RSV) using ELISAs (all VirionSerion, Würzburg, Germany). IgG and IgA antibodies to pertussis toxin (PT) were measured using an in-house ELISA [12]. Interpretation of serology: commercial ELISAs measured antibodies quantitatively in arbitrary units (AU/ml). The cut-offs of the IgG ELISAs for viral serology were set to detect no antibodies in healthy blood donors and IgA antibodies to viral antigens and/or IgM antibodies to M. pneumoniae above the cut-off were also regarded as indicative of recent contact. For IgG anti-PT, recommendations of the European reference laboratories were followed [13], and ≥100 IU/ml and IgA-anti-PT ≥12 IU/ml were regarded as indicative of recent contact. Irrespective of isotype, antibodies to influenza virus A and influenza virus B were not interpreted as a recent contact, when patients were reported to be vaccinated against influenza or no information about influenza vaccination was available.
Statistical analysis
We calculated statistics using SAS, version 9.4 (SAS Institute, Cary, NC, USA). For continuous outcomes, which were not normally distributed, we used the Kruskal–Wallis test. For categorical outcomes we used the Pearson Chi-squared test. Kaplan–Meier curves were plotted for survival curves depicting persistence of coughing. Censoring criteria were stopping of coughing at any particular week and week 26, because coughing beyond 26 weeks was considered not to be related to the pathogens. p values <0.05 were considered significant.
Results
Between October 2001 and December 2004, a total of 3,946 patients fulfilled the inclusion criteria, of which 2,720 were from HRO and 1,226 from KR. Of these, a total of 975 (24.7%) were included in the study and 67% were female (n = 650). The female/male ratio did not significantly differ between HRO and KR. Median age was 50.2 years (44.8 in HRO, 54.5 in KR) and the range was 18.0–87.8 years.
The algorithm for estimating population-based incidence according to Strebel et al. [6] was applied as outlined in Fig. 1. In KR the sentinels represented 13.2% of patients with social medical insurance and 18.7% of those with private medical insurance. The overall number of patient contacts during the study period (13 quarters) was 228,800 in patients with social medical insurance and 24,570 of those with private medical insurance. In HRO, the sentinels represented 33.9% of patients with social medical insurance and 40.8% of those with private medical insurance. The overall number of patient contacts during the study period (9 quarters) was 357,345 patients with medical insurance and 21,438 patients with private medical insurance.
Burden of disease
As outlined in Fig. 1, we estimated the overall incidence of longer lasting coughs in adults to be between 1,400 and 2,100 per 100,000 per year. The proportion of smokers in the study population was 26.1% (254 smoked, 718 did not smoke, and 3 provided no data). We had information about the duration of cough from 611 patients. The median duration of coughing, irrespective of the pathogen identified, was 6 weeks, with an interquartile range of 4–11 weeks. No significant difference in the duration of cough was found between patients in KR and those in HRO. The duration of coughing did not differ between smokers and nonsmokers (p value: 0.4975; Fig. 2).
The subgroup of 138 patients with assessment of medical resource use and treatment was in respect to gender and age distribution, the subgroup was not statistically different from the overall cohort in respect to gender and age distribution. These patients had a total of 624 contacts related to coughing with their GPs. The mean and median number of contacts was 4·0 per patient (Range: 1–35). A total of 30% (41/138) of the sub cohort were referred to another specialist, i.e. radiologists for a chest x-ray (n = 18) or ENT specialists (n = 14). Overall, 85% of patients were prescribed any type of drug, and these were mostly antibiotics (64%), antitussives (37%), a mucolytic agent (45%) or steroids (17%) (Table 1). Among the antibiotics, macrolides, aminopenicillins, and tetracycline were prescribed most frequently. Many of the patients received more than one drug, and 17% of those with antibiotics received more than one antibiotic.
Pathogens and symptoms
We identified a possible infectious cause of coughing in 48.3% of the patients (Table 2). Any positive PCR was found in 8 out of /974 cases (8.9%), and any positive serology was observed in 383 out of 965 cases (39.7%). The probability of positive PCR results ranging between 0.6% (human metapneumovirus) and 2.3% (adenovirus) was similar for all pathogens tested with overlapping 95% CIs. The most frequent pathogens identified by serology were adenovirus, RSV, and B. pertussis in decreasing order, with disjunctive 95% CIs in between and compared with all other pathogens with positive tests. Mixed infections occurred in 9.4% and various combinations of positive tests were found, most frequently adenovirus plus RSV, RSV plus B. pertussis, and adenovirus plus M. pneumoniae.
According to the inclusion criteria, all patients coughed for 7 days or more. Table 3 relates the symptoms in patients, from whom information on symptoms were available (n = 733) to the results of the diagnostic tests. The pathogen spectrum in patients filling out the questionnaires did not differ from the overall study cohort. As shown in Table 3, the patients had coughed for 3 weeks in median (interquartile range: 2–5 weeks) before consulting a physician. Fever was only found in 23.6% on average (228 had fever, 738 had no fever, and 8 provided no data) and 48.6% reported choking (468 choked, 495 did not choke, and 11 provided no data). None of the reported symptoms in the patients with a positive test was significantly different from symptoms found in patients with negative tests. As expected, fever was reported more often from influenza patients, but at a similar frequency also from RSV patients. Figure 3 shows a survival analysis for 596 out of 611 patients who had a positive test for adenovirus, RSV, B. pertussis, influenza viruses, mixed infections, or who had no positive test (15 patients positive for other pathogens were excluded). Overall, patients infected with B. pertussis seemed to cough longer than the others, without reaching significance.
Kaplan–Meier survival plots comparing the duration of symptoms in weeks as related to diagnostic tests in 596 German adult patients with complete information on the duration of coughing. Agents with n < 10 (human metapneumovirus, n = 3; rhinovirus, n = 7; and parainfluenza, n = 5) are not shown in the figure
Discussion
For adult pertussis, population-based incidence estimates for patients using medical resources varied between 0.15 and 0.5% per year [2], and around 1–2% with active surveillance [3]. The sentinel analyzed here estimated the population-based pertussis incidence at 0.16% per year [4]. Thus, the burden of suffering is known for pertussis, but unclear for most prolonged coughing in adults, affecting about 1.4 and 2.1% of the adult population annually. The condition is cumbersome owing to a median duration of coughing of 6 weeks, and it is a substantial burden to the healthcare system. In about half of the patients, a possible pathogen could be identified by the tests used in this study. However, patients visited their physicians only after coughing for 3 weeks in median, thus limiting the clinical relevance of diagnostic findings for therapeutic interventions. The duration of coughing was equal for smokers and nonsmokers and the proportion of smokers in our sample (26.1%) was similar to the 24.5% reported in the 2013 microcensus [14].
As the average duration of coughing was considerable, it is not surprising that patients visited their GPs frequently, and that drug prescription was frequent. More than 80% of the patients received some drug treatment, and antibiotics, antitussives and steroids were not recommended for these infections [15, 16]. However, probably because of the long-lasting symptoms, 63% of patients received antibiotics, 47% antitussives, and 17% steroids. A retrospective database analysis of drug prescriptions in influenza and influenza-like illnesses of much shorter duration of coughing in Germany [17] showed that in that cohort, around 50% of patients did not receive prescriptions. However, among those who did receive drugs, 40% received antibiotics (63% in our study) and 12% received antitussives (37% in our study).
There are a number of studies linking the pathogens considered in our analyses to ARI. Adenovirus outbreaks of ARI in young adults have plagued the military for some time, and recruits in the USA are vaccinated against adenovirus 4 and 7 [5]. M. pneumoniae is mostly associated with community-acquired pneumonia, and less so with ARI and prolonged coughing [5]. Using active surveillance, Szilagyi et al. [18] found that 13% were caused by coronavirus (not studied here), 12% by rhinovirus (2.8% PCR), 7% by RSV (7.6% serology), 4% by influenza virus (4.0% PCR and serology) and metapneumovirus (0.6% PCR), and 1% by adenovirus (15.1% PCR and serology). In their sample, however, only 39% of patients had a healthcare visit. Another US study [19] showed that among adults with febrile or severe ARI, around 40% were positive for any virus, with influenza virus and rhinovirus the leading causes. The importance of rhinovirus was also stressed by a European study pointing to the role of re-infections with another rhinovirus type [20]. Linking a laboratory database with telehealth service data in the UK, Morbey et al. [21] showed that the greatest burden of ARI was associated with influenza and RSV, and that RSV patients most often complained about coughing.
In our study, we established a role of these pathogens in prolonged adult coughing disease. Similar to the other studies and depending on the inclusion criteria for ARI, every pathogen accounted for only a relatively small proportion of cases. Therefore, targeted diagnostics would be tempting, if guidance by clinical symptoms were possible. Unfortunately, our data gave no hint of the potential role of specific clinical symptoms for either agent. Although a possibly relevant pathogen could be identified in half of the patients, diagnosis was too late for effective therapeutic interventions, as patients with prolonged coughing did not consult their GP before a median of 3 weeks after onset of symptoms.
The strength of our study is the substantial number of sentinel physicians included and the use of two cities for sampling. In accordance with a study from the UK [22], our cohort also showed a higher consultation rate for women among all age groups. To account for annual variability in the circulation of microorganisms, the study was performed over three winter seasons. However, there are some limitations. The sentinels consisted of GPs and internists who worked as GPs. Thus, we systematically missed few patients who primarily attended specialists such as pulmonologists, or ENT specialists. The age distribution differed between HRO and KR, and patients in HRO were younger than those in KR, and we could not identify any cause of this. We used nasopharyngeal swabs for B. pertussis PCR, and pharyngeal washings for viral PCRs. Nasopharyngeal swabs are recommended for pertussis, but pharyngeal washing represents a non-optimal material for viral PCRs [23].
As the patients were coughing for a median of 3 weeks before visiting their physician, the overall sensitivity of PCR testing was reduced, as viral shedding, i.e., for rhinovirus or RSV [20, 24, 25] is mostly shorter. For serology, we only collected an acute serum sample, and could not show titer increases, which would have improved the specificity. Diagnostic serology is relevant for pertussis and mycoplasma infections [13, 26], and in 9 patients with IgM antibodies to M. pneumoniae, we assumed a polyclonal response to multiple other antigens. Although viral serology is sometimes regarded as obsolete, we have recently shown that applying latent class analysis for validating diagnostic methods in the absence of a “gold standard,” single-sample viral serology may identify additional cases [27].
Regarding the external validity of our findings, the sampling period is critical. In respect to influenza, the season 2001/2002 was described as moderate, the 2002/2003 season was strong, and the 2003/2004 season was again moderate [28]. Pertussis occurs in 3- to 4-yearly epidemic waves, and notified cases of pertussis in former East Germany [29] indicated that the study was carried out during an interepidemic period. Therefore, it is possible that the proportion of cases with influenza or pertussis might be higher in other time periods. A more timely publication of our results would have been warranted; unfortunately, the data and analyses could only be generated with substantial delay. However, there is no reason to assume that this invalidates our findings.
In conclusion, our data show that prolonged adult coughing requiring medical attention is a cumbersome condition prompting substantial healthcare use and drug prescriptions. A broad range of pathogens beyond B. pertussis was associated with the symptoms. Unfortunately, most patients sought medical attention too late for these diagnostic procedures to guide efficacious therapeutic interventions.
References
Cherry JD, Tan T, Wirsing von König CH, Forsyth KD, Thisyakorn U, Greenberg D, Johnson D, Marchant C, Plotkin S (2012) Clinical definitions of pertussis: summary of a global pertussis initiative roundtable meeting, February 2011. Clin Infect Dis 54:1756–1764. https://doi.org/10.1093/cid/cis302
von König W, Halperin S, Riffelmann M, Guiso N (2002) Pertussis of adults and infants. Lancet Infect Dis 2:744–750
Ward JI, Cherry JD, Chang SJ, Partridge S, Keitel W, Edwards K, Lee M, Treanor J, Greenberg DP, Barenkamp S, Bernstein DI, Edelman R, APERT Study Group (2006) Bordetella pertussis infections in vaccinated and unvaccinated adolescents and adults, as assessed in a national prospective randomized acellular pertussis vaccine trial (APERT). Clin Infect Dis 43:151–157
Riffelmann M, Littmann M, Hülsse C, O’Brien J, Wirsing von König CH (2006) Pertussis: incidence, symptoms and costs. Dtsch Med Wochenschr 131:2829–2834
Cesario TC (2012) Viruses associated with pneumonia in adults. Clin Infect Dis 55:107–113
Strebel P, Nordin J, Edwards K, Hunt J, Besser J, Burns S, Amundson G, Baughman A, Wattigney W (2001) Population-based incidence of pertussis among adolescents and adults, Minnesota, 1995–1996. J Infect Dis 183:1353–1359
Riffelmann M, Wirsing von König CH, Caro V, Guiso N (2005) Real-time polymerase chain reaction for diagnosis of Bordetella infections. J Clin Microbiol 43:4925–4929
Heim A, Ebent C, Harste G, Pring-Akerblom P (2003) Rapid and quantitative detection of human adenovirus DNA by real-time PCR. J Med Virol 70:228–239
Schulze M, Nitsche A, Schweiger B, Biere B (2010) Diagnostic approach for the differentiation of the pandemic influenza a (H1N1) virus from recent human influenza viruses by real-time PCR. PLoS One 5:e9966. https://doi.org/10.1371/journal.pone.00099
Wright PF, Deatly AM, Karron RA, Belshe RB, Shi JR, Gruber WC, Zhu Y, Randolph VB (2007) Comparison of results of detection of rhinovirus by PCR and viral culture in human nasal wash specimens from subjects with and without clinical symptoms of respiratory illness. J Clin Microbiol. 45:2126–2129
Bouscambert-Duchamp M, Lina B, Trompette A, Moret H, Motte J, Andréoletti L (2005) Detection of human metapneumovirus RNA sequences in nasopharyngeal aspirates of young French children with acute bronchiolitis by real-time reverse transcriptase PCR and phylogenetic analysis. J Clin Microbiol 43:1411–1414
Wirsing von König CH, Gounis D, Schmitt HJ, Laukamp S, Bogaerts H (1999) Single sample serological diagnosis of pertussis. Eur J Clin Microbiol Infect Dis 18:341–345
Guiso N, Berbers G, Fry NK, He Q, Riffelmann M, Wirsing von König CH, EU Pertstrain group (2011) What to do and what not to do in serological diagnosis of pertussis: recommendations from EU reference laboratories. Eur J Clin Microbiol Infect Dis 30:307–312. https://doi.org/10.1007/s10096-010-1104-y
Statistisches Bundesamt (Federal statistical office): Mikrozensus - Fragen zur Gesundheit; − Rauchgewohnheiten der Bevölkerung (Prevalence of smokers), https://www.destatis.de/DE/ZahlenFakten/GesellschaftStaat/Gesundheit/GesundheitszustandRelevantesVerhalten/Tabellen/Rauchverhalten.html. Accessed 17 Aug 2017)
Hurst JR, Saleh AD (2014) Neither anti-inflammatory nor antibiotic treatment significantly shortens duration of cough in acute bronchitis compared with placebo. Evid Based Med 19:98
Llor C, Moragas A, Bayona C, Morros R, Pera H, Plana-Ripoll O, Cots JM, Miravitlles M (2013) Efficacy of anti-inflammatory or antibiotic treatment in patients with non-complicated acute bronchitis and discoloured sputum: randomized placebo controlled trial. BMJ 347:f5762
Ehlken B, Anastassopoulou A, Hain J, Schröder C, Wahle K (2015) Cost for physician-diagnosed influenza and influenza-like illnesses on primary care level in Germany—results of a database analysis from May 2011 to April 2012. BMC Public Health 15:578
Szilagyi PG, Blumkin A, Treanor JJ, Gallivan S, Albertin C, Lofthus GK, Schnabel KC, Donahue JG, Thompson MG, Shay DK (2016) Incidence and viral aetiologies of acute respiratory illnesses (ARIs) in the United States: a population-based study. Epidemiol Infect 144(10):2077–2086. https://doi.org/10.1017/S0950268816000315
Radin JM, Hawksworth AW, Kammerer PE, Balansay M, Raman R, Lindsay SP, Brice GT (2014) Epidemiology of pathogen-specific respiratory infections among three US populations. PLoS One 9(12):e114871. https://doi.org/10.1371/journal.pone.0114871 eCollection 2014
Zlateva KT, de Vries JJ, Coenjaerts FE, van Loon AM, Verheij T, Little P, Butler CC, Goossens H, Ieven M, Claas EC, GRACE Study Group (2014) Prolonged shedding of rhinovirus and re-infection in adults with respiratory tract illness. Eur Respir J 44(1):169–177. https://doi.org/10.1183/09031936.00172113
Morbey RA, Harcourt S, Pebody R, Zambon M, Hutchison J, Rutter J, Thomas H, Smith GE, Elliot AJ (2017) The burden of seasonal respiratory infections on a national telehealth service in England. Epidemiol Infect 145:1922–1932. https://doi.org/10.1017/S095026881700070X
Hardelid P, Rait G, Gilbert R, Petersen I (2015) Recording of influenza-like illness in UK primary care 1995-2013: cohort study. PLoS One 10:e0138659. https://doi.org/10.1371/journal.pone.0138659
Lieberman D, Lieberman D, Shimoni A, Keren-Naus A, Steinberg R, Shemer-Avni Y (2009) Identification of respiratory viruses in adults: nasopharyngeal versus oropharyngeal sampling. J Clin Microbiol 47:3439–3443
Peltola V, Waris M, Kainulainen L, Kero J, Ruuskanen O (2013) Virus shedding after human rhinovirus infection in children, adults and patients with hypogammaglobulinaemia. Clin Microbiol Infect 19(7):E322. https://doi.org/10.1111/1469-0691.12193
Munywoki PK, Koech DC, Agoti CN, Kibirige N, Kipkoech J, Cane PA, Medley GF, Nokes DJ (2015) Influence of age, severity of infection, and co-infection on the duration of respiratory syncytial virus (RSV) shedding. Epidemiol Infect 143:804–812
Loens K, Ieven M (2016) Mycoplasma pneumoniae: current knowledge on nucleic acid amplification techniques and serological diagnostics. Front Microbiol. https://doi.org/10.3389/fmicb.2016.00448
Sobotzki C, Riffelmann M, Kennerknecht N, Hülsse C, Littmann M, White A, Von Kries R, Wirsing von König CH (2016) Latent class analysis of diagnostic tests for adenovirus, Bordetella pertussis and influenza virus infections in German adults with longer lasting coughs. Epidemiol Infect 144:840–846
der Heiden MA, Köpke K, Buda S, Buchholz U, Haas W (2013) Estimates of excess medically attended acute respiratory infections in periods of seasonal and pandemic influenza in Germany from 2001/02 to 2010/11. PLoS One 8:e64593. https://doi.org/10.1371/journal.pone.0064593.
Robert Koch-Institut (2005) Pertussis Morbidität in den neuen Bundesländern. Epidemiol Bull 23:195–198
Acknowledgements
Primarily, we thank all the patients who agreed to participate in this study. We would also like to thank all sentinel physicians:
Krefeld: Frau und Herr Dr Rieger, Praxis Dr Krausbauer und Frau Dr Möhrke, Herr Dr Dotzel, Herr Dr Frackenpohl, Praxis Dr Lüdemann und Herr Dr Schultz, Herr Dr Urban, Herr Dr Urlbauer, Herr Dr Baselt, Herr Dr Ridderskamp, Praxis Dr Hochbruck und Dr Hermann, Praxis Dr Kemmerich und Dr Thomaßen, Herr Dr Meißner, Herr Dr Seelhoff.
Rostock: Frau Dr Lusch, Herr Dr Rothe, Frau Dr Krüger, Herr Dr Th Hohlbein, Frau Dr Borchmann, Frau Dr Kähler, Frau Dr Bichowski, Frau Dr Lüder, Frau Dr Glaser, Frau Dr B Hohlbein, Frau Dr Vilbrandt, Herr Dr Anft, Frau Dr Burow, Frau Dr Olwig, Frau Dr Engelhardt, Frau Dr Lange, Herr Dr Langer, Frau Dr Evert, Frau Dr Michelsen, Frau Dr Frank, Frau Dr Morcan.
Funding
The logistics of the sentinel were funded jointly by GlaxoSmithKline Pharma, Munich, Germany and Sanofi Pasteur, Leimen, Germany, to produce estimates of the incidence of adult pertussis. Both sponsors had no influence on any part of the study. All other laboratory tests, the data analysis, and the production of the manuscript were not funded externally.
Author information
Authors and Affiliations
Contributions
RW, RvK and CHWvK wrote the manuscript. RW and RvK extracted and analyzed the data. CHWvK planned the study, and MR and CHWvK established and supervised the logistics in Krefeld, as CH and ML did in Rostock. NK supervised the laboratory work; JO’B collated the resource use data. All authors have read the manuscript, commented on it, and agreed to the final version.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest. For the sentinel physicians, products of pharmaceutical companies played no role; thus, all sentinel physicians declare that no conflicting interests were relevant in this study. Physicians received no remuneration in this study, doctor’s assistants received 25€ per patient for organizing the study logistics.
Ethical approval
This study was approved by the ethics committees of the Medical Boards in KR (Ethikkommission bei der Ärztekammer Nordrhein, Lfd. Nr.: 2,000,269) and HRO (Ethikkommission bei der Ärztekammer Mecklenburg-Vorpommern, Reg. Nr.: I42/01. Arzneimittelüberwachung MV: Lfd. Nr. AMÜSt 20a/610.1).
Informed consent
All adult patients included in this study were informed about the study goals and declared their consent to participate in the study by signing an appropriate form.
Rights and permissions
About this article
Cite this article
Weinberger, R., Riffelmann, M., Kennerknecht, N. et al. Long-lasting cough in an adult German population: incidence, symptoms, and related pathogens. Eur J Clin Microbiol Infect Dis 37, 665–672 (2018). https://doi.org/10.1007/s10096-017-3158-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3158-6